* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Histamine - heartha..
Discovery and development of proton pump inhibitors wikipedia , lookup
Drug interaction wikipedia , lookup
CCR5 receptor antagonist wikipedia , lookup
Discovery and development of TRPV1 antagonists wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
NMDA receptor wikipedia , lookup
Toxicodynamics wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Neuropharmacology wikipedia , lookup
Psychopharmacology wikipedia , lookup
Histamine
Introduction
Autacoids is a general term that refers to a number of compounds such as: histamine, serotonin, endogenous
peptides, prostaglandins, and leukotrienes
o The formal definition of autacoids is "self-remedy, referring to the action of local hormones
Chemistry and Pharmacokinetics
o The formation of histamine occurs by the removal of a carboxyl group (decarboxylation) from amino acid
L-histidine
o One of the important issues associated with formation of a biologically active compound is the mechanism
that accounts for the compounds inactivation.
Histamine is active biologically, but the first step for its inactivation involves the addition of a
methyl group (CH3) followed by a chemical oxidation.
o Most of the time very little histamine is excreted unchanged because of these metabolic steps. One
exception would be the case of neoplastic disease (cancer). For instance, significant histamine is excreted
unchanged in the presence of these diseases: (a) systemic mastocytosis, (b) gastric carcinoid syndrome
or (c) urticaria pigmentosa.
Tissue Distribution:
o The primary site for histamine localization is the mast cell granules (or basophils)
Mast cells are important in that they release histamine in response to potential tissue injury
Other sites include the central nervous system where histamine may function as a
neurotransmitter and the fundus of the stomach (enterochromaffin-like cells) which are major
acid secretagogues [They promotes accretion by activation of acid-producing mucosal parietal
cells]
Histamine: Storage and Release
o Immunologic Release: The most important mechanism for histamine release is in response to an
immunological stimulus. In
Mast cells, if sensitized by surface IgE antibodies, degranulate when exposed specific antigen.
Degranulation means liberation of the contents of the mast cell granules, including histamine.
Degranulation is involved in the immediate (type I) allergic reaction.
Release regulation is present in most mast cells.
Histamine Modulation is associated with the inflammatory responses. Following local injury,
histamine first produces a local vasodilation (reddening of the area) followed by an the release of
acute inflammation mediators. Inflammatory cells are involved in this process and include
neutrophils, eosinophils, basophils, monocytes & lymphocytes. In
o
Mechanical/Chemical Release: A second type of release occurs following chemical or mechanical injury
to mast cells. In these injuries caused degranulation as noted above including again histamine release.
Common drugs such as morphine or tubocurarine can displace histamine from granule storage sites.
o
Pharmacodynamics-- Mechanism of Action -- Histamine mediates its effects by interacting with
receptors.
Receptor Subtype
Localization
Receptor coupling
Antagonists (partially
selective)
H1
Endothelium, brain,
smooth muscle
receptor activation
causes and increased IP3,
DAG (diacylglycerol)
production
N/A
H2
mass and cells, gastric
mucosa, cardiac muscle,
brain
receptor activation
causes an increase in
cAMP production
ranitidine (Zantac),
cimetidine (Tagamet)
H3
presynaptic: brain,
mesenteric plexus (other
neurons)
G protein coupled
N/A
Receptor subtypes --H1, H2, and H3:
o intracellular G protein interactions
H1:endothelial and smooth muscle cell localization
o H1 receptor activation causes can increase in phosphoinositol hydrolysis and an increase in
intracellular calcium.
H2 gastric mucosa, cardiac muscle cells, immune cell localization:
o H2 receptor activation causes an increase in cyclic AMP.
