* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Striatal D2 / D3 Receptor Occupancy, ... and Side Effects with Amisulpride: An Iodine-123-Iodobenzamide SPET Study
Polysubstance dependence wikipedia , lookup
Clinical trial wikipedia , lookup
Pharmacokinetics wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
NMDA receptor wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Toxicodynamics wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Theralizumab wikipedia , lookup
Dydrogesterone wikipedia , lookup
Psychopharmacology wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
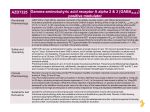
Original Paper 169 Striatal D2/D3 Receptor Occupancy, Clinical Response and Side Effects with Amisulpride: An Iodine-123-Iodobenzamide SPET Study Authors E. M. Meisenzahl1, G. Schmitt1, G. Gründer3, S. Dresel2, T. Frodl1, C. la Fougère2, J. Scheuerecker1, M. Schwarz1, R. Boerner1, J. Stauss2, K. Hahn2, H.-J. Möller1 Affiliations 1 Department of Psychiatry, LMU University of Munich, Munich, Germany Department of Nuclear Medicine, LMU University of Munich, Munich, Germany 3 Department of Psychiatry and Psychotherapy, RWTH Aachen University, Aachen, Germany Abstract & Introduction: Amisulpride appears to be an effective atypical agent for treating schizophrenia in a dose-dependent manner. Methods: 29 patients suffering from schizophrenia or schizoaffective disorder were treated with a broad dose range of amisulpride (50– 1 200 mg/day, mean: 455.2 ± 278.8 mg/day). After 2 weeks, brain single photon emission tomography (SPET) scans were performed two hours after intravenous injection of 185 MBq [123I]IBZM. Clinical evaluations and ratings of extrapyramidal symptoms were performed at baseline and after steady state treatment of two weeks with amisulpride. Introduction & received revised accepted 24.10.2007 30.01.2008 12.02.2008 Bibliography DOI 10.1055/s-2008-1076727 Pharmacopsychiatry 2008; 41: 169–175 © Georg Thieme Verlag KG Stuttgart · New York ISSN 0176-3679 Correspondence E. M. Meisenzahl, MD Department of Psychiatry Ludwig-Maximilians-University of Munich Nussbaumstraße 7 80336 Munich Germany Tel.: + 49/89/5160 24 23 Fax: + 49/89/5160 45 55 [email protected] Amisulpride is a substituted benzamide which has a unique binding and clinical profile, with high affinity for dopamine D2 and D3 receptors but none for D1, D4 and D5 receptors or adrenergic, serotonergic or histaminergic receptor systems. This pharmacological profile means that amisulpride has advantages with regard to side effects, with a lower incidence of hypotension, anticholinergic and sedative effects and EPS [11, 21]. A recent meta-analysis of 18 clinical trials showed that amisulpride is an effective and welltolerated atypical antipsychotic for the treatment of both positive and negative symptoms [8]. Up to now, there are different models about the mechanisms of the atypical action of amisulpride. It may be related to its preferential autoreceptor binding, especially at low doses. Alternatively, its preferential interaction with the limbic dopaminergic system may give it the benefit of atypicality. Amisulpride seems to have a particular affinity for limbic D2 dopamine receptors. Studies in rodents have shown that amisulpride is 2.5-fold more Results: In patients treated with amisulpride, specific binding of [123I]IBZM to D2 receptors was significantly decreased (p < 0.001) compared to healthy controls. D2 receptor blockade correlated well with administered doses and plasma concentrations of amisulpride. Extrapyramidal side effects, which had to be treated with biperiden, were observed in 31 % of the patients. Clinical response was very good, without correlation between the response and striatal D2 occupancy. Discussion: Within the first two weeks of treatment with the atypical antipsychotic amisulpride a significant occupancy of striatal postsynaptic dopamine D2 receptors was achieved. At the same time amisulpride shows an excellent tolerability with good efficacy. potent at inhibiting the binding of 3H-raclopride in the limbic system than in the striatum [17]. Finally, as amisulpride rapidly dissociates from the dopamine D2 receptor, its atypicality may be explained by the fast dissociation hypothesis of atypicality from Seeman and Kapur [6]. Despite the need to clarify the in vivo mechanism of action, up to now only a few investigations have been performed to investigate the striatal and extrastiatal D2 receptor occupancy during amisulpride treatment [2, 4, 9, 20, 22]. As previous studies, due to different dosage regimes and small sample sizes, obtained different results concerning the D2 binding of amisulpride, our present investigation aimed to evaluate by means of SPET the striatal D2/D3 receptor occupancy of a broad range of dosages of amisulpride, between 50 mg and 1 200 mg daily, in a large sample of patients [4]. Beside the obtained D2/D3 bindings [4], another highly relevant objective was to evaluate the clinical response to and possible side effects of amisulpride. An exploratory analysis of the relationship between clinical response and striatal D2/D3 occupancy was performed. Meisenzahl EM et al. Striatal D2/D3 Occupancy, Clinical Response … Pharmacopsychiatry 2008; 41: 169–175 This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited. 2 170 Original Paper The study included consecutively admitted inpatients LMU (19 males, 10 females) from the Department of Psychiatry at the University of Munich, who were suffering from schizophrenia (N = 26) or schizoaffective disorder (N = 3) (DSM IV). Their mean age was 31.7 years (31.7 ± 12.2 years, range: 19–68 years). All patients received continuous monotherapy with amisulpride in a prospective, open study design. Medication was given according the clinical needs and was chosen by the respective attending clinician. Medication remained stable over 14 days. None of the patients was receiving any other concomitant antipsychotic substance, and no depot formulation had been used previously. Permissible concomitant medication was restricted to biperiden, zopiclon and lorazepam. Before the SPET investigation, all patients had been treated with amisulpride in a daily dose between 50 and 1 200 mg/day, with a mean dose of 455.1 ± 278.8 mg/day (6.07 ± 3.94 mg/kg body weight). The last medication was given 12–14 hours before the SPET. Patients pretreated with other antipsychotics underwent a wash-out period from prior treatment of 3 days duration before starting the monotherapy with amisulpride. Eleven of the 29 patients were pretreated with psychotropic medication before the wash-out period (four patients with olanzapine, two with clozapine, two with risperidone, one with perazine, one with paroxetine and one with lorazepam). All others had had no intake of medication for at least 3 months. In 28 of the 29 patients, plasma levels of amisulpride were assessed just before the SPET investigation was performed. The mean plasma concentration was 200 ± 182 ng/mL (range: 26.5–910 ng/mL). According to the diagnostic criteria (DSM IV), 26 patients were diagnosed as suffering from schizophrenia, and 3 from schizoaffective disorder. None of the patients had a second psychiatric disease or any dependency on drugs and alcohol. The assessment of psychopathology was performed at baseline and after 14 days of steady-state treatment using CGI, BPRS, PANSS and SANS scales. The Extrapyramidal Symptom Rating Scale (ESRS) and the Barnes Akathisia Scale (BAS) were used to assess extrapyramidal symptoms after 14 days of steady-state treatment with amisulpride. The response criterion was a reduction of 30 % of the baseline scores of PANSS and SANS. Ethical approval for the SPET investigation was provided by the local ethics committee, all patients had given informed written consent prior to the study. SPET investigation Each subject was injected with 185 MBq [123I]IBZM intravenously 12–14 hours after the last amisulpride intake. Two hours after radiotracer administration, SPET acquisitions were performed over a period of 50 minutes. A Prism 3000 XP triple headed gamma camera (Picker, Cleveland, Ohio) equipped with high resolution fan beam collimators was used for SPET image acquisition. The acquisition parameters included a 20 % energy window centered on 159 keV, a rotational radius of 13 cm or less, 120 projection angles over 360 degrees, and a 128 × 128 matrix with a pixel width of 2.11 mm in the projection domain. The projection images were reconstructed by filtered back projection and filtered by a low pass filter, Chang’s first order method was used for uniform attenuation correction. Images were uniformly re-sliced by drawing a line connecting the anterior-most aspect of the frontal pole to the posterior-most aspect of the occipital pole, which approximates the line connecting the anterior and posterior commissures (AC-PC line). The control group utilized for this study consisted of ten healthy age- and sex-matched subjects (six males, four females, age 32.4 years, range: 22–58 years). In order to assess specific tracer uptake in the striatum, we used the region of interest (ROI) technique. For each patient, data were evaluated in the 2 consecutive transverse slices showing the highest tracer accumulation in the basal ganglia, and then the arithmetic mean of these 2 slices was calculated. Mean specific binding (SB) in the basal ganglia regions was calculated according the following equation: SB = (STR − BKG)/BKG where STR and BKG are the mean counts per pixel in the striatum and frontal cortex as background, respectively. Templates were used to define the striatal ROIs. The size and shape of the templates was established and optimized using the control data. The non-specific background activity was estimated by drawing an ROI around the frontal cortex. Mean specific binding values of a normal control group were used to calculate the striatal dopamine D2 receptor occupancy: D2 occupancy = [(SBcontrol − SBpatient )/SBcontrol ] ×100% Measurement of amisulpride plasma concentrations The detection of amisulpride was performed via an isocratic reversed-phase high-performance liquid chromatography (HPLC) separation and ultraviolet (UV) detection at 280 nm and 195 nm. The HPLC system consisted of a Waters 515 pump, a Waters 717 auto sampler and a Waters 2487 dual wavelength UV detector (Waters, Milford, MA). The chromatographic separation was achieved by using an end-capped C8 reversed-phase HPLC column (Merck, Darmstadt, Germany) connected with a guard column (Merck, Darmstadt, Germany). Benperidole, kindly provided by Bayer Healthcare (Leverkusen, Germany), was used as the internal standard. Amisulpride was kindly provided by SanofiSynthelabo GmbH (Berlin, Germany). A stock solution of the analyte (1 mg/mL) was