* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Muscle alanine synthesis and hepatic gluconeogenesis
Survey
Document related concepts
Beta-Hydroxy beta-methylbutyric acid wikipedia , lookup
Nucleic acid analogue wikipedia , lookup
Lactate dehydrogenase wikipedia , lookup
Point mutation wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Metalloprotein wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Peptide synthesis wikipedia , lookup
Proteolysis wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Protein structure prediction wikipedia , lookup
Genetic code wikipedia , lookup
Citric acid cycle wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Biosynthesis wikipedia , lookup
Transcript
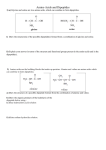
Biochemical Review Muscle alanine synthesis and hepatic gluconeogenesis KEITH SNELL Division of Biochemistry, Department of Biochemistry, Universiry of Surrey, Guiliford, Surrey GU2 5XH,U.K. Gluconeogenesis is the metabolic process involving the synthesis de novo of glucose molecules from other carbon precursors during situations in which there is an enhanced oxidative utilization of body glucose or in which there is a dietary insufficiency of carbohydrate to supply the body requirements for oxidative glucose metabolism. Glucose synthesis is, for the most part, confined to the liver, although in prolonged starvation in man the contribution by the kidney becomes substantial (Owen et al., 1969). In certain situations the hepatic gluconeogenic pathway may be operative in the face of an adequate dietary supply of carbohydrate, when carbon precursors are diverted towards the repletion of liver glycogen rather than to glucose synthesis for hepatic release into the circulation. Such situations include re-feeding after starvation (Hems et al., 1972) and the analogous situation of weaning following the suckling stage of neonatal development (K. Snell, unpublished work). Hepatic gluconeogenesis is regulated within the liver by metabolic and hormonal factors and indirectly by the supply of gluconeogenic precursors from peripheral tissues (see Exton, 1972 for review). Not only are the various precursors utilized at different rates for glucose formation within the liver, but the physiological circulating concentrations of many precursors lie below the saturating levels for hepatic glucose synthesis, as demonstrated in the perfused liver in vitro (Exton & Park, 1967; Mallette et al., 1969a) and the whole animal in vivo (Aikawa et al., 1972). Thus both the rate of precursor supply and the nature of the precursors will influence the rate of glucose formation by the liver. The principal endogenous glucogenic precursors are lactate, pyruvate and amino acids derived from skeletal muscle and other tissues, and glycerol derived from the hydrolysis of triacylglycerol in adipose tissue. Cahill and his colleagues have quantified the relative contribution of these various precursors to glucose formation in man, particularly during starvation when gluconeogenesis is increased (Cahill, 1970). As starvation is extended beyond 24 h, the relative contribution of proteinderived amino acids to total hepatic glucose production increases. A similar increased contribution has been observed in diabetic subjects where gluconeogenesis is also elevated above normal (Wahren et al., 1972). Of these amino acids, the contribution by alanine to hepatic glucose output is quantitatively the most significant. Hepatic extraction of alanine exceeds that of all other amino acids in the rat (Ishikawa, 1977) and man (Felig et al., 1969a) in vivo, and, in addition, it has been shown in the perfused liver in vitro that alanine is the best amino acid substrate for gluconeogenesis in the adult rat (Ross et al., 1967; Exton & Park, 1967). A specific stimulation of alanine transport into the liver cell has been found in starvation and after glucagon stimulation of gluconeogenesis (Mallette et al., 19696; Fehlmann et al., 1979). Sources of circulating alanine Measurements of arteriovenous differences across specific organs and work with isolated preparations of various tissues have shown that alanine is released into the circulation by a number of tissues, including skeletal muscle, heart, small intestine, kidney, adipose tissue and brain (Aikawa et al., 1973; IshiVol. 8 kawa, 1977; Ruderman & Berger, 1974; Snell & Duff,1977a,b; Taegtmeyer et al., 1977; Windmueller & Spaeth, 1974, 1975; Hanson & Parsons, 1977). Of these sources, skeletal muscle is undoubtedly the most significant contributor to circulating alanine, because it represents such a large fraction of the total body mass compared with other tissues and, moreover, contains almost 60% of the total body protein. Muscle protein therefore serves as an important metabolic reservoir of amino acid precursors for gluconeogenesis. Measurements of arteriovenous differences of amino acids across forearm and leg muscles in man (Felig et al., 1970; Felig & Wahren, 197 1) or rat (Ishikawa, 1977), and measurements of the pattern of amino acid release from the perfused hind-limb (Ruderman & Berger, 1974) or isolated rat muscle preparations (Odessey et al., 1974; Garber et al., 1976a) have shown that the relative proportions of the amino acids released by muscle do not correspond to the fractional amino acid composition of muscle proteins. The striking feature is that alanine and glutamine together account for more than 50% of the total amino acids released by skeletal muscle, which is considerably more than their relative abundance in muscle proteins. The implication of these findings is that alanine and glutamine release involves not only muscle proteolysis but also the synthesis de nouo of these amino acids from other amino acids within the muscle. The importance of alanine as a precursor for hepatic gluconeogenesis has been discussed above. In contrast, glutamine is not removed from the circulation by the liver but by the small intestine and kidney. The mucosal epithelial cells of the small intestine apparently utilize glutamine in a major way as a respiratory fuel (Hanson & Parsons, 1977; Windmueller & Spaeth, 1978; Watford et al., 1979). In addition, glutamine contributes both carbon and nitrogen for alanine formation and release by the intestine, so that glutamine is indirectly involved in hepatic gluconeogenesis insofar as it serves as a precursor of circulating alanine. Extraction of glutamine by the kidney is elevated in starvation and under acidotic conditions when the amino nitrogen is removed to produce ammonia for the neutralization of the acid urine (see Pitts, 1964). The carbon of glutamine may be oxidized or used for the synthesis of glucose (Hems, 1972); renal gluconeogenesis