* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Anti- muscarinic agents
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Discovery and development of TRPV1 antagonists wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
CCR5 receptor antagonist wikipedia , lookup
Drug interaction wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
NMDA receptor wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
Toxicodynamics wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Neuropharmacology wikipedia , lookup
Nicotinic agonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
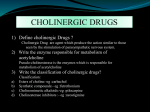
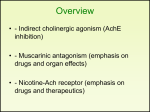
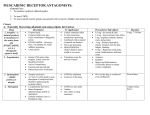
Cholinergic antagonists Samuel Aguazim ( MD) What are cholinergic antagonists? • Drugs that bind to cholinergic receptors ( muscarinic and/or nicotinic), but do not trigger the usual intracellular response. The antagonize the effects of acetylcholine Name 3 subclasses of cholinergic antagonists. • 1. Muscarinic blockers • 2. Neuromuscular blocking agents- inhibit the efferent impulses to skeletal muscle via the nicotinic muscle receptor (Nm) • 3. Ganglionic blockers- inhibit the nicotinic neuronal receptor (Nn) of both parasympathetic and sympathetic ganglia Muscarinic antagonists • • • • • • • Give six examples of muscarinic blockers 1. atropine 2. scopolamine 3. homatopine 4. cyclopentolate 5. tropicamide 6. pirenzepine Anti- muscarinic agents • • • • sites of action 1. Secretions by salivary, bronchial and sweat glands. 2. The eye and cardiac responses mediated by the vagus. 3. Urinary bladder and GI tract. 4. Gastric secretions. • Note: All of the muscarinic antagonists are competitive antagonists for the binding of acetylcholine to the muscarinic receptor Naturally occurring • Atropine ( belladonna ) • Scopolamine • Homatropine The effect and side effects of these drugs are the opposite of the drugs considered in the previous chapter • • • • • Eye: Mydriasis, cyclopedia ( blurred vision) Skin : Reduced sweating, flushing GI: Reduced motility and secretions CVS: Increased Heart Rate ( High Doses) Respiratory: Bronchial Dilation and decreased secretion • GU: Urinary retention • CNS: drowsiness, hallucinations, coma • ATROPINE – high affinity for muscarinic receptors. acts both centrally and peripherally • It causes reversible, nonselective blockade of muscarinic receptors. • Mydriasis, cycloplegia. • Eneuresis in children • Low doses- bradycardia. • High doses—tachycardia • Dilates cutaneous vasculature • • • • • Atropine uses In ophthalmology –mydriatic/ cycloplegic Spastic disorders of GI and lower urinary tract. To treat Organophosphate poisoning To suppress respiratory secretions prior to surgery. Synthetic quaternary ammonium antimuscarinic agents. • Ipratropium • Propantheline Synthetic tertiary amine muscarinic antagonists • Cyclopentolate • Tropicamide • Dicyclomine • Pirenzipine CNS • Due to its greater lipid solubility, scopolamine has significant CNS effects even at low therapeutic doses. • An adjunct for anesthesia due to an ability to decrease short term memory. • Motion sickness (scopolamine) • Antipsychotic therapy: used to treat the extrapyramidal symptoms Eye • Mydriasis • Refract the eye during ophthalmic examinations. • Caution : glaucoma Heart • Low doses initially produce bradycardia, but later doses produce tachycardia. • Some times in Surgery/catheterization Lung • Broncho -dilation: Ipratropium • Mainly used as inhalation in treating asthma and COPD. • Atropine prior to surgery will decrease the respiratory secretions GI tract • Salivary secretions decrease • Can cause dry mouth and difficulty in swallowing • Only Pirenzepine has some potency to decrease hyperacidity.. Other uses • With an opioid to relax the ureter in renal colic. • To increase the capacity and decrease the frequency of bladder