prepared in methanol and added to human drug-free serum obtained from healthy donors to establish five different calibration concentrations, ranging from 50 to 1000 ng/mL, and three different control sample concentrations (50, 400, 800 ng/mL). The five-point calibration curves were plotted by the peak-high ratios of the analyte/internal standard versus concentrations of the analyte in serum. Regular participation in an external quality control scheme (Health control, Cardiff, UK) guaranteed the specificity of the analysis. Statistical analysis Statistical analyses of SPET measurements and the clinical outcome data of amisulpride-treated patients and controls were performed using one-way analysis of variance (ANOVA). Posthoc tests (Scheffe) were used to test significance of differences. Student’s t-test was performed to compare two independent groups. Equality of variances was tested using Levene’s test of equality of variances. Continuous values were correlated using Pearson correlation coefficients, and discrete values using the Spearmens’s Rho coefficients. Plasma concentrations at time of injection and D2/D3 receptor occupancy values were fit to a one site ligand binding model by Meisenzahl EM et al. Striatal D2/D3 Occupancy, Clinical Response … Pharmacopsychiatry 2008; 41: 169–175 This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited. Patients and Methods & Subjects Original Paper 171 14 days significance steady state age gender dose amisulpride plasma levels weight CGI (0–7) BPRS (0–126) PANSS (0–210) SANS (0–120) EPS parkinsonism dyskinesia dystonia (STR-BKG/BKG) D2 occupancy rate 31.7 ± 12.2 y 19 m/10 f 50–1200 mg 200.3 ± 181.5 ng/mL 73.9 ± 13.5 5.8 ± 0.64 64.4 ± 10.0 105.6 ± 18.2 58.2 ± 16.8 75.3 ± 13.6 4.3 ± 1.02 42.8 ± 11.7 73.9 ± 20.9 48.0 ± 18.2 0.0001 0.0001 0.0001 0.0001 0.03 80 60 40 20 0 0 1.6 ± 3.9 4.7 ± 7.8 0.12 ± 0.5 0.43 ± 0.32 73.3 % ± 13.7 non-linear regression analysis using Sigma Plot, Version 9.0, to the following equation: Occupancy [%] = (Emax ×[C Ami ])/(EC50 +[C Ami ]) where Emax is the maximum attainable receptor occupancy, EC50 is the plasma concentration predicted to provide 50 % of the maximum attainable receptor occupancy and CAmi is the plasma concentration of amisulpride. Data were considered to be significant when p < 0.05. Results & D2/3 receptor binding and amisulpride plasma levels All patients treated with the novel antipsychotic amisulpride showed a reduced striatal IBZM D2 binding in comparison to untreated healthy controls (t = 14. 9, p < 0.0001) (䊉䉴 Table 1). The mean dosage of amisulpride was 455.1 ± 278.8 mg daily. Striatal IBZM binding of the patient group, expressed as [STR–BKG]/ BKG, ranged from 0.0–1.12 (mean 0.43 ± 0.32) versus a mean striatal IBZM binding of 0.95 ± 0.10 (range: 0.78–1.12) for the healthy control group. No differences were found between the treatment group and the comparison group in terms of age (p = 0.62) or gender (p = 0.88). Additionally, no statistical differences emerged between the pretreated patient group (N = 11) and the non-pretreated patient (N = 18) group for any sociodemographic item (age: p = 0.33, weight: p = 0.65) or psychopathological rating at baseline (PANSS: p = 0.84, SANS: p = 0.30, ESRS Parkinsonism: p = 0.17, ESRS dystonia p = 0.20, ESRS dyskinesia: p = 0.98) or striatal D2 receptor occupancy after 14 days of steady state treatment (p = 0.21). In the patient group, individual striatal D2 receptor occupancy ranged from 42 to 100 % with a mean value of 73 ± 14 %. The average occupancy was 42 % for 50 mg (N = 1), 55 % for 100 mg (N = 2), 58 % for 150 mg (N = 1), 71 % for 200 mg (N = 2), 73 % for 300 mg (N = 8), 70 % for 400 mg (N = 3), 81 % for 500 mg (N = 2), 79 % for 600 mg (N = 3), 81 % for 800 mg (N = 6) and 93 % for 1 200 mg (N = 1). When dopamine D2/D3 receptor occupancy and amisulpride daily dose were related to each other according to the law of mass action, the two parameters were highly significantly 200 400 600 800 1000 1200 1400 Amisulpride Daily Dose [mg] Fig. 1 Dopamine D2/D3 receptor occupancy highly significantly correlated with amisulpride plasma concentration at the time of the SPET scan. 100 80 60 40 20 0 0 200 400 600 800 1000 Amisulpride Plasma Level [ng/ml] Emax = 90% EC50 = 30 ng/ml Fig. 2 Dopamine D2/D3 receptor occupancy highly significantly correlated with amisulpride daily dosage at the time of the SPET scan. correlated (R = 0.70; 䊉䉴 Fig. 1), with an Emax value of 87 % (p < 0.0001) and an ED50 of 60 mg (p = 0.0028). The amisulpride plasma concentration was measured in 28 of the 29 patients and showed a mean of 200 ng/mL ± 182 (range: 27–910 ng/mL). There was a significant positive correlation between the amisulpride dose at steady state and amisulpride plasma levels (r = 0.54, p = 0.003). Dopamine D2/D3 receptor occupancy highly significantly correlated with amisulpride plasma concentration at the time of the SPET scan (R = 0.63, 䉴 Fig. 2), with an E 䊉 max value of 90 % (p < 0.0001) and an ED50 value of 30 ng/mL (p = 0.0047) (䊉䉴 Fig. 2). The D2/D3 measurements were checked for possible confounding factors of comedication: the effect of biperiden on D2/D3 binding (p = 0.26) and the effect of the benzodiazepines on D2/D3 binding was not significant (p = 0.19). Side effects: EPS Of the 29 patients, 16 (55.1 %). developed mild extrapyramidal symptoms (EPS). After the treatment with amisulpride, the