* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download nicotinic receptors
Pharmacokinetics wikipedia , lookup
Polysubstance dependence wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Drug design wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Orphan drug wikipedia , lookup
Drug discovery wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Toxicodynamics wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
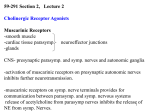
4 - 11 - 2013 pharmacology – sheet #16 Banan G. Zureikat We talked about cholinergic agonists in the previous lecture and in this lecture we will be mainly talking about the muscarinic blocking drugs urinary retention: Methacholine, Carbachole and Bethanechol are Ach derivatives (muscarinic agonists). One of the clinical uses of these drugs is urinary retention: we remember that the parasympathetic nervous system induces the rest and digest response; thus when it's activated it will cause contraction of the bladder walls and relaxation of the sphincter, so these drugs can be used for urinary retention (inability to urinate). Bethanechol: - Used to treat postsurgical bladder dysfunction associated with the retention of urine. - Most commonly given orally, but it also can be given subcutaneously to get a faster effect. - It's mechanism of action: it increase the tone and contractility of the smooth muscles of the urinary bladder and relax the sphincter Metacholine is used as a diagnostic tool to know whether this patient has asthma or not, by performing a test in which the patient is given metacholine and observing the effect. So what will metacholine do to the bronchi? It will cause constriction of the bronchi. The Drs will observe the degree of the constriction in the patient and according to certain measurements they will decide whether it's normal or exaggerated constriction. If the constriction is exaggerated the patient will be diagnosed as asthmatic. Of course after completion of the test we need to dilate the patient's bronchi, so a rapid-acting bronchodilator is given to counteract the bronchoconstriction caused by Methacholine. [Beta 2 adrenergic agonists are the best drugs that can dilate the bronchi, e.g., albuterol and turbutaline]. Now we'll talk about indirectly acting cholinergic drugs: Such drugs will exert the same actions as Ach but they don't bind to the receptor, what they do is that they increase the amount of Ach present by inhibiting the enzyme that breaks Ach which is acetylcholinesterase. |Page1 4 - 11 - 2013 pharmacology – sheet #16 Banan G. Zureikat Examples of such drugs; Sarin gas/nerve gas which is irreversible inhibitor of Ach-esterase and there are also other drugs which are reversible inhibitors of Ach-esterase When do we need more Ach? One of the conditions where we need more Ach is mysthenia gravis disease: It's an autoimmune disease caused by antibodies to the nicotinic receptors at the neuromuscular junction. So we have destruction of the nicotinic receptors less number of nicotinic receptors those patients will suffer from muscle weakness, fatigue and their respiration might also be compromised. In this case we want to increase the amount of Ach to activate the remaining receptors. so we give them drugs such as neostigmine that mainly works on nicotinic receptors on the skeletal muscles end plate rather than the autonomic nervous system. We can conclude that: - Inhibition of Ach-esterase by anticholinesterases can be reversible or irreversible. - They provide cholinergic action by prolonging the life time of Ach. Thus they will affect both nicotinic and muscarinic receptors, as well as neuromuscular junctions. - Their action is going to be related to the action of Ach because they will mainly increase the amount of Ach present. Example of such drugs: Neostigmine and Physostigmine. The differences between these drugs are related to: - Polarity (which of them can cross the blood-brain barrier (BBB) and which can't) - Selectivity toward different enzymes; We have pseudo-acetylcholinesterase and realacetylcholinesterase, the pseudo-ach-esterase in plasma can degrade many drugs that are similar to Ach. Physostigmine: - Lipid soluble (not polar) so it can cross BBB, useful in Atropine poisoning. [atropine is a cholinergic muscarinic antagonist] Some people take atropine as a drug. Atropine is also present in a plant called Atropa belladonna and it can poison humans (it causes many of the cholinergic receptor blocking symptoms) so treat this overdose of atropine we use physostigmine to antagonize its effect by increasing the concentration of Ach. |Page2 4 - 11 - 2013 pharmacology – sheet #16 Banan G. Zureikat - Physostigmine is also used to treat overdose of drugs with strong antimuscarinic side effects: some drugs that we take such as anti-histamine and tricyclic anti-depressants work on the central nervous system by blocking their own receptors there, but they also have affinity towards the muscarinic receptors so they will block them. That's why we'll see anticholinergic effect with the use of these drugs. So when having an over dose of anti-histamine or tricyclic anti-depressants (antimuscarinic drugs) we can block their anticholinergic effects by the use of physostigmine. - Physostigmine is used as drops in the eyes to treat glaucoma but Pilocarpine is superior to it. Neostigmine: - Similar activity to Physostigmine but it's polar, so it doesn't go to the CNS (doesn't cross the BBB). - Its effects are mainly associated with nicotinic receptors that’s why it's useful in the treatment of mysthenia gravis (an auto