H3: primarily presynaptic
o activation causes a decrease in transmitter release {transmitters: histamine,acetylcholine,
norepinephrine, serotonin)
Organ System Effects: Histamine
Cardiovascular:
o Systolic and diastolic blood pressure: Vasodilation of arterioles and precapillary sphincters account for
histamine's vasodilating effects. Vasodilation may be due in part to nitric oxide liberation.
o Following from the reduced blood pressure, the heart rate increases by autonomic reflex mechanisms and
by direct action.
o Both H1 and H2 receptors involved in cardiovascular responses.
o Histamine-associated edema:H1 receptor effects (postcapillary vessels)
increase in vessel permeability due to separation of endothelial cells, allowing transudation of
fluid and molecules as large as small proteins.
responsible for urticaria (hives)
endothelial cell separation: secondary to histamine-induced calcium influx causing
intracellular actin/myosin-mediated contraction
o Direct cardiac effects:
1. increased contractility (positive inotropism)
2. increased pacemaker rate (positive chronotropism)
Gastrointestinal tract: Histamine promotes intestinal smooth muscle contraction which is an H 1 receptor
mediated effect
Bronchiolar smooth muscle activation by histamine causes bronchodilation (H1 receptor mediated )
o It is not surprising that inhaled histamine is a diagnostic, provocative test for bronchial hyperreactivity
(asthma or cystic fibrosis)
Nerve Endings: Sensory nerve endings are stimulated by histamine, especially those endings which mediate
pain and itching.
o These effects are H1 receptor mediated effect and represent part of the local reaction to insect stings
(urticarial responses)
Secretory tissue:
o Histamine cause the stimulation of release by secretory tissues. For example, a significant increase in
gastric acid secretion is caused by histamine. Other examples of increased release include gastric pepsin.
o Mechanism of Action: Considering the gastric parietal cells, histamine interacts with H 2 receptors and
initiates a second messenger response which proceeds by (1.) Increasing adenylyl cyclase activity which
(2.) Results in an increase in the second messenger, cyclic AMP which (3.) Causes an increase in
intracellular calcium levels. The increase in calcium triggers release. This releasing characteristic of
calcium applies broadly in physiology.
Histamine:Clinical Pharmacology-- uses
o
Pulmonary Function: histamine aerosol may be used to test for bronchial hyperreactivity.
Toxicities include:
o
Flushing, hypotension, tachycardia, headache, bronchoconstriction, gastrointestinal disturbances
Should not be given to asthmatics (except with extreme caution in pulmonary function testing)
Should not be given to patients with active ulcer disease or gastrointestinal hemorrhage.
Histamine Antagonists Introduction:
o physiologic antagonists: example -- epinephrine, agents that produce opposing effects, acting and
different receptors
o release inhibitors: reduced mast cell degranulation: example: cromolyn and nedocromil
o receptor antagonists: selective blockade of histamine receptors (H 1, H2, H3 types)
H1 receptor antagonists:
o General properties:
H1 antagonists include both first-generation and second-generation compounds
Both categories of agents are orally active and are metabolized by the liver using the
cytochrome P450 drug-metabolizing system
The average duration of pharmacological action is about 4-6 hours
Meclizine (Antivert) and several second-generation drugs far longer acting, with
effects lasting 12-24 hours.
First-generation agents tend to be relatively more sedating and more likely than secondgeneration drugs to block autonomic receptors -- for example antimuscarinic effects [blockade
of cholinergic, muscarinic-type receptors]
Second-generation agents are relatively less sedating compared to the earlier first-generation
agents and exhibit less CNS penetration, which accounts for reduced sedation. Some of the
second-generation agents are metabolized by a cytochrome P450 type that is inhibited by other
drugs, such as the antifungal agent ketoconazole (Nizoral). Therefore, plasma concentrations of
certain second generation H1 antagonists may increase, even the toxic levels, if the patients also
taking drugs such as ketoconazole (Nizoral) or erythromycin estolate (Ilosone).
Histamine Pharmacodynamics:
o Histamine H1 Receptor Blockade:
H1 receptor blockers exhibit competitive antagonism for H1 receptor sites whereas little effects at
H2 receptor sites and negligible effects of H3 sites are observed.