becomes of increasing significance with prolonged starvation (Cahill & Owen, 1968). What contribution glutamine makes to the net release of alanine by the kidney (Aikawa et al., 1973) is presently not known. Thus both alanine and glutamine released by skeletal muscle will make significant contributions to body glucose formation, although it is only alanine that is involved directly in hepatic gluconeogenesis. Muscle alanineformation Because alanine release by muscle is out of proportion to its relative abundance in muscle proteins, it is presumed that synthesis de nouo is involved in the formation of this amino acid in muscle. Alanine is formed by the transamination of glutamate and pyruvate catalysed by alanine aminotransferase (EC 2.6.1.2). For amino acids other than glutamate to contribute amino groups for alanine synthesis, they must first be transaminated with 2-oxoglutarate to produce glutamate, since direct transamination with pyruvate in muscle is essentially restricted to glutamate (Rowsell, 1956; Rowsell & Corbett, 1958). Muscle 2-oxoglutarate transamination only occurs to any appreciable extent with aspartate and the branched-chain amino acids (valine, leucine and isoleucine) (Krebs, 1975), so that these 205 BIOCHEMICAL SOCIETY TRANSACTIONS 206 Amino-oxyacetata 1-Cycloserine r--Valine I I I / I 3-Methyl-2-oxobutanoata- .-,-Succinyl-CoA !Citric acid cycle 1 Oxaloacetate -- Alanine 'm ' T 3-Mercap;opicdinate Phoophoenolpyruvste Lactatej l r " r u ~ ~ ~ Acetyl-CoA i c h l o ~ o ~ c e t a t e I Miowlo Glycogen A b other tissues Liver 1 1 amino acids and glutamate itself will be the major precursors for alanine formation. The linked transaminations catalyse the reactions: L-Amino acid + 2-oxoglutarate * L-glutamate+ 2-moacid L-Glutamate + pyruvate s 2-oxoglutarate + L-alanine Net = L-Amino acid + pyruvate = 2-0x0 acid + L-alanine Evidence for the involvement of transamination in alanine formation has come from the inhibitory effects of L-cycloserine and amino-oxyacetate (potent transaminase inhibitors) on alanine release from muscle in vivo (Blackshear et al., 1975) and in vitro (Ruderman & Berger, 1974; Garber et al., 1976a,b; Snell & Duff, 1977a; Snell, 1978) (see Scheme 1). Alanine aminotransferase catalyses a freely reversible reaction with an equilibrium constant of 0.67 (Krebs, 1953). :Measurements of the mass-action ratio of the reactants in freeze-clamped leg muscle from fed rats gave a value of 0.58 (Ruderman et al., 1977), which suggests that the concentrations of reactants in the cell are near to equilibrium values. Thus changes in the intracellular concentration of either glutamate or pyruvate will lead to changes in alanine concentration. The increased formation and release of alanine by the leg muscles of diabetic rats is apparently the result of an increase in intracetlular glutamate concentration leading to a displacement of the ahnine amhotransferase reaction from equilibrium and an increase in the mass action ratio from 0.58 to 0.95 (Ruderman et al., 1977). Since the branched-chain aminotransferase reaction has a similar equilibrium constant (0.57 with leucine as reactant; Taylor et al., 1970), it is to be expected that the provision of branched-chain amino acids would lead to an increase in intracellular glutamate concentration and an increased formation and release of alanine by the linked transaminations shown above. A number of workers have shown a stimulation of alanine release by various muscle preparations with added branched-chain amino acids (Odessey et al., 1974; Ruderman & Berger, 1974; Garber et al., 19766; Goldstein & Newsholme, 1976; Snell, 1976; Snell & Duff, 1977~).The freely reversible nature of these transaminations is shown by the fact that the addition of a branched-chain keto acid, 4-methyl-2-oxopentanoate or 3-methyl-2-oxobutanoate to hemidiaphragm incubations decreased alanine release to 50 and 33% respectively of the control values obtained without added keto acid (K. %ell& D. A. Duff, unpublished observations). Similar observations have been made by Spydevold et al. (1976) in the perfused hindlimb preparation. The addition of the branched-chain keto acids displaces the branched-chain aminotransferase reaction towards branched-chain amino acid and 2-oxoglutarate formation at the expense of glutamate. The decreased glutamate concentration will result in increased alanine transamination with 2-oxoglutarate, thus reducing the net formation of alanine. Changes in intracellular pyruvate availability for transamination to alanine can be brought about by stimulating pyruvate oxidation with dichloroacetate (which activates pyruvate dehydrogenase). This agent decreases alanine release from muscle In vivo (Blackshear et al., 1975) and decreases alanine, pyruvate and lactate release from muscle preparations In ultro (Snell, 1976; SneU & Duff, 1977a; Goodman et al., 1978) (see Scheme 1). The hypoglycaemic action of dichloroacetate (Stacpoole & Felts, 1970; Blackshear et al., 1974) may, in part, be due to a diminished supply of gluconeogenic precursors from muscle to the liver. On the other hand, increasing the availability of intracellular pyruvate by perfusing hind-limb preparations with lactate (Ruderman & Berger, 1974), by incubating isolated muscles in uftro with glucose (Odessey et al., 1974; Snell & Duff, 1977a) or pyruvate (Garber et al., 1976a), or by infusing pyruvate into post-absorptive man in uivo (Pozefsky & Tancredi, 1972) all increased the release of alanine. A consideration of the intracellular source of pyruvate for muscle alanine formation has led a number of workers to emphasize the role of glycolysis, and this has prompted the formulation of a 'glucose+ a l e e cycle' (Mallette et al., 1969a; Felig et al., 1970; Felig & Wahren, 1974). The glucose-alanine cycle The formulation of a glucose-alanine cycle embodies the concept that glucose taken up by muscle from the bloodstream 1980 207 BIOCHEMICAL REVIEW serves directly, or indirectly via glycogen, as a glycolytic source of pyruvate for alanine synthesis. Alanine is released into the circulation, taken up by the liver and converted by gluconeogenesis into glucose, which is then returned to the bloodstream (see Scheme 1). This scheme involves a constant recycling of glucose carbon between muscle and liver and complements the carbon recycling via lactate of the Cori cycle. The Cori cycle ensures that when skeletal muscle derives the energy for contraction by anaerobic glycogenolysis, the muscle lactate so formed can be reconverted by the liver to glucose, which can then serve to replenish the muscle glycogen stores (Cori, 193 1). The physiological role of the glucose-alanine cycle, however, probably rests in the