immune disease that caused by antibodies to the nicotinic receptors at the neuromuscular junction). [It has more nicotinic effects than physostigmine] - It has a greater effect on the skeletal muscles. Remember: the parasympathetic nervous system has nicotinic and muscarinic receptors. The nicotinic receptors are the ones present in ganglia, and the muscarinic receptors are present at the neuroeffector sites. We also have nicotinic receptors at the skeletal muscles end plate. But these are not part of the autonomic nervous system. They are both nicotinic receptors and both are activated by nicotine and Ach but they're not exactly the same. So Neostigmine has more affinity for the nicotinic receptors in the skeletal muscles. That’s why its uses are more related to skeletal muscles. - Another use of Neostagmine: Tubacurarine is a nicotinic antagonist (was used to cause paralysis in animals while hunting). Clinically anesthetists use Tubacurarine and its derivative in operations to cause muscle relaxation. To reverse its effect in order to recover the patient from the paralysis of the muscles, we use Neostigmine. [The main use of this drug is to reverse the effect of neuromuscular blocking drugs that are used to induce muscle paralysis during surgical prosedures.] |Page3 4 - 11 - 2013 pharmacology – sheet #16 Banan G. Zureikat There are newly discovered indirectly acting cholinomimetic drugs that blocks Ach-esterase. They are used to treat Alzheimer. Why are they used in Alzheimer? In Alzheimer the cognitive ability of the patient decreases, and it was found out that Ach increases cognition, that's why these Ach esterase inhibitors are useful for patients with Alzheimer. Inhibition of Achesterase ach increase Ach in brain increase cognition. The last group is Organophosphates: Such as insecticides, nerve gas and chemicals for agricultural uses. A lot of the deaths among agricultural workers are because of the toxicity of these insecticides. If a patient was poisoned with insecticides, what symptoms might he suffer from? Due to increased amount of Ach activation of parasympathetic nervous system, so such patients are characterized with : 1- Bradycardia 2- Pin point pupils (these patients when put in a dark room their pupils won't dilate like normal people do) 3- Perfused sweating: In addition to the inhibition of the muscarinic function, these agents block the few sympathetic neurons that are cholinergic, such as those innervating sweat glands (Ach works on sweat glands, this is the exception of sympathetic nervous system) 4- Fatigue because of the weakening of the muscles Note: activating sympathetic nervous system centrally will cause increase in the sweating (activation), while giving adrenergic agonists won't affect sweating. Insecticide poisoning is same as nerve gas poisoning; both cause irreversible blocking of nicotinic receptors. These patients will probably die from the inability of the respiratory muscle to contract efficiently, so we try to save these patients: initially by giving them anticholinergic drugs to decrease the effects of agonists (we prevent ach from reaching the receptor and activating it). Then we'll try to recover the enzyme by a drug called Pralidoxime (also called 2 PAM) it helps in the recovery of the enzyme to presume its partial function but it doesn't recover it fully, it only recovers it partially. This leads to an increase in the breakdown of Ach. This drug should be used early on before we reach muscle paralysis phase. |Page4 4 - 11 - 2013 pharmacology – sheet #16 Banan G. Zureikat Note: continuous contraction of the muscles due to binding of ach to the receptors (muscle fasciculations) will prevent the muscle from reaching refractory period, eventually the muscle won't respond and that's what we mean by paralysis. There're 2 kinds of paralysis: 1- paralysis due to blocking of the nicotinic receptors 2- paralysis due to excessive stimulation of the muscle Organophosphates are irreversible while Neostigmine and Physostigmine are reversible. Now we'll talk about cholinergic antagonists: we'll start with the muscarinic receptors antagonists, these drugs will bind to the cholinergic muscarinic receptors and prevent their activation, they block the binding of Ach to them so they will lower the activity of ach and oppose the action of parasympathetic nervous system. atropine: it's a naturally present in a plant called Atropa belladonna Bella donna means beautiful woman in Italian. Because wide pupils are from the signs of beauty in women, they used this plant as a drop in the eye to dilate the pupils. Two drugs originate from Atropa belladonna: atropine and Scopolamine. These are organic esters formed by combination of aromatic acids, tropic acids and complex organic bases (we don't have to memorize this). These are competitive antagonists of muscarinic agonists competing for a common binding site. This means that these are blockers so they'll inhibit the binding of ach or any muscarinic agonist to its receptor, so they block the effect of parasympathetic activation (parasympathetic activation is opposed in all target sites). So what are the effects that we will see? On heart tachycardia (but initially we have Bradycardia due to complex mechanisms related to vagal stimulation of A.V and S.A nodes but the final effect is tachycardia) On salivation decrease, so dentally the effect is xerostomia (dry mouth). |Page5 4 - 11 - 2013 pharmacology – sheet #16 Banan G. Zureikat On the GIT relaxation and slowed peristalsis (motility). that’s why anticholinergic drugs are used to treat spasms of the