H1 receptor blockers prevent bronchiolar or gastrointestinal smooth muscle constriction
H1 receptor blockers do not completely prevent cardiovascular effects (some of these effects are
mediated by H2 receptors)
H1 receptor blockers cannot affect increases in gastric acid secretion or mast cell histamine
release because these effects are H2 receptor site-mediated.
H1
H2
Receptor Type: Sites of Action
endothelium, brain, smooth muscle
mast cells, gastric mucosa, cardiac muscle, brain
Histamine Pharmacodynamics continued: Some important histamine promoted effects occur not true
histamine's interaction with histamine receptors but by histamine interaction with other receptors. Many of
these interactions are responsible for "side effects" associated with antihistamines medications. One
prominent example is the side effect of sedation. The side effect is the basis for antihistamine use as a sleep
aid.
o Non-Histamine Receptor-Mediated Effects
First-generation H1 receptor blockers cause effects mediated by many other receptor systems.
These other effects in the mediated by muscarinic cholinergic receptors, alpha adrenergic
receptors, serotonergic receptors and local anesthetic receptor sites.
Sedation: Sedation is a common side effect of first-generation H1 antagonists and provided the
rationale for these agents to be used has sleep-aids, i.e. hypnotics. These agents may produce a
paradoxical excitement and children and toxic reactions can include stimulation, agitation, or
even coma. The newer H1 antagonists, by contrast, cause minimal or no sedation.
Anti-emetic/Antinausea: Some first-generation H1 antagonists prevent motion sickness. In this
application these agent should be used as prophylaxis. Therefore they should be taken well in
advance of the activity which might be expected to induce motion-sickness.
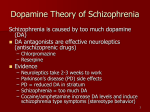
Anti-Parkinsonism: Certain first-generation H1 antagonists, because of their antimuscarinic
properties, turn out to be effective in suppressing Parkinsonian symptoms which are side-effects of
some antipsychotic medications. The antipsychotic drugs involved here tend to be "first-
generation" agents which have numerous neurological side effects. The side effects are much less
prevalent with newer antipsychotic drugs, such as olanzapine (Zyprexa) or risperidone (Risperdal).
Anticholinergic effects: Some first-generation H1 antagonists have strong antimuscarinic actions
(atropine-like effects). Prominent anticholinergic effects include blurred vision (loss of
accommodation) and urinary retention. Therefore patients who may have benign prostatic
hypertrophy may exhibit significant worsening of their clinical state due to antimuscarinic effects.
Probably benign prostatic hypertrophy would be one example of the syndrome for which there
would be a relative contraindications for these drugs.
Alpha adrenergic blocking effects: Some first-generation H1 antagonists block alpha adrenergic
receptors. Alpha-adrenergic receptor blockade can cause orthostatic (postural) hypotension.
Serotonergic blockade: Some first-generation H1 antagonists block serotonin receptors
Local Anesthetic effects:
Many first-generation H1 antagonists are local anesthetics, exhibiting sodium channel
blockade [similar in general to that caused by procaine (Novocain) and lidocaine
(Xylocaine)].
For example, diphenhydramine (Benadryl) and promethazine (Pherergan) are more potent
than procaine (Novocain) as a local anesthetic
Clinical Uses: H1 Histamine Receptor Blockers
Allergic Reactions:
o The pharmacological objective in the use of these medications is to treat or prevent symptoms of
allergic reaction.
o H1 histamine receptor blockers are drugs of choice to treat allergic rhinitis and urticaria. In both
cases, histamine is the primary mediator of the symptoms
o By contrast, in asthma their multiple mediators and H1 histamine receptor blockers are ineffective.
o Angioedema (hives) may be initiated by histamine but are maintained by bradykinins. In this clinical
setting H1 histamine receptor blockers are also ineffective.
o For atopic dermatitis, diphenhydramine which is a H1 histamine receptor blocker proves effective in
control of itching and for sedation.
o For allergic conditions, an example being hay fever, the H1 histamine receptor blockers are effective for
symptomatic relief. The goal is to minimize sedating effects while retaining beneficial symptomatic relief.
o The Second-generation H1 histamine receptor blockers, for example terfenadine (Seldane) or astemizole
(Hismanal) are beneficial because they exhibit minimal sedation while being effective in management of
allergic rhinitis and chronic urticaria. At present, these medications tend to be more expensive than
first-generation histamine receptor H1 antagonists.