scores on the ESRS for symptoms of Parkinsonism (scores 0–48) Meisenzahl EM et al. Striatal D2/D3 Occupancy, Clinical Response … Pharmacopsychiatry 2008; 41: 169–175 This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited. Baseline D2/D3 Receptor Occupancy [%] Patients 100 D2/D3 Receptor Occupancy [%] Table 1 Demographic and psychopathological variables of patients at baseline and after 14 days of steady state treatment with amisulpride (mean: 1.6 ± 3.9), dyskinesia (scores: 0–42) (4.7 ± 7.8), dystonia (scores 0–96) (mean: 0.12 ± 0.55) and BAS (scores: 0–14) (mean: 0.86 ± 1.86) appeared quite low. Antiparkinsonian medication (biperiden) was necessary in 9 of the 29 patients (31.0 %). The treatment with biperiden had no influence on the EPS scores after 14 days (ESRS Parkinsonism p = 0.64, ESRS dykinesia p = 0.13, ESRS dystonia p = 0.07). Additionally, 10 patients were treated temporarily with lorazepam. EPS, D2 receptor occupancy and dosage Within the group of patients with EPS, the D2/D3 receptor binding was 77 ± 13 % (range: 51–100 % D2 blockade), which was higher than in those without EPMS, who showed a D2 blockade of 69 ± 13 % (range: 42–86 %). This difference did not reach statistical significance (p = 0.12). There was a significant difference in the daily dosage of amisulpride between the subgroups of patients with (mean dosage 591 mg ± 272) and those without EPS (mean dosage 288 ± 185) (p = 0.002). There was no correlation between the EPS subscales and D2 receptor occupancy (ESRS Parkinson r = 0.003, p = 0.98; ESRS dyskinesia r = − 0.21, p = 0.28; ESRS dystonia r = 0.20, p = 0.29). Clinical efficacy The psychopathology of the patients at baseline was assessed with BPRS (64.4 ± 10. 04), PANSS (105.6 ± 18.2), SANS (58.2 ± 16.8) and CGI (5.8 ± 0.64). After 14 days of steady state treatment, in all three scales there was a significant improvement (PANSS p < 0.0001, PANSS Positive subscale p < 0.0001 and SANS p < 0.001) of psychopathology (䊉䉴 Table 1). Regarding psychopathology, in the comparison between the subgroups of patients treated with lower dosage (LD) of amisulpride (50–300 mg amisulpride/daily) in comparison to the patients treated with higher dosages (HD) (400–1 200 mg amisulpride/ daily), the ratings show that the patients treated with higher dosages had higher scores at the beginning of the study, in all psychopathological items including the productive and the negative symptoms dimensions (CGI HD 6.1 ± 0.7, LD 5.6 ± 0.4; BPRS HD 67.2 ± 8.7; LD 61.5 ± 10.7; PANSS 110.4 ± 15.7, LD 100.5 ± 19.9; SANS HD 63.4 ± 15.0, LD 52.6 ± 17.3) reaching marginal significance for the CGI (p = 0.057). After two weeks of steady state treatment, the distribution of the responders was as follows: PANSS: 14 responders/15 non-responders (response rate 48.3 %), PANSS Positive subscale: 18 responders/11 non-responders (response rate 62.1 %) SANS: 9 responders/20 non-responders (response rate 31 %). No differences regarding clinical improvements between the groups treated with high and low dosages of amisulpride emerged for the PANSS scale (p = 0.60) and the BPRS (p = 0.55) and the SANS (p = 0.07). Response was not influenced by pretreatment with psychotropic medication (PANSS: p = 0.81, PANSS Positive Subscale: p = 0.89, SANS: p = 0.62) or by additional comedication with benzodiazepines (PANSS: p = 0.12, PANSS Positive Subscale: p = 0.11, SANS: p = 0.66) or antiparkinsonian medication (PANSS p = 0.06, PANSS Positive Subscale p = 0.64, SANS p = 0.50). Clinical response and D2 receptor occupancy No differences emerged between the responder and nonresponder (NR) groups on the PANSS scale, with respect to the D2 receptor occupancy (responder group: 73.6 % ± 13. 9 vs. nonresponder 72.9 % ± 14.0, p = 0.89), plasma level of amisulpride (responder group 172.1 ± 95.8 vs. NR 224.7 ± 233.7, p = 0.45) or intake dose per mg daily (responder 410.7 mg/d ± 223.0 vs. NR 496.6 mg/d ± 324.2 , p = 0.41). The same was true for the PANSS Positive Subscale and the D2 receptor occupancy (responder group: 73.7 % ± 14.2 vs. nonresponder 72.4 % ± 13.4, p = 0.80), plasma level of amisulpride (responder group 197.7 ± 120.3 vs. NR 204.4 ± 256.5, p = 0.92), intake dose per mg daily (responder 486.1 mg/d ± 247.2 vs. NR 404.5 mg/d, p = 0.45), and the SANS scale and D2 receptor occupancy (responder group: 68.4 % ± 18.3 vs. non-responder 75.4 % ± 10.9, p = 0.20), plasma level of amisulpride (responder group 173.3 ± 164.4 vs. NR 211.1 ± 190.9, p = 0.62) and intake dose per mg daily (responder 338.8 mg/d ± 236.8 vs. NR 507.5 mg/d ± 285.7 , p = 0.13). In an exploratory analysis, the clinical response after 14 days of steady state treatment and the D2 receptor occupancy of amisulpride was correlated. The clinical improvement was calculated by the following procedure: [PANSSBaseline score– PANSSFollow-up score 14 days]. The value achieved was correlated with the D2/D3 receptor binding and showed no significant correlation with the Spearman’s rho (r = 0.07; p = 0.70). Discussion & We investigated the striatal D2/D3 receptor occupancy of a broad range of dosages of amisulpride between 50 mg and 1 200 mg daily in a large sample of patients with schizophrenia after steady state treatment of 2 weeks. The mean dosage of 455 mg daily of amisulpride achieved a relatively high mean D2/3 receptor binding of 73 % in the striatum. We determined an EC50 value of 30 ng/mL