contractions, i.e. enuresis in children. • To decrease the frequency of urination in spastic paraplegia. Toxic effects • • • • • • • • • decreased concentration and memory drowsiness sedation excitation ataxia asynergia disorientation hallucinations coma ATROPINE PSYCHOSIS • Disorientation, confusion, recent loss of memory, agitation, incoherent speech, restlessness, hallucinations, anxiety and delirium. • Treatment – symptomatic only and discontinue the drug immediately. Therapeutic uses of muscarinic antagonists • 1. Premedication • · Atropine • · Given before operations to prevent unwanted M stimulation. • · Want to eliminate bronchial secretions (don't want the patient to choke on their own secretions) • · Want to block vagal stimulation to the heart and lungs (want to keep airways open) • · During induction of anesthesia, there may be excessive vagal stimulation, which we want to eliminate. • Anticholinesterase toxicity • Toxicity due to over dose of physostigmine and other anticholinesterases • Atropine is used to treat this condition by blocking all M receptors. • • • • • • • • 2. Antispasmodic · Hyoscine N butyl Bromide · A quaternary derivative · Treats colic 3. Bronchodilator (asthma) · Ipratropium · A quaternary derivative · Given by inhalation, get a local effect • Homatropine • · Much shorter action than atropine • · It is the drug of choice when doing investigations of the eye, since it dilates the pupil for a short time only. • • • • 4.Treatment of peptic ulcers · Pirenzepine · Selective M1 antagonist · Not as good as H2 antagonists (e.g. cimetidine) or proton pump inhibitors (e.g. omeprazole) • 5. Parkinson's disease • · Benztropine, trihexiphenidyl also used to treat the extrapyramidal symptoms due to Antipsychotic drugs • 6. Motion sickness · Hyoscine, scopolamine ADVERSE EFFECT OF ATROPINE • DRY MOUTH • INHIBITION OF SWEATING ESPECIALLY IN YOUNG CHILDREN • TACHYCARDIA AND CUTANEOUS VASODILATION • BLURRING OF VISION • HALLUCINATIONS AND DELIRIUM MUSCARINIC EFFECTS • • • • • • • REMEMBER S --- salivation L --- lacrimation U --- urination D --- diaphoresis G --- GI E --- Eye & emesis GANGLIONIC BLOCKERS • • • • NICOTINE TRIMETHAPHAN MECAMYLAMINE Ganglionic blockers work by interfering with the postsynaptic action of acetylcholine. They block the action of acetylcholine at the nicotinic receptor of all autonomic ganglia. These drugs are very rarely used clinically SITE OF ACTION • ALL NICOTINIC RECEPTORS • IN ANS ( BOTH SNS AND PNS ) • IN CNS NICOTINE DOSAGE GANGLION • LOW DOSE • STIMULATION • HIGH DOSE • BLOCK CNS/ NICOTINE • LOW DOSE- EUPHORIA,RELAXATION • HIGH DOSEcentral respiratory paralysis hypotension- medullary paralysis PERIPHERAL EFFECTS • • • • COMPLEX HR RAISES B.P.- RAISES GIT- MOTILITY RAISES OTHERS • TRIMETHAPHAN- SHORT ACTING • HTN EMERGENCIES • used in surgery, particularly neurosurgery, to produce a relatively bloodless operative field (controlled hypotension). • MECAMYLAMINE- LONG ACTING CHR. CASES of HTN Neuromuscular Blocking Drugs They block the effects of acetylcholine by interacting with nicotinic receptor. Mainly during surgery to produce complete muscle relaxation, without giving higher anesthetic doses. Neuro muscular blocking drugs • • • • • • • • Atracurium Doxacurium Mivacurium Pancuronium Rocuronium Succinylcholine Tubocurarine Vecuronium Atracurium • safe in renal failure, used in critically ill patients for mechanical ventilation. • Short duration of action – so suitable for short surgical procedures. Rocuronium & Succinylcholine • Rapid onset of action – so used mainly in tracheal intubation in patients with gastric contents. Vecuronium – short duration of action , so used in short surgical procedures. Imp side effects • Tubocurarine – induce histamine release and also lower B.P. • Pancuronium – Increased H.R. • Succinylcholine – malignant hyperthermia, hyperkalemia and increased Intraocular pressure.