Allergic Rhinitis
H1 antihistamines are effective for treating nasopharyngeal itching, sneezing, watery rhinorrhea,
and ocular itching, tearing, erythema.
o
Side effects associated with older H1 antihistamines include sedation, visual disturbance,
urinary retention, and arrhythmias
Newer H1 antihistamines:( terfenadine (Seldane) astemizole (Hismanal))
o These agents exhibit less sedation associated with their reduced ability to cross the blood
brain barrier.
o However, there are very important drug-drug interactions associated with this category.
For example, macrolide antibiotics such as erythromycin, clarithromycin (Biaxin),
ketoconazole-class broad-spectrum antifungal drugs, inhibit terfenadine (Seldane) or
astemizole (Hismanal) metabolism.
Toxic levels of terfenadine (Seldane) or astemizole (Hismanal) may induce
potentially fatal cardiac arrhythmias.
These new H1 antihistamines are contraindicated for concurrent use with macrolide
antibiotics and ketoconazole-class and fungal drugs or in the presence of impaired
hepatic function or inpatients predisposed to arrhythmias.
Topical alpha-adrenergic agonists:
o Phenylephrine (Neo-Synephrine) or oxymetazoline (Afrin) reduce nasal
congestion/obstruction.
Efficacy duration: limited due to rebound rhinitis and systemic effects which may
include insomnia, irritability, and hypertension -- the latter which is seen more
commonly with oral alpha adrenergic agonists.
Oral alpha-adrenergic agonists may be useful in diminishing antihistamine-mediated sedation
while improving antihistamine efficacy in relieving congestion. However, there is a concern that
these agents due to their potentially hypertensive effects, may precipitate adverse cardiovascular
effects, such as stroke. Recently, there has been an effort to remove such "pressor" agents from
common over-the-counter cold medications.
Cromolyn sodium: This agent is a liquid provided as a nasal metered-does spray. Cromolyn sodium
(Intal) is not associated with side effects and typically is used prophylactically to reduce episodic
allergen nasal mast cell activation. This agent may be used as part of a anti-asthma drug regimen.
Intranasal glucocorticoids:
o Intranasal glucocorticoids are the most potent drugs available for management of
established rhinitis (seasonal or perennial) and including vasomotor rhinitis
Topical-to-systemic activity greater for: flunisolide (AeroBid) or budesonide
(Rhinocort), compared to beclomethasone (Banceril) or triamcinolone (Aristocort).
o Despite the different route of administration, intranasal-administered glucocorticoids exhibit
the same efficacy but with reduced systemic side effects compared to same agent
administered orally.
o Side effects include local irritation, which is the most frequent side effect to Candida overgrowth which is an unusual side effect
o Topical high potency glucocorticoids exhibit superior efficacy compared antihistamines during
pollen season.
Immunotherapy (hyposensitization): This approach is based on repeated, subcutaneous injections of
gradually increasing allergen (specific for the symptom complex) over a period of 3-5 years.
o Contraindications include significant cardiovascular disease and unstable angina
o Cautious use applies to patients receiving beta adrenergic blockers (due to difficulty in
managing possible anaphylactoid responses to treatment)
o Clinical Management Sequence:
1. Identification of allergens confirmed by allergens-specific IgE skin testing and/or
serum assay.
2. Avoidance of offending allergen
3. Mild symptoms: prophylaxis with topical cromolyn sodium or single (bedtime) dose of
chlorpheniramine (Chlor-Trimeton) or astemizole (Hismanal) or terfenadine (Seldane)
(decision based on side effects and presence of other concurrent medications or
disease.