with regard to amisulpride plasma concentration and an EC50 of 60 mg with regard to amisulpride daily dose. D2/D3 binding of amisulpride Amisulpride is an atypical antipsychotic drug with selective affinity for D2/D3 dopamine receptors and thus provides an excellent pharmacological model for testing the hypothesis of atypical action in the CNS. The valid evaluation of in vivo striatal D2/D3 binding is an important piece of the puzzle towards a better understanding of antipsychotic drug action [24]. Our study aimed to contribute to the question of the extent of striatal D2/D3 receptor binding of amisulpride. When comparing the striatal D2/D3 occupancy rates of all studies available [2, 9, 19, 20, 22] including our own results [4], there are marked differences regarding the D2 binding of the drug. A variety of methodological and clinical aspects has to be taken into account when comparing striatal D2 occupancy results of studies. First of all, the usage of different methods such as SPET and PET makes comparison difficult. Additionally, the application of differently affine ligands and the specific modeling applied to the acquired data have to be borne in mind. The time point of data acquisition after the last ingestion of medication is critical, if plasma concentrations of the investigational drug are not available. From a clinical viewpoint, a variety of clinical variables have a notable influence on results, such as the selection of the control group, the drug dosage investigated, the group size and their clinical characteristics with medical pretreatment, age and sex. The duration of drug treatment is probably also a relevant factor. The earliest PET study on the D2 binding of amisulpride was performed with a relatively low mean dose of 205 mg (range: 50–800 mg). The mean striatal D2 binding achieved by use of the ligand [76Br]bromolisuride was 30 % with a range between Meisenzahl EM et al. Striatal D2/D3 Occupancy, Clinical Response … Pharmacopsychiatry 2008; 41: 169–175 This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited. 172 Original Paper 4 and 76 % [9]. The same research group applied the highly affine ligand [76Br]FLB 457 with an only slightly higher mean dosage of 278 mg daily (range: 25–1 200 mg) of amisulpride. In this second investigation, an even lower mean D2 binding of 25 % and a range of 0 to 62 % was detected [22, 23]. In contrast, Vernaleken et al. [20] using PET with [18F]desmethoxyfallypride demonstrated a significantly higher striatal D2/D3 occupancy, with a mean value of 67 % (43–85 %) in the putamen and 76 % (67–90 %) in the caudate [19]. Evident discrepancies between these investigations are the medication ranges administered with the highest doses used in the latter study and the timing of the PET scan relative to the last drug administration. In the study by Vernaleken et al. the timing of the PET scan was close to tmax of amisulpride. However, at comparable amisulpride plasma concentrations, Xiberas et al. [22, 23] report markedly lower striatal D2 receptor occupancies than Vernaleken et al. [20]. The latter authors attribute the overt discrepancy to an underestimation of striatal D2 occupancy in the study by Xiberas et al., because these authors most likely measured striatal binding of their tracer not at equilibrium [15]. The only published SPET study on the D2/D3 binding characteristics of amisulpride in eight patients used [123I]epidepride as the radiotracer [2, 19] [123I]. Epidepride is a high affinity ligand, which allows for the quantification of extrastriatal D2 receptors also. Bressan et al. documented a mean striatal D2 occupancy of 56 % with individual values ranging from 19 to 75 % [2], which seem to be somewhat lower than the values reported here. However, the studies by Bressan et al. [2], Martinot et al. [9], Vernaleken et al. [20], and ours have in common that they report markedly higher striatal D2/D3 receptor occupancies than the study by Xiberas et al. [22, 23]. These four studies consistently show that striatal occupancy increases dose-dependently and that the 80 % EPS threshold is crossed at high plasma concentrations. Our data can be reliably compared with those documented by Bressan et al. [2] and Vernaleken et al. [20], when brain binding data and plasma concentrations are related to each other according to the law of mass action [Martinot et al. [9] did not report plasma concentrations]. The time-course of dopamine D2 receptor occupancy of an antipsychotic is a function of its plasma pharmacokinetics and in vivo affinity. Thus, regardless of the time of the PET scan relative to the last drug administration, the estimated data can be described by a non-linear fit describing a one site saturation. While all three studies reveal an Emax close to total saturation of D2/D3 receptors, the reported EC50 values are somewhat different. Bressan et al. [2] calculated an EC50 of 206 ng/mL for the total striatum from a sample of only six subjects, while Vernaleken et al. [19] in their sample of nine patients found an EC50 of 144 ng/mL for the putamen and 60 ng/mL for the caudate. In our large sample we determined an EC50 of 30 ng/mL. Assuming a “therapeutic window” for antipsychotic drug action between 60 and 80 % striatal D2/D3 receptor occupancy, it can be calculated from our EC50 value that 60 % of the striatal D2/D3 receptors are occupied at an amisulpride plasma