fact that it serves as a transport system for amino acid nitrogen from muscle to liver, where the nitrogen is eliminated via conversion to urea Deamination of amino acids and ammonia formation occurs during muscular exercise through the operation of the purine nucleotide cycle (Lowenstein, 1972; Lowenstein 8c Goodman, 1978). Diversion of some of the amino acid nitrogen towards alanine formation would serve to prevent excessive generation of potentially toxic ammonia by the purine nucleotide cycle. The precise roles of amino acid breakdown and ammonia generation in muscle are not clear, but it may be that one function of ammonia formation is as an intracellular buffer to hydrogen ion production during ATP hydrolysis associated with contraction. Alanine formation may also serve as an alternative glycolytic end product to lactate. Diversion of some of the pyruvate towards alanine synthesis might prevent an excessive build-up of lactate, which might disturb the cellular redox state through the lactate dehydrogenase reaction. Both of these roles of alanine formation suggest that alanine release would be proportional to the extent of muscle anaerobic glycolysis and the intensity of muscular exercise. Felig 8c Wahren (1971) found with exercising human subjects that an increased release of alanine from leg muscles was indeed proportional to the intensity of the work being performed. However, contradictory findings have been reported with the contracting perfused hind-limb preparation of the rat, where lactate (and ammonia) release increased with the frequency of muscle contractions, but alanine release was decreased (although its concentration in muscle tissue did increase) (Goodman 8c Lowenstein, 1977). Evidence for decreased alanine formation due to a limitation of the glycolytic provision of pyruvate has come from observations on a patient with McArdle’s syndrome (Wahren er al., 1973). This condition is characterized by a lack of muscle phosphorylase and a consequent impairment of glycogenolysis. During muscular exercise the rate of glycolysis fails to increase, and decreases in arterial pyruvate and alanine concentrations were observed. Furthermore, the net release of alanine from leg muscle normally observed during exercise is abolished, and indeed reversed, in patients with McArdle’s syndrome (Wahren et al., 1973). In this pathological situation it appears that the rate of glycolysis becomes a limiting factor for alanine release during muscular exercise. In most physiological situations it seems unlikely that the rate of glycolysis is rate-limiting for alanine formation. Stimulation of glucose uptake and glycolysis by the addition of insulin to muscle incubations (K. Snell 8c D. A. Duff, unpublished observation; Odessey et al., 1974; Garber et al., 1976a) or to hind- limb perfusions (Ruderman & Berger, 1974; Goodman & Lowenstein, 1977) had a negligible or slightly inhibitory effect on alanine release, despite a stimulation of lactate and pyruvate release. Similarly, the addition of dibutyryl cyclic AMP to muscle homogenates (Snell, 1975) or B-adrenergic agonists to intact muscle preparations (Garber et al., 1976c; Li & Jefferson, 1977; Goodman & Lowenstein, 1977) decreased alanine release while increasing lactate and pyruvate release. The decreased alanine release in these experiments with hormonal agents is probably due to inhibitory effects on protein degradation (Fulks et al., 1975; Li 8c Jefferson, 1977) and hence a decreased availability of amino acids for glutamate formation and danine synthesis. A lack of association between glycolysis and alanine formation is also seen during starvation, where rates of release of pyruvate and lactate by incubated diaphragm muscle show a progressive increase as starvation periods become greater, but alanine release displays a delay of about 24h before increases are noted (Fig. 1; Snell 8c Duff, 1979). Again, the pattern of alanine release during progressive starvation correlates with protein degradation (Li & Goldberg, 1976). Pardridge & Davidson (1979) have also observed a lack of correlation between glycolysis and alanine formation in a myogenic line of rat skeletal-muscle cells in tissue culture. They conclude that alanine formation is linked to the intracellular concentration of pyruvate (above a certain critical level), but that this is not necessarily a function of the rate of glucose utilization. Although recycling of glucose carbon in a glucose-alanine cycle may be a source of much of the pyruvate used for alanine synthesis in exercising muscle in the fed rat, the situation during starvation, when there is an increased body requirement for net glucose synthesis, is different. The glucose-alanine cycle will not provide for any net addition of glucose to the body pool. In the face of continued oxidative glucose metabolism and in the absence of any dietary carbohydrate, glucose must therefore be synthesized from endogenous precursors. The major consumer of glucose during moderate starvation is the brain, although there is an adaptation of brain metabolism towards ketone-body utilization in prolonged starvation, which lessens this glucose requirement somewhat. During starvation, muscle protein is broken down and the amino acid carbon, which is released mainly in the form of alanine, can be converted by the liver to glucose for use by the brain. Indeed, calculations, based on arteriovenous differences across gluconeogenic tissues and nitrogen excretion in humans (Owen et al., 1969; Cahill, 1970), show that in starvation the glucose requirements of the brain can be accounted for by gluconeogenesis from amino acids derived from muscle protein (plus a smaller contribution from glycerol) (see Newsholme, 1976). In the very early stages of starvation some of the pyruvate available for alanine formation may arise by glycolysis from the partial breakdown of muscle glycogen reserves (Sugden et al., 1976; Snell & Duff, 1979). However, muscle protein breakdown is potentially a much more significant source of carbon and one that persists after glycogen breakdown has ceased (Table 1; Snell & Duff, 1979). Thus pathways must exist in muscle for the conversion of amino acid carbon skeletons to pyruvate for alanine formation, so that the alanine released may make a net gluconeogenic contribution to the body glucose pool. Table 1. Potential yield of blood glucose from rat diaphragm-muscle glycogen and protein during starvation Data taken from Snell & Duff (1979). The maximum glucose yield assumes a maximum yield of 1g of glucose from 1.7g of protein (Krebs, 1964). Starvation period (h) 0-24 24-48 48-72 Vol. 8 Loss of glycogen (mg/diaphragm) 0.25 0.00 0.07 Maximum glucose yield (mol) 1.4 0.0 0.4 