4. Prominent symptoms: Topical beclomethasone (Banceril) or if needed budesonide
(Rhinocort) or flunisolide (AeroBid)
5. Management failure: immunotherapy
Clinical Uses: H1 Histamine Receptor Blockers continued
Motion Sickness:
o Scopolamine and certain first-generation H1 blockers are among the most effective drugs for motion
sickness prevention
o Diphenhydramine and promethazine are the H1 blockers with the greatest effectiveness
o Cyclizine (Marezine) and meclizine are also effective agents and are less sedating than those above.
Nausea and Vomiting (Pregnancy)
o
H1 blockers are not recommended for use in management of nausea and vomiting associate with
pregnancy because:
Difficulty in assessment of possible birth defects associated with certain H 1 (benedictin)
antagonists and known teratogenic effects of others (e.g., doxylamine) in animal models.
H1 blockers: Toxicity
o
Uncommon toxic effects following systemic demonstration:
excessive excitation and convulsions in children
orthostatic (postural) hypotension
Allergic responses
o Drug allergy -- relatively common, following topical use of H1 antagonists
o First-generation overdosage: similar to atropine overdosage
o
Second-generation overdosage: may induce cardiac arrhythmias
Drug-Drug Interactions
Second-generation H1 blockers:
o
Myocardial toxicity:
Toxicity follows combination of terfenadine or astemizole combined with ketoconazole (Nizoral),
itraconazole (Sporanox), or macrolide antibiotics (e.g.,erythromycin) because Q-T (ECG) prolongation
Ventricular arrhythmias which may be potentially fatal.
Terfenadine (Seldane)/astemizole (Hismanal) are contraindicated in patients taking ketoconazole
(Nizoral), itraconazole (Sporanox), macrolide antibiotics, and patients with diminished liver
function.
patients taking ketoconazole (Nizoral), itraconazole (Sporanox), macrolide antibiotics, and
patients with diminished
Fexofenadine (Allegra), a metabolite of terfenadine (Seldane), is safer.
H2 Receptor Antagonists
Introduction-- overview
o H2 receptor antagonists inhibit histamine-induced stomach acid secretion
o Interest in these drugs: based on the high incidence of peptic ulcer disease (and related gastrointestinal
disease)
o H2 receptor antagonists: frequently prescribed, available as over-the-counter preparations in some dosage
forms.
Pharmacology of H2 receptor blockers:
H2 receptor blocker
Mechanism of Elimination
Cimetidine (Tagamet)
Mainly renal
Ranitidine (Zantac)
Mainly renal
Famotidine (Pepcid)
Mainly renal
Nizatidine (Axid)
Mainly renal
Pharmacodynamics: H2 Receptor Antagonists
Mechanism of action: H2 Receptor Antagonists involves selective competitive antagonism at H2 receptor sites.
Effects on organ systems
o Acid secretion and gastric motility
The most important action is a reduction in gastric acid secretion due to H 2 receptor blockade.
Blockade of gastric acid secretion in the presence of H2 receptor blockade following histamine,
gastrin, cholinomimetics (acetylcholine-like drugs such as bethanechol (Urecholine)) and vagal
stimulation.