concentration of 60 ng/mL, and that the 80 % threshold is passed at 240 ng/mL. Müller et al. in a large sample of 378 patients treated with amisulpride found that the optimal amisulpride plasma concentrations to avoid non-response and EPS were in the range between 100 and 320 ng/mL [13]. Consequently, while the plasma concentrations, which are predicted by means of [123I]IBZM SPET to have the best efficacy/ safety ratio, are somewhat lower than those found in clinical practice, the two available PET studies slightly underestimate the striatal D2/D3 receptor occupancy at the most suitable clinical doses, with the study by Bressan et al. [2] documenting the lowest occupancy values. The most likely explanation for these discrepancies is the different affinity of the used radiotracers, with [123I]epidepride having the highest affinity, making this tracer probably less likely to be sensitive to competition with other ligands. It is noteworthy, that discrepant treatment durations might also influence D2 receptor occupancy as measured with nuclear imaging technology. While we measured D2 blockade after 14 days steady state treatment, Bressan and colleagues studied patients who had been treated between 21 and 348 days. While it is clear that treatment with psychotropic drugs changes receptor availability over time, study of the dynamics of these processes in the human brain has as yet been completely neglected in nuclear imaging. The picture is further complicated by the finding of a regionspecific differential binding of amisulpride. The two imaging studies that evaluated the D2 occupancy of amisulpride in striatal and extrastriatal brain regions showed a significantly higher occupancy of the agent in extrastriatal than in striatal regions [2, 22, 23]. However, while the study by Xiberas et al. [22, 23] has been criticized for its methodological flaws [15, 20], the discrepancy between striatal and extrastriatal binding is much less pronounced in the study by Bressan et al. [2]. Olsson and Farde [15] extensively discussed factors that influence these findings, such as ligand affinity and the different time of binding equilibrium in different brain regions with different D2 receptor density. The time of the scan relative to the last drug administration is only relevant when drug plasma concentrations are not available [3]. Clinical side effects The second aim of the study was to evaluate emerging clinical side effects during the first 14 days of treatment with a large dose range up to 1 200 mg daily of amisulpride. The D2 occupancy rate achieved a mean of 73 % with a maximum D2 occupancy of 100 %. 55 % of the patients experienced EPS, mostly mild in severity. 9 out of 29 patients (31 %) had to be treated with the anticholinergic agent biperiden. Therefore, our data are in accordance with the SPET study by Bressan, who found a favorable extrapyramidal symptom profile after treatment with a mean dose of 406 mg amisulpride daily for 190 days. Based on basic research and in vivo imaging studies, two mechanisms could explain the atypicality of amisulpride; preferential action on limbic D2/D3 receptors and preferential blockade of presynaptic D2/D3 autoreceptors [28]. In addition, the fast dissociation hypothesis can contribute to the explanation of the atypical clinical profile of amisulpride [11, 18]. The patients who experienced extrapyramidal side effects had a range of D2 occupancy between 51.3 and 100 % D2 blockade and a mean of 76.8 %. As the mean value in this subgroup exceeded the threshold for EPS suggested by Farde, whereas the patients without EPS revealed a mean D2 blockade of 68.9 %, statistically our data support the concept of Farde of a certain threshold in D2 occupancy for EPS symptoms. Finally, the correlation between D2 occupancy and EPS rates was not confirmed in our data. This was probably due to the very low rating scores overall with Parkinson symptom scores of 1.6, dyskinesia scores of 4.7 and dystonia scores with 0.12. Meisenzahl EM et al. Striatal D2/D3 Occupancy, Clinical Response … Pharmacopsychiatry 2008; 41: 169–175 This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited. Original Paper 173 One clear limitation in any open trial including ours is that the rater is not blinded for the dosage of the medication. This aspect has to be taken clearly into account. The most frequent primary requirement for atypicality is primarily the low risk of extrapyramidal side effects. Observations from psychopharmacological research define the combined 5HT2/D2 receptor antagonism as the most valid explanation for the atypical profile of antipsychotics. Although the atypical antipsychotic amisulpride is a highly selective D2/D3 receptor antagonist, it has been shown that amisulpride is clearly associated with lower EPS symptoms and with a lower number of drop-outs due to adverse events than conventional antipsychotics [7]. Therefore, our results are in line with the previous findings of a good tolerability of amisulpride. The underlying psychopharmacological mechanism of a low profile of side effects with amisulpride is therefore not due to the combined 5HT2/D2 antagonism as might be the case for other atypical antipsychotics [25]. Given the fact that amisulpride lacks 5-HT2A antagonism, the pharmacological explanation of the clinically well-proven atypicality of amisulpride is of great interest. Clinical response