Loss of protein (mg/diaphragm) 8.7 2.2 3.4 Maximum glucose yield (WOl) 28.5 1.2 11.1 208 Pathways of alanine synthesis from amino acids Valine, isoleucine, aspartate and glutamate are all theoretically able to supply pyruvate carbon for alanine synthesis, by contributing net carbon to the citric acid cycle. C, citric acidcycle intermediates can then produce pyruvate or phosphoenolpyruvate by decarboxylation. Leucine, which does not contribute net carbon to the citric acid cycle, is unable to produce pyruvate in this way. There is considerable evidence that the pyruvate for muscle alanine synthesis may originate, in part, from other amino acids. Inhibition of glucose uptake and metabolism by inhibitors of glycolysis, such as NaF (Goldstein & Newsholme, 1976) or iodoacetate (Garber et al., 1976a), had no effect on the rate of alanine release, or on the stimulation of alanine release by added amino acids, in isolated muscle incubations. Contradictory findings with these inhibitors have been reported by Chang & Goldberg (1978~).Garber et al. (19766) concluded on the basis of carbon-balance measurements that, in the presence of iodoacetate, the stimulation of alanine formation by the addition of amino acids was accompanied by a net efAux of total carbon that could only be accounted for by a contribution of amino acid carbon to alanine formation. Similar conclusions were reached by Goldstein & Newsholme (1976), who found that incubation of hemidiaphragms with glutamate or isoleucine in the absence of glucose increased alanine output and increased the intracellular concentration of pyruvate. Evidence for a contribution of branched-chain amino acid carbon to the concentrations of citric acid-cycle intermediates has been presented (Spydevold et al., 1976; Lee & Davis, 1979), and estimates of the rate of flux of C, citric acid-cycle intermediates to C, metabolites show that this is in excess of that required to account for reported rates of alanine release (Lee & Davis, 1979). On the other hand, Chang & Goldberg ( 1 9 7 8 ~ ) discount any contribution of amino acidderived pyruvate to alanine formation on the grounds that the rate of formation of glycolytically derived pyruvate in diaphragms incubated with 5 mM-glucose exceeds the possible net formation of pyruvate from proteolytically derived amino acids by some 30-fold. However, the rate of glycolysis in such muscle incubations in uitro is many times greater than that which occurs in resting muscle in uiuo or in the perfused hind-limb (Maizels et al., 1977). Grubb (1976) has shown that in the perfused hind-limb only 2.7% of the glucose taken up by the preparation appears as alanine, and she calculates that there is a short-fall of carbon for alanine formation that can only be balanced by an additional contribution through amino acid metabolism. It seems that indirect calculations of potential contributions by glycolysis and amino acid metabolism to muscle pyruvate formation give little indication of the actual relative contribution by either process. The absolute value for potential pyruvate formation from amino acids (Chang & Goldberg, 1978a) is sufficient to account for observed rates of alanine formation. Indeed in a subsequent paper, Chang & Goldberg (19786) calculate, on the basis of the amino acid frequency in muscle proteins and the actual measured rates of release by muscle, that the rate of intracellular metabolism of amino acids produced by protein breakdown is sufficient to account for the formation of glutamine de nouo. But, by using the same considerations, one could equally well account for the formation de nouo of alanine in a similar way. On the basis of the relative incorporation of radioactivity from [I4Clvalineor [14Clsuccinateinto alanine and glutamine, Chang & Goldberg (19786) conclude that glutamine formation is the major fate of amino acid metabolism by muscle. However, such quantitative conclusions of net carbon flux are difficult to make in view of the possibilities of radioactivity exchange reactions and particularly since the specific radioactivities of the immediate precursors of the alanine and glutamine were not known. In addition, the assumptions that the specific radioactivity of lactate released into the medium is equal to that of intramitochondrial pyruvate, and that the ratio of radioactivity recovered in lactate to that recovered in CO, equals the BIOCHEMICAL SOCIETY TRANSACTIONS ratio of the rate of lactate release to that of pyruvate oxidation are not valid (Ottaway & Mowbray, 1977), and so the quantitative interpretations of the metabolic fates of pyruvate and of carbon chains entering the citric acid cycle (Chang & Goldberg, 19786) are very uncertain. The findings of incorporation of radioactivity from [I4Clvaline, [“Clsuccinate (Chang & Goldberg, 19786) or [14Clpropionate (Lee & Davis, 1979) into alanine by muscle preparations indicate that the necessary enzymic reactions for the conversion of amino acid carbon to alanine are present in muscle. The pathway for the production of pyruvate from citric acidcycle intermediates could involve the decarboxylation of malate by NAD+- or NADP+-dependent malate dehydrogenase (decarboxylating), or the decarboxylation of oxaloacetate to phosphoenolpyruvate by phosphoenolpyruvate carboxykinase followed by pyruvate kinase action. Both phosphoenolpyruvate carboxykinase (Opie & Newsholme, 1967; Nolte et al., 1972; Newsholme & Williams, 1978; Snell & Duff, 1979) and NAD+- or NADP+-dependent malate dehydrogenase (Nolte et al., 1972; Lin & Davis, 1974; Newsholme & Williams, 1978; Snell & Duff, 1979) activities have been found in skeletal muscle. During starvation, when muscle alanine release is increased (Karl et al., 1976; Snell & Duff, 1979), phosphoenolpyruvate carboxykinase activity is also increased (Newsholme & Williams, 1978; Snell & Duff, 1979), whereas NADP+-dependent malate dehydrogenase activity is decreased (Snell & Duff, 1979) or is unchanged (Karl et al., 1976; Newsholme & Williams, 1978). Similarly, dietary supplementation with valine or isoleucine leads to an increase in alanine release by muscle (Snell, 1979), with an increase in phosphoenolpyruvate carboxykinase activity but little change in NADP+-malate dehydrogenase activity (Newsholme & Williams, 1978; Snell, 1979). Also, mercaptopicolinate, an inhibitor of phosphoenolpyruvate carboxykinase, inhibits the glutamate- or valine-stimulated release of alanine by diaphragm muscle from starved rats ( b e l l & Duff, 1977~).This is further evidence for a pathway of pyruvate formation for alanine synthesis, which involves decarboxylation of citric acidcycle intermediates via phosphoenolpyruvate carboxykinase (Scheme 1). Alanine release in the