GIT. e.g., motulin, riabal (for babies). On the urinary tract relaxation of the walls and contraction of the sphincter. In the eye pupil dilation spasm of accommodation/cilliary muscle blocking less accommodation increase eye pressure (increase glaucoma) On CNS drowsiness, antimotion sickness action, antiparkinson action, amnesia and delirium. Ach is a neurotransmitter present in brain and it's a CNS stimulant, so it increases cognitive abilities and stimulates many centers in brain like memory and the center responsible for motion sickness. So drugs that can cross the BBB like atropine can exert actions centrally, so they are used to reverse the action of Ach producing the previously mentioned effects on the CNS. Scopolamine: is used for seasickness because it has antimotion sickness action centrally. In the eye cycloplesia (spasm of accommodation of the eye – cilliary muscles doesn't contract well), mydriasis and reduction in lacrimal secretions. Note: usually with the parasympathetic inhibition we have reduction in the secretion of everything in our body (sweat gland , salivary gland, lacrimal gland also HCL secretion in stomach) that’s why in old days these drugs where used to treat peptic ulcers, but due to their numerous side effects they're not used any more, there're new better drugs. In bronchi they oppose the action of parasympathetic nervous system so they cause broncodilation. This is another clinical use for these drugs: a drug called ipratropium was used as treatment of asthma but because of the discovery of beta 2 adrenergic agonists, which are more selective, Ipratropium is not used much. (ipratropium is used when there are contraindications for beta 2 adrenergic agonists use, but it has many side effects) In GU (gastro-urinary tract) relaxation of the muscles and urinary retention. Glands decrease in secretions. |Page6 4 - 11 - 2013 pharmacology – sheet #16 Banan G. Zureikat Skin inhibition of sweating, hyperthermia and flushing of the skin of the face as a reflux to the inhibition of sweating. Remember there is no direct innervation by parasympathetic nervous system on blood vessels but there are some exceptions: 1- the skin of the face: activation of parasympathetic NS in skin of the face causes constriction of the blood vessels so when blocked, it causes dilation resulting in flushing. Flushing thus is due to: -dilation of blood vessels in the skin of the face -the reflux hyperthermia because of inhibition of sweating 2- the blood vessels of the penile tissue in the genitourinary tract (will be discussed later). Note: the parasympathetic antagonists have a lot of similar actions to the sympathetic agonists. The factors that decides which of them to use are: - the selectivity of the drug (to minimize the side effects): the more selective the better the drug is. - the intrinsic activity of each drug (the tendency of a drug to activate the signals in respective to how much drug is bound to the receptors) [the problem of parasympathetic antagonists is that they are not selective, so we usually have side effects all over the body while sympathetic agonist have a lot of selective agonists for the different subtypes of receptors.] Clinical applications for antimuscarinic drugs In CNS we use 2 drugs: 1) Benztropine: treat the manifestations of Parkinson disease 2) Scopolamine: reduces motion sickness In eye: Atropine is used to cause mydriases and cycloplegia. But it is used mainly locally because it's not selective and can cause many side effects if used systematically. Cyclopentolate is a derivative of atropine that's used when the Dr wants to examine the eye since it dilates the pupil. It has a shorter duration of action (6-24 hours) in comparison with atropine that stays in the body for almost one week. |Page7 4 - 11 - 2013 pharmacology – sheet #16 Banan G. Zureikat In bronchi: Ipratropium is a drug used to treat asthma (bronchodilator) In GIT: Methscopolamine reduces motility, so it's used in cases of spasms and contraction of the GIT. Side effect of this drug: constipation due to the reduction of motility. In GU: Oxybutanin is used to treat transient cystitis and postoperative bladder spasms. Cystitis: is the infection of bladder. Patients with cystitis need to urinate a lot because of the contraction of bladder. Atropine: it was isolated in the 1831. It’s a specific muscarinic antagonist but not selective for a specific subtype. Atropine effects: (not all of these effects are clinically used) What happens in body when we use atropine? -Increase heart rate -decrease the tone and motility of the GI tract -diminish salivary secretion -pupil dilation -relax urinary tract and airway smooth muscles Clinical uses of Atropine: -administered prior to anesthesia to reduce secretions of respiratory tract -to control rhinorrhea -used to treat peptic ulcers because it reduces the secretions of HCL in the stomach. -treatment of diarrhea -treatment of frequent urination and bedwetting -therapy of certain bradycardias and heart blocks -causes cycloplegia and mydriases when used in the eye -short term treatment of bronchiospasm associated with COPD. |Page8 4 - 11 - 2013 pharmacology – sheet #16 Banan G. Zureikat In dentistry Atropine is used to diminish salivation and to produce a dry field but it has one problem: it can cause bradycardia initially this is the first response of the body to atropine. Note: a patient is said to have bradycardia if his heart rate is less than 60 Overdose of atropine can cause tachycardia, blurred vision, photophobia, dry mouth it also can cause CNS excitation. Good Luck = |Page9