Clinical improvement and therefore efficacy especially in schizophrenia includes a large range of clinical and neurocognitive items [27]. In our design reduction of psychopathological items were in the focus. Clinical response was defined as a 30 % reduction from baseline in the scores of the psychopathological scales applied. This was evaluated for both, the PANSS positive subscale and the SANS. The response quote after 2 weeks of steady state treatment was 62.1 % for the PANSS positive subscale, showing treatment to be effective. The SANS scale showed a response rate of 31 % already within the first 2 weeks. The efficacy of amisulpride was demonstrated by studies comparing the efficacy of amisulpride with that of haloperidol and risperidone [10]. Amisulpride was at least as effective as haloperidol and risperidone in the improvement of positive symptoms, and significantly more efficacious than haloperidol in reducing PANSS negative subscores (P = 0.038) in patients with acute exacerbations. Amisulpride demonstrated a greater improvement in BPRS total scores and PANSS negative subscores than haloperidol after 12 months of treatment in chronic schizophrenic patients with acute exacerbations. In conclusion, amisulpride can thus be considered for use as first-line treatment of acute and chronic schizophrenia [10]. Additionally, recently Assion et al. [26] showed the beneficial effect of augmented amisulpride at a daily dose of 600 mg in patients suffering from chronic schizophrenia and treated by clozapine. Amisulpride was more beneficial in a higher than a lower dosages and no severe side-effects occurred. Augmented amisulpride improved the global outcome of patients suffering from chronic schizophrenia in this pilot study and tended to be a helpful treatment option in cases of partial or non-responsiveness to clozapine. The correlation between clinical response and striatal D2 occupancy rate was evaluated. It is of great interest to investigate how antipsychotic action at a clinical level is correlated to striatal and extrastriatal D2 occupancy rate. Our short intervention study over 14 days was designed carefully with a prospective and steady state treatment for each patient and a strict monotherapeutic regime of amisulpride. The responder criterion with a 30 % reduction of psychopathological scores is quite well accepted. Our open trial revealed no differences between the subgroups of responders and nonresponders regarding striatal D2 occupancy. Up to now, there are very few investigations regarding the correlation of the clinical response and striatal occupancy. However, the general question of how to define remission criteria in schizophrenia is still a large matter of debate [1]. On the other hand, it has to be borne in mind that open trials are limited regarding statements of clinical response. The relationship between D2 occupancy and clinical response was demonstrated by Nordström in a placebo-controlled, double-blind PET trial with the classical neuroleptic raclopride over 2 weeks. The finding was a statistically significant relationship between D2 receptor occupancy and the antipsychotic effect of raclopride compared to placebo [14]. The double-blind PET study by Kapur and colleagues detected a relationship between D2 occupancy and improvement of CGI ratings, however the relationships between D2 occupancy and improvement of PANSS and SANS scores did not achieve significance [5]. In an open trial, Pilowsky and collegues used IBZM SPET to investigate if the striatal D2 occupancy determines response to typical neuroleptics [16]. Their findings suggested that nonresponse to classical antipsychotic medication was not accounted for by different striatal D2 occupancy rates. Although speculative, our results may therefore indicate a different antipsychotic action besides the striatal D2 occupancy rate, as it is hypothesized by the concept of the limbic selectivity of amisulpride. However, it has to be noted that the ligand 123I-IBZM does not provide information on the extrastriatal regions (Tauscher et al. 2002). In summary, the study results confirm that amisulpride is an atypical neuroleptic agent with good efficacy, and good EPS tolerability despite a marked striatal D2 occupancy of 73.3 %. However, the open study design is beyond question a major limitation. The strength of the study is the strict, wide and prospective design with a large range of monotherapeutic steady state treatment dosages of amisulpride over 14 days and a large sample size. Acknowledgements & The investigation was supported by Sanofi-Aventis, Berlin. References 1 Andreasen N, Carpenter WT, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: Proposed Criteria and Rationale Consensus. Am J Psychiat 2005; 162: 441–449 2 Bressan RA, Erlandsson K, Jones HM, Mulligan R, Flanagan RJ, Ell PJ et al. Is regionally selective D2/D3 dopamine occupancy sufficient for atypical antipsychotic effect? An in vivo quantitative [123I]epidepride SPET study of amisulpride-treated patients. Am J Psychiat 2003; 160: 1413–1420 3 Erlandsson K, Bressan RA, Mulligan RS, Ell PJ, Cunningham VJ, Pilowsky LS. Analysis of D2 dopamine receptor occupancy with quantitative SPET using the high-affinity ligand [123I]epidepride: resolving conflicting findings. Neuroimage 2003; 19: 1205–1214 4 Fougere C la, Meisenzahl E, Schmitt G, Stauss J, Frodl T, Tatsch K et al. D2 receptor occupancy during high- and low-dose therapy with the atypical antipsychotic amisulpride: a 123I-iodobenzamide SPECT study. J Nucl Med 2005; 46: 1028–1033 5 Kapur S, Zipursky R, Jones C, Remington G, Houle S. Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiat 2000; 157 (4): 514–520 Meisenzahl EM et al. Striatal D2/D3 Occupancy, Clinical Response … Pharmacopsychiatry 2008; 41: 169–175 This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited. 174 Original Paper 6 Kapur S, Zipursky R, Jones C, Shammi CS, Remington G, Seeman P. A positron emission study of quetiapine in schizophrenia: a preliminary finding of an antipsychotic effect with only transiently high dopamine D2 receptor occupancy. Arch Gen Psychiatry 2000; 57: 553–559 7 Leucht S, Pitschel-Walz G, Engel RR, Kissling W. Amisulpride, an unusual “atypical” antipsychotic: a meta-analysis of randomized controlled trials. Am J Psychiat 2002; 159: 180–190 8 Leucht S, Wahlbeck K, Hamann J, Kissling W. New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet 2003; 361: 1581–1589 9 Martinot JL, Paillere-Martinot ML, Poirier MF, Dao-Castellana MH, Loc’h C, Maziere B. In vivo characteristics of dopamine D2 receptor occupancy by amisulpride in schizophrenia. Psychopharmacology 1996; 124: 154–158 10 Möller HJ. State of the art of drug treatment of schizophrenia and the future position of the novel/atypical antipsychotics. Wld J Biol Psychiat 2000; 1: 204–214 11 Möller HJ. Amisulpride: limbic specificity and the mechanism of antipsychotic atypicality. Prog Neuro-Psychopharmacol Biol Psychiat 2003; 27: 1101–1111 12 Möller HJ. Antipsychotic and antidepressive effects of second generation antipsychotics: two different pharmacological mechanisms? Eur Arch Psychiat Clin Neurosci 2005; 255: 190–201 13 Müller MJ, Wetzel H, Eich FX, Rein W, Puech A, Benkert O, Amisulpride Study Group. Dose-related effects of amisulpride on five dimensions of psychopathology in patients with acute exacerbation of schizophrenia. J Clin Psychopharmacol 2002; 22: 554–560 14 Nordstrom AL, Farde L, Wiesel FA, Forslund K, Pauli S, Halldin C et al. Central D2-dopamine receptor occupancy in relation to antipsychotic drug effects: a double-blind PET study of schizophrenic patients. Biol Psychiat 1993; 33: 227–235 15 Olsson H, Farde L. Potentials and pitfalls using high affinity radioligands in PET and SPET determinations on regional drug induced D2 receptor occupancy – a simulation study based on experimental data. Neuroimage 2001; 14: 936–945 16 Pilowsky LS, Costa DC, Ell PJ, Murray RM, Verhoeff NP, Kerwin RW. Antipsychotic medication, D2 dopamine receptor blockade and clinical response: a 123I IBZM SPET (single photon emission tomography) study. Psycholog Med 1993; 23: 791–797 17 Scatton B, Claustre Y, Cudennec A, Oblin A, Perrault G, Sanger DJ et al. Amisulpride: from animal pharmacology to therapeutic action. Int Clin Psychopharmacol 1997; 12: 29–36 18 Seeman P. Atypical antipsychotics: mechanism of action. Can J Psychiat 2002; 47: 27–38 19 Stone JM, Bressan RA, Erlandsson K, Ell PJ, Pilowsky LS. Non-uniform blockade of intrastriatal D2/D3 receptors by risperidone and amisulpride. Psychopharmacology 2005; 180: 664–669 20 Vernaleken I, Siessmeier T, Buchholz HG, Hartter S, Hiemke C, Stoeter P et al. High striatal occupancy of D2-like dopamine receptors by amisulpride in the brain of patients with schizophrenia. Int J Neuropsychopharmacol 2004; 7: 421–430 21 Wetzel H, Gründer G, Hillert A, Philipp M, Gattaz WF, Sauer H et al. Amisulpride versus flupentixol in schizophrenia with predominantly positive symptomatology – a double-blind controlled study comparing a selective D2-like antagonist to a mixed D1-/D2-like antagonist. The Amisulpride Study Group. Psychopharmacology 1998; 137: 223–232 22 Xiberas X, Martinot JL, Mallet L, Artiges E, Canal M, Loc’h C et al. In vivo extrastriatal and striatal D2 dopamine receptor blockade by amisulpride in schizophrenia. J Clin Psychopharmacol 2001; 21: 207–214 23 Xiberas X, Martinot JL, Mallet L, Artiges E, Loc’H C, Maziere B et al. Extrastriatal and striatal D(2) dopamine receptor blockade with haloperidol or new antipsychotic drugs in patients with schizophrenia. Br J Psychiat 2001; 179: 503–508 24 Leuner K, Müller WE. Dopamine in the prefrontal cortex and its different modulation by conventional and atypical antipsychotics. Pharmacopsychiatry 2007; 40: 17–33 25 Pietro NC, Seamans JK. Dopamine and serotonin interactions in the prefrontal cortex: insights on antipsychotic drugs and their mechanisms of action. Pharmacopsychiatry 2007; 40: 27–33 26 Assion HJ, Reinbold H, Lemanski S, Basilowski M, Juckel G. Amisulpride augmentation in patients with schizophrenia partially responsive or unresponsive to clozapine. A randomized, double-blind, placebo-controlled trial. Pharmacopsychiatry 2008; 41: 24–28 27 Meisenzahl EM, Scheuerecker J, Schmitt GJS, Möller HJ. Dopamine, prefrontal cortex and working memory in schizophrenia. Pharmacopsychiatry 2007; 40 (Suppl): 62–72 28 Sokoloff P, Diaz J, Foll B Le, Guillin O, Leriche L, Bezard E, Gross C. The dopamine D3 receptor: a therapeutic target for the treatment of neuropsychiatric disorders. CNS Neurolog Disord – Drug Targets 2006; 5: 25–43 Meisenzahl EM et al. Striatal D2/D3 Occupancy, Clinical Response … Pharmacopsychiatry 2008; 41: 169–175 This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited. Original Paper 175