Reduced gastric acid volume
Decreased pepsin concentration
o Other effects: unrelated to H2 receptor blockade
Cimetadine (to lesser degree ranitidine; not famotidine or nizatidine): inhibits cytochrome P450
microsomal drug metabolizing system
Cimetadine and ranitidine inhibit renal clearance of basic drugs that use renal secretory transport
systems
Cimetadine, by binding to androgen receptors, produce antiandrogen effects
Clinical Uses: H2 Receptor Antagonists
Peptic Ulcer Duodenal Disease:
o H2 receptor antagonists (low toxicity) by reducing gastric acidity has significantly advanced treatment of
peptic ulcer disease
Other agents that reduce gastric acid include:
1. antimuscarinic drugs (at high dosages required, side effects are significant)
2. antacids which require frequent dosing and may be associated therefore with poor
patient compliance
3. Omeprazole (Prilosec) and lansoprazole (Prevacid) (proton pump blockers and) are very
effective in reducing gastric acid by directly inhibiting an enzyme-pump which produce
hydrogen ions (protons) in the stomach thus decreasing pH
Sucralfate (Carafate) (a coating agent) promotes healing
Antibiotics are prominent in current therapy because of the importance of H. pylori in gastric
ulcer disease.
Gastric Ulcer:
o H2 receptor antagonists reduce symptoms and promote healing for benign gastric ulcers
Gastroesophageal Reflux Disorder (erosive esophagitis)
o H2 receptor antagonists, at higher dosages than for management of peptic or gastric ulcer disease,are used
as one component of treatment. Proton pump blockers (e.g. omeprazole) are usually also administered.
Hypersecretory Disease:
o
Zollinger-Ellison syndrome is associated with acid hypersecretion which is caused by gastrin-secreting
tumor. This disorder is often fatal; however, H2 receptor antagonists often control symptoms.
o
Systemic mastocytosis and multiple endocrine adenomas are hypersecretory conditions in which H 2
receptor antagonists often control symptoms.
Toxicity:H2 receptor antagonists:
o Overview: these agents are generally well tolerated. The most common side effects include diarrhea,
dizziness, somnolence, headache and rash.
Cimetidine (Tagamet) has the most adverse effects whereas, nizatidine (Axid) has the fewest
adverse effects.
o CNS effects are uncommon. However, in the elderly confusional of states, delirium, and slurred speech
may occur. These effects are often associate with cimetidine (Tagamet) and are unusual with ranitidine
(Zantac).
o Endocrine effects are also relatively uncommon. However cimetidine (Tagamet) does exhibit
antiantherogenic effects because the drug blinds to androgen receptors and therefore can cause
gynecomastia (men) and galactorrhea (women).
Endocrine effects not associated with famotidine, ranitidine, nizatidine
o Other uncommon side effects include blood dyscrasias [cimetidine (Tagamet): granulocytopenia,
thrombocytopenia, neutropenia, aplastic anemia which is extremely rare], hepatotoxicity with reversible
cholestatic effects, reversible hepatitis, liver enzyme test abnormalities.
o Use in pregnancy:
Harmful effects on the fetus have not been observed when H 2 blockers are prescribed to pregnant
women even though H2 blockers are secreted into breast milk and may affect nursing infants.
The general rule, however is that since these drugs across the placenta, they should only
be prescribed when absolutely required.
Since these drugs to cross the placenta, the drugs should only be prescribed when
absolutely required.
Drug-drug Interactions:
o Cimetidine (Tagamet) is the prominent agent in this category for drug-drug interactions. This observation
occurs because cimetidine (Tagamet) is particularly effective in inhibiting the cytochrome P450 drug
metabolizing system therefore influencing the metabolism of other drugs. Additionally, cimetidine
(Tagamet) reduces liver blood flow and the combination of effects on blood flow and metabolism tend to
decrease the clearance (removal from the body) of certain drugs.
warfarin
Quinidine gluconate
(Quinaglute,
Quinalan)
Cimetadine inhibits clearance of these agents (partial listing):
propranolol
metoprolol
phenytoin (Dilantin)
(Inderal)
(Lopressor)
caffeine
lidocaine
(Xylocaine)
theophylline
labetalol (Trandate,
Normodyne)
alprazolam (Xanax)
triazolam (Halcion)
chlordiazepoxide
(Librium)
carbamazepine
(Tegretol)
ethanol
tricyclic
antidepressants
metronidazole
(Flagyl)
calcium channel
blockers
sulfonylureas
diazepam (Valium)
flurazepam
(Dalmane)