presence of leucine, which cannot contribute net carbon to the citric acid cycle, was unaffected by mercaptopicolinate. In fed rats, mercaptopicoh a t e was ineffective in blocking glutamate- or valine-stimulated alanine release by diaphragm muscle (Snell & Duff, 1977a) or in blocking incorporation from [14Clpropionateinto alanine in perfused hind-limb preparations (Lee & Davis, 1979). The reasons for the difference between fed and starved rats in this respect are not clear, but it suggests that in the fed rat decarboxylation of citric acid-cycle intermediates occurs by a route other than via phosphoenolpyruvate carboxykinase. A similar difference in mercaptopicolinate sensitivity between fed and starved rats was observed for valine-stimulated alanine release from adipose tissue ( h e l l & Duff, 19776), and the agent was ineffective in blocking glutamine-stimulated alanine release by isolated intestinal preparations from fed rats (Hanson & Parsons, 1977; Watford et al., 1979). Thus the pathway for pyruvate production from citric acid-cycle intermediates appears to vary between different tissues, and in the same tissue in different physiological situations. Nevertheless, in situations associated with enhanced rates of gluconeogenesis, muscle appears to synthesize alanine by a pathway involving phosphoenolpyruvate carboxykinase. Branched-chain amino acid metabolism and alanine formation Muscle is believed to be the major body site of branchedchain amino acid metabolism (Adibi, 1976), in contrast with most other amino acids that are predominantly metabolized by the liver. Thus the release of branched-chain amino acids by muscle is less than would be expected from their relative frequency in muscle proteins (Ruderman & Berger, 1974; Odessey et al., 1974), and it can be calculated that their intracellular 1980 209 BIOCHEMICAL REVIEW metabolism is sufficient to account for the observed rate of alanine synthesis de nouo (cf. Chang & Goldberg, 19786). In vitro the branched-chain amino acids are among the most effective precursors for alanine formation (Ruderman & Berger, 1974; Odessey et al., 1974; Garber et al., 19766; Snell & Duff, 1977~).Intracellular protein breakdown is probably the major source of the amino acids, particularly in situations such as starvation and diabetes, although an additional supply may come from the liver, which releases branched-chain amino acids during starvation in rats (Mallette et al., 19698; Bloxham, 1972) and man (Marliss et af., 1971), in diabetic rats (Miller, 1962) and man (Felig, 1973), and after protein ingestion in normal and diabetic man (Wahren et al., 1976). In the last example the actual source of the amino acids is from intestinal absorption, but, because of the minor role of the liver in their metabolism, they escape hepatic uptake and account for more than half of the initial total amino acid uptake by leg muscles (Wahren et al., 1976). Protein feeding results in a continuous output of alanine and glutamine by leg muscles (Wahren et al., 1976), and it is likely that this is due, in large part, to metabolism of the branchedchain amino acids taken up by the muscle. It is significant in this respect that dietary supplementation of rats with branched-chain amino acids results in increased alanine output by muscles in uitro (Snell, 1979) and in elevations of phosphoenolpyruvate carboxykinase (the enzyme implicated in the carbon pathway from branched-chain amino acids to alanine) (Newsholme & Williams, 1978; Snell, 1979), and branchedchain keto acid dehydrogenase (the rate-limiting enzyme of branched-chain amino acid catabolism) (Shinnick & Harper, 1977). Similarly, starvation, which results in increased alanine release by muscle (Snell & Duff, 1979), is also accompanied by increased branched-chain amino acid metabolism (Goldberg & Odessey, 1972) and elevated phosphoenolpyruvate carboxykmase activity (Newsholme & Williams, 1978; Snell & Duff, 1979). These findings suggest that there is an intimate link between branched-chain amino acid oxidation and alanine formation in muscle. As well as acting themselves as precursors for alanine synthesis, the branched-chain amino acids may also control the flow of other amino acid mecursors derived from protein breakdown and so indirectly atTect alanine synthesis (see Scheme 1). Thus the branched-chain amino acids, and leucine in particular, uniquely stimulate protein synthesis and independently inhibit protein degradation in muscle (Odessey et al., 1974; Fulks et al., 1975; Buse & Reid, 1975). The mechanisms of these effects on protein turnover are not known, but metabolism of the branchedchain amino acids may play a crucial regulatory role, either by determining the intracellular concentrations of the amino acids themselves or of some regulatory product of amino acid oxidation, which in turn influence the process of protein turnover. The association between branched-chain amino acid metabolism, protein degradation and alanine release is illustrated by the similarity in the patterns of these metabolic processes during progressive starvation (Fig. 1). One feature of branched-chain amino acid metabolism and alanine formation that is not apparent from Scheme 1 is the possible location of the various reactions in different intracellular compartments. The coupling of the branched-chain aminotransferase and alanine aminotransferase to effect the transfer of nitrogen from the branchedchain amino acids to pyruvate to form alanine suggests that it might be appropriate if these two enzymes shared the same intracellular compartment to facilitate this transfer. Over 90% of alanine aminotransferase activity is present in the cytosol fraction of various muscle types (Table 2; DeRosa & Swick, 1975). Moreover, kinetic considerations suggest that the cytosol isoenzyqe form of alanine aminotransferase is more appropriate for catalysing alanine formation from pyruvate than the mitochondrial isoenzyme form (DeRosa & Swick, 1975). Ichihara et al. (1975) have reported that most of the branchedchain aminotransferase activity (72%) is located in Vol. 8 lo r - 0.4 $= .c, E - 0.3.Zo 0 - 0.2 - 0.1 3: 3 e: O M I=--- 4z > E OL -0 OL 1 0 2 3 Starvation period (days) Fig. 1. Effect of progressive starvation on alanine release, valine oxidation andprotein degradation by rat muscle Alanine release (0) in the presence of 3 mwvaline (Snell & Duff, 1979) and [ l-l'Clvaline oxidation (0) in the presence of 0.1mMvaline (Goldberg & Oddessey, 1972) were measured in incubations with hemidiaphragms. Protein degradation was measured by the rate of tyrosine released (A) by soleus muscle incubated with 10mM-ghCOSe and 0.5 mM-cycloheximide (Li & Goldberg, 1976). The data are taken from the references cited. Table 2. Subcellular distribution of alanine aminotransferase in rat muscle tissues Particle and cytosol fractions were prepared by differential sedimentation from rat muscle homogenates as described by Snell (1978). Alanine aminotransferase was assayed as previously (Snell, 1978) and activities are given as the meanf S.E.M. for four observations in each case Alanine aminotransferase activity (pmollmin per g of tissue) Muscle tissue Diaphragm Heart Hind-limb r Total 2.75 k0.24 2.10k0.20 4.84k0.35 Particulate 0.19kO.02 0.12k0.01 0.54+0.02 cytosol 3 2.48k0.22 1.91 k0.28 4.78k0.32 the particulate fraction of (unspecified) muscle. In addition, the subsequent oxidation of the keto acid carbon chain derived from the branched-chain amino acids takes place intramitochondrially (see Dancis & Levitz, 1972). From these findings it may be inferred that there must be a transfer of branched-chain amino acid nitrogen from the mitochondria to the cytosolic location of alanine aminotransferase, and Scheme 2(a) (Snell & Duff, 1977a) is an attempt to account for this. In this scheme mitochondrial aspartate efflux serves a dual function as a carrier of both branched-chain amino acid nitrogen and of oxaloacetate carbon derived from oxidation of the valine carbon skeleton. Transamination of aspartate in the cytosol not only donates amino nitrogen for glutamate and alanine formation, but also generates oxaloacetate, which, through the action of phosphoenolpyruvate carboxykinase, can provide phosphoenolpyruvate and pyruvate for alanine formation. The presence of aspartate aminotransferase in both mitochondrial and cytosolic compartments (Snell, 1978) is necessary for aspartate to fulfil this function. However, Odessey & Goldberg (1979) have reported that branched-chain aminotransferase activity is largely (68%) cytosolic in hind-limb muscles, while confirming that further metabolism of the carbon skeleton is confined to the mitochondrial compartment. This contradictory finding on the intracellular location of the aminotransferase activity necessitates a reappraisal of the scheme for the compartmentalization of the reactions involved in alanine formation, as shown in Scheme 2(b). In this revised scheme, mitochondrial aspartate efflux is still required to provide cytosolic oxaloacetate in order to BIOCHEMICAL SOCIETY TRANSACTIONS 210 Cytosol IbJ VaIine ~ 2 - O x o g l u ~ r a t e ~ . ~ l a n i n e 3-MetwZ-oxobutyrate Glutamate P y r u v a t e L Phosphoenolpyruvate Aspartate' 2-Oxoglutarate Cytosol Mitochondria 4 3 - M e t h v l - 2 - o x o b u t v r a t e ~ Succinyl-CoA,~ - I I Aspartate 2-Oxoglutarate 6 V A . B 0xaloacetate"Glutamate I Scheme 2. Intracellular compartmentalization of the proposed pathway of alanine formationfrom valine in muscle of starved rats Mitochondrial-cytosolic inter-relationships based on ( a ) mitochondrial localization of branched-chain aminotransferase, and (b) cytosolic localization of branched-chain aminotransferase are shown. The locus of action of the inhibitor 2-amino-4-methoxy-trans-but3-enoate fAMB) is indicated. The enzymes involved are: 1, alanine aminotransferase (EC 2.6.1.2); 2, cytosolic aspartate aminotransferase (EC 2.6.1.1); 3, phosphoenolpyruvate carboxykinase (EC 4.1.1.32); 4,pyruvate kinase (EC 2.7.1.40); 5, branched-chain aminotransferase (EC 2.6.1.6); 6, mitochondrial aspartate aminotransferase (EC 2.6.1.1); 7, enzymes converting 3-methyl-2-oxybutyrate into succinyl-CoA; 8, enzymes of the citric acid cycle converting succinyl-CoA into oxaloacetate. produce pyruvate for alanine formation by the pathway involv- formation, this prevents the reoxidation of cytosolic NADH, ing phosphoenolpyruvate carboxykinase. Evidence for a role of which is normally effected by the reduction of pyruvate to lacaspartate transamination in the formation of alanine has come tate by the lactate dehydrogenase reaction. from experiments with 2-amino-4-methoxy-trans-but-3-enoic acid, a relatively specific inhibitor of aspartate aminotransferase, Role of alanine in regulation of interorgan metabolism which diminished the valine-stimulated release of alanine by diaThe importance of muscle alanine formation in hepatic glucophragm muscle in vitro (Snell, 1978). Other evidence has shown neogenesis during starvation has been emphasized in this disthat there is a mitochondrial efflux of aspartate in the perfused cussion. During starvation there is a net breakdown of body rat heart associated with an increased concentration of alanine protein to provide amino acid carbon, carried mainly in the form of alanine, for the net synthesis of glucose by the liver. The (Safer & Williamson, 1973). Where the source of pyruvate for alanine formation is from major organ involved in the utilization of circulating glucose in glycolysis rather than from citric acid-cycle intermediates (as these circumstances is the brain. However, it is evident that a when leucine serves as a precursor), then the oxaloacetate continued breakdown of proteins, as starvation continues for carbon from aspartate must be returned from the cytosol to the .prolonged periods, is likely to jeopardize survival. Thus it is not mitochondria in the form of malate to prevent depletion of mito- surprising that adaptive mechanisms have evolved to prevent the chondrial oxaloacetate. The cytosolic formation of malate from dissolution of body protein in this situation, and nitrogen excreoxaloacetate also serves to reoxidize cytosolic NADH formed in tion is drastically curtailed. Coincident with this diminution of the triose phosphate dehydrogenase glycolytic reaction and protein catabolism, glucose utilization and production are ensures a continued glycolytic production of pyruvate for markedly reduced (Owen et al., 1969), and this is due to a alanine formation. This circumvents the theoretical dificulty decreased utilization of glucose by the brain, which adapts to the t h t when pyruvate formed by glycolysis is utilized for alanine utilization of circulating ketone bodies to satisfy its energy 1980 21 1 BIOCHEMICAL REVIEW Scheme 3. Regulatory role of alanine and ketone bodies in the interorgan metabolism of carbohydrate,fat and protein Solid lines indicate biochemical transformations and broken lines indicate regulatory effects; 0.stimulation; 0, inhibition; BCAA, branched-chain amino acids. This scheme is modified from that of Newsholme (1976). In starvation, ketone bodies replace glucose as a fuel for brain metabolism, restrict lipolysis in adipose tissue, so that fatty acid provision keeps pace with oxidation in muscle and with ketogenesis, and conserve muscle protein by inhibiting protein breakdown and alanine formation. Diminished muscle alanine release restricts hepatic gluconeogenesis, in keeping with the adaptations in brain metabolism. In protein feeding, alanine serves as a gluconeogenic precursor, stimulates hepatic glucose production and restricts hepatic ketogenesis, in keeping with the availability of glucose as a fuel. Overlaying these metabolic controls are hormonal controls by insulin (released by ketone bodies) and glucagon (released by alanine). Insulin and glucagon release is also influenced by the blood glucose concentration (not shown). requirements (Owen et al., 1967; 1969; Ruderman et al., 1974). mechanism by which protein breakdown and alanine release is Because of this switch in metabolic behaviour by the brain, there diminished during prolonged starvation is not explicable in terms is a reduced requirement for gluconeogenesis, which in turn of the hormonal changes in this situation (insulin is lowered and serves to spare body protein breakdown. glucagon is raised). It seems that ketone bodies may regulate the The key factor responsible for the reduction in gluconeogene- breakdown of protein and the release of alanine by a direct sis during prolonged starvation appears to be the decreased action on muscle. Blackburn et al. (1973) and Hoover et al. availability of alanine from peripheral tissues. Thus circulating (1975) showed that infusions of amino acid into patients alanine concentrations fall to a much greater extent than other recovering from surgery caused a hyperketonaemia while amino acids, and this is reflected in a fall in the uptake of alanine reducing nitrogen loss. Infusion of ketone bodies into human by the splanchnic bed (Felig et al., 1969~).Measurements of subjects resulted in a specific decline in plasma alanine compararteriovenous differences across the forearm of starved human able with that observed in starvation and caused a decrease in subjects showed that the release of amino acids, but most urinary nitrogen excretion in starved subjects (Sherwin et al., dramatically that of alanine, was reduced during prolonged star- 1975). The addition of ketone bodies to incubated diaphragm vation (Felig et al., 1970). That the availability of alanine, from muscle in vitro resulted in decreased protein breakdown and a muscle and other peripheral tissues, rather than a change in its decrease in alanine release (Palaiologos & Felig, 1976). The hepatic metabolism, is responsible for limiting gluconeogenesis mechanism of this effect of ketone bodies is not known, but, in in this situation is shown by the immediate rise in blood glucose view of their inhibitory action on branched-chain amino acid concentration, and in the incorporation of radioactivity from oxidation (Buse et al., 1972), one possibility is the accumulation [“Clalanine into blood glucose that is observed after alanine of branched-chain amino acids in the muscle leading to inhibiinfusion into starved human subjects (Felig et al., 1969b). The tion of protein degradation and/or stimulation of protein VOl. 8 9 212 synthesis, which would diminish the flow of amino acid precursors for alanine formation. Inhibition of branchedchain amino acid metabolism by ketone bodies may also directly affect alanine formation by blocking the flow of carbon skeletons to pyruvate. Whatever the mechanism, these findings indicate that the circulating concentrations of ketone bodies regulate protein turnover in muscle, and, by diminishing alanine release, reduce the blood concentration of alanine and thereby decrease gluconeogenesis. Thus ketone bodies have a dual role in prolonged starvation: they diminish glucose utilization by the brain by serving as an alternative fuel, and they reduce gluconeogenesis through a decrease in alanine release, which conserves body protein. The effect of ketone bodies on the regulation of protein and amino acid metabolism extends the role of these metabolites in the integration of metabolism in the body (see Newsholme, 1976). Scheme 3 depicts these inter-relationships in metabolism and includes the effects of ketone bodies on fat, carbohydrate and protein metabolism. A further regulatory facet of alanine-ketone-body interactions is the effect of alanine on ketone-body production. Alanine infusion is known to result in hypoketonaemia in man (Genuth, 1973;Genuth & Castro, 1974) and rats (Ozand et al., 1977). This effect is due to an inhibition of ketogenesis in the liver (Ozand et al., 1978). An increase in circulating alanine will result in an increase in gluconeogenesis (see above), but there is also evidence that alanine will stimulate gluconeogenesis from other precursors (Ozand el al., 1978). In addition, alanine is known to promote the release of pancreatic glucagon (Muller et al., 1971; Wise et al., 1972, 1973a,b), which stimulates hepatic gluconeogenesis directly (Exton, 1972), as well as indirectly by increasing alanine transport into the liver (Mallette ef al., 19696; Fehlman el al., 1979). Thus an increase in circulating alanine, such as occurs after protein feeding, will encourage glucose formation and inhibit ketogenesis, leading to a switch in body fuel metabolism as the availability of glucose increases. When glucose is plentiful, there is evidence that alanine may have a stimulatory role in diverting gluconeogenic substrates towards glycogen synthesis (Katz et al., 1976). It appears that the circulating concentrations of ketone bodies and alanine may complement each other in controlling the interorgan patterns of carbohydrate, fat and protein metabolism (Scheme 3). Conclusions It is clear that alanine plays a major role in glucose homoeostasis. One illustration of this is the many disease states in which disturbances in glucose homoeostasis are associated with alterations in the availability of alanine from peripheral tissues (Felig, 1973; Ruderman, 1975). The carbon of the alanine released from muscle must be derived from amino acids produced by protein breakdown, if the alanine is to make a net contribution to body glucose through hepatic gluconeogenesis. The quantitative aspects of the amount of pyruvate for alanine formation that is produced from other amino acids compared with that originating by glycolysis are not yet clear. The metabolic pathway involved in alanine synthesis using the carbon of other amino acids remains to be established, although current evidence favours a role for phosphoenolpyruvate carboxykinase in this process. There appears to be a correlation between branched-chain amino acid metabolism and alanine formation in muscle, but further understanding is required of the precise interrelationship and their metabolic and hormonal regulation. An understanding of this problem may help to explain the bouts of hypoglycaemia associated with the genetic impairment of branchedchain amino acid metabolism in Maple Syrup Urine disease. The branched-chain amino acids may provide a link between muscle protein turnover and alanine release, and future work in this area might provide insights into possible mechanisms that underlie various muscle-wasting conditions, such as BIOCHEMICAL SOCIETY TRANSACTIONS diabetes, muscular dystrophy and tumour-related cachexia. Circulating alanine concentrations influence metabolic processes in other tissues and vary inversely to ketone-body concentrations. The concentration of alanine and ketone bodies may play an important role in integrating the interorgan metabolism of carbohydrate, fat and protein. Adibi, S. A. (1976)Metab. Clin. Exp. 25, 1287-1302 Aikawa, T., Matsutaka, H., Takezawa, K. & Ishikawa, E. (1972) Biochim. Biophys. Acta 279,234-244 Aikawa, T., Matsutaka, H., Yamamoto, H., Okuda, T., Ishikawa, E., Kawano, T. & Matsumura, E. (1973) J. Biochem. (Tokyo) 74, 1003-1017 Blackburn, G. L., Flatt, J. P., Clowes, G. H. A., O’Donnell, T. F. & Hensle, T. E. (1973) Ann. Surg. 125,588-594 Blackshear, P. J., Holloway, P. A. H. & Alberti, K. G. M. M. (1974) Biochem. J. 142,279-286 Blackshear, P. J., Holloway, P. A. H. & Alberti, K. G. M. M. (1975) Biochem. J. 150,379-387 Bloxham, D. L. (1972) Br. J. Nutr. 27,233-247 Buse, M. G. & Reid, S . S . (1975)J. Clin. Invest. 56, 1250-1261 Buse, M. G., Biggers, J. F., Friderici, K. H. & Buse, J. F. (1972)J. B i d . Chem. 247,8085-8096 Cahill, G. F. (1970) N. Engl. J. Med. 282,668-675 Cahill, G. F. & Owen, 0. E. (1968) in Carbohydrate Metabolism and its Disorders (Dickens, F., Randle, P. J. & Whelan, W. J., eds.), vol. 1, pp. 497-552, Academic Press, London Chang, T. W. & Goldberg, A. L. ( 1 9 7 8 ~ J. ) Biol. Chem. 253, 36773684 Chang, T. W. & Goldberg, A. L. (19786) J. B i d . Chem. 253, 36853695 Cori, G. F. (193 1) Physiol. Rev. 11, 143-275 Dancis, J. & Levitz, M. (1972) in The Metabolic Basis of Inherited Disease (Stanbury, J. B., Wyngarden, J. B. & Fredrickson, D. S., eds.), pp. 4 2 6 4 3 9 , McGraw-Hill, New York DeRosa, G. & Swick, R. W. (1975)J. Biol. Chem. 250,7961-7967 Exton, J. H. (1972) Metab. Clin. Exp. 21,945-990 Exton, J. H. & Park, C. R. (1967) J. B i d . Chem. 242,2622-2636 Fehlmann, M., Le Cam, A., Kitabgi, P., Rey, J.-F. & Freychet, P. (1979) J. Biol. Chem. 254,401-407 Felig, P. (1973) Metab. Clin. Exp. 22, 178-207 Felig, P. & Wahren, J. (1971) J. Clin. Inuest. 50,2703-2714 Felig, P. & Wahren, J. (1974) Fed. Proc. Fed. Am. SOC.Exp. Biol. 33, 1092- 1097 Felig, P., Owen, 0. E., Wahren, J. Br Cahill, G. F. ( 1 9 6 9 ~ J. ) Clin. Inuest. 48,584-594 Felig, P., Marliss, E., Owen, 0. E. & Cahill, G. F. (1969b) Adu. Enzyme Regul. 7 , 4 1 4 6 Felig, P., Pozefsky, T., Marliss, E. & Cahill, G. F. (1970) Science 167, 1003-1004 Fulks, R. M., Li, J. B. & Goldberg, A. L. (1975) J. B i d . Chem. 250, 290-298 ) B i d . Chem. 251, Garber, A. J., Karl, I. E. & Kipnis, D. M. ( 1 9 7 6 ~J. 826-836 Garber, A. J., Karl, I. E. & Kipnis, D. M. (19766) J. B i d . Chem. 251, 836-84 3 Garber, A. J., Karl, I. E. & Kipnis, D. M. (1976~)J . Biol. Chem. 251, 85 1-857 Genuth, S . M. (1973) Metab. Clin. Exp. 22, 927-937 Genuth, S. M. & Castro, J. (1974)Metab. Clin. Exp. 23,375-386 Goldberg, A. L. & Odessey, R. (1972) Am.J. Physiol. 233, 1384-1391 Goldstein, L. & Newsholme, E. A. (1976) Biochem. J . 154,555-558 Goodman, M. N. & Lowenstein, J. M. (1977) J. B i d . Chem. 252, 5054-5060 Goodman, M. N., Ruderman, N. B. & Aoki, T. T. (1978) Diabetes 27, 1065-1074 Grubb, B. (1976) Am. J. Physiol. 230, 1379-1384 Hanson, P. J. & Parsons, D. S . (1977) Biochem. J . 166,509-5 19 Hems, D. A. (1972) Biochem. J. 130,671-680 Hems, D. A., Whitton, P. D. & Taylor, E. A. (1972) Biochem. J. 129, 529-538 Hoover, H. C., Grant, J. P., Gorschbath, C. & Ketcham, A. S. (1975) N. Engl. J. Med. 293, 172-175 Ichihara, A., Yamasaki, Y., Masuji, H. & Sato, J. (1975) in Isoenzymes (Markert, C. L., ed.), vol. 3, pp. 875-889, Academic Press, New York Ishikawa, E. (1977) Adu. Enzyme Regul. 14, 117-136 1980 BIOCHEMICAL REVIEW Karl, I. E.,Garber, A. J. & Kipnis, D. M. (1976)J. Biol. Chem. 251, 844-850 Katz, J., Golden, S. & Wals, P. A. (1976)Proc. Natl. Acad. Sci. U.S.A. 73,3433-3437 Krebs, H. A. (1953)Biochem. J. 54,82-86 Krebs, H. A. (1964)in Mammalian Protein Metabolism (Munro, H. N. & Allison, J. B., eds.), vol. 1, pp. 125-176, Academic Press, New York Krebs, H. A. (1975)Adv. Enzyme Regul. 13,449-472 Lee, S.-H. & Davis, E.J. (1979)J.Biol. Chem. 254,420-430 Li, J. B. & Goldberg, A. L. (1976)Am. J. Physiol. 231,441-448 Li, J. B. & Jefferson, L. S. (1977)Am. J. Physiol. 232, E243-E249 Lm,R. C. & Davis, E. J. (1974)J.Biol. Chem. 249,3867-3875 Lowenstein, J. M. (1972)Physiol. Rev. 52,382-414 Lowenstein, J. M. & Goodman, M. N. (1978)Fed. Proc. Fed. Am. SOC. Exp. Biol. 37,2308-2312 Maizells, E. Z.,Ruderman, N. B., Goodman, M. N. & Lan, D. (1977) Biochem. J. 162,557-568 Marliss, E. B., Aoki, T. T., Pozefsky, T., Most, A. & Cahill, G. F. (1971)J.Clin. Invest. SO, 814-817 Mallette, L. E., Exton, J. H. & Park, C. R. (1969a)J.Biol. Chem. 244, 5713-5 723 Mallette, L. E., Exton, J. H. & Park, C. R. (19696)J. Biol. Chem. 244, 5724-5 728 Miller, L. L. (1962)in Amino Acid Pools (Holten, J. T., ed.), pp. 708721,Elsevier, Amsterdam Muller, W. A., Faloona, G. R. & Unger, R. H. (1971)J. Clin. Invest. 50,2215-2218 Newsholme, E. A. (1976)Clin. Endocrinol. Metab. 5,543-578 Newsholme, E. A. & Williams, T. (1978)Biochem. J. 176,623-626 Nolte, J., Brdiczka, D. & Pette, D. (1972)Biochim. Biophys. Acta 284, 497-507 Odessey, R. & Goldberg, A. L. (1979)Biochem. J. 178,475-489 Odessey, R., Khairallah, E. & Goldberg, A. L. (1974)J. Biol. Chem. 249,7623-7629 Opie, L. H. & Newsholme, E. A. (1967)Biochem. J. 103,391-399 Ottaway, J. H. & Mowbray, J. (1977)Curr. Top. Cell. Regul. 12, 108208 Owen, 0.E., Morgan, A. P., Kemp, H. G., Sullivan, J. N., Herrera, M. G. & Cahill, G. F. (1967)J.Clin.Znvest. 46,1589-1595 Owen, 0.E., Felig, P., Morgan, A. P., Wahren, J. & Cahill, G. F. (1969)J. Clin. Invest. 48,474-583 Ozand, P. T., Reed, W. D., Givard, J., Hawkins, R. L., Collins, R. M., Tildon, J. T. & Cornblath, M. (1977)Biochem. J. 164,557-564 Ozand, P. T., Reed, W. D., Hawkins, R. L., Stevenson, J. H., Tildon, J. T. & Cornblath, M. (1978)Biochem. J. 170,583-591 Palaiologos, G. & Felig, P. (1976)Biochem. J. 154,709-716 Pardridge, W. M. & Davidson, M. B. (1979)Biochim. Biophys. Acta 585,34-42 Pozefsky, T. & Tancredi, R. G. (1972)J.Clin. Invest. 51,2359-2369 Pitts, R. F. (1964)Am. J. Med. 36,720-742 Vol. 8 213 Ross, B. D., Hems, R.. & Krebs, H. A. (1967)Biochem. J. 102, 94295 1 Rowsell, E.V. (1956)Biochem. J. 64,246-252 Rowsell. E. V. & Corbett, K. (1958)Biochem. J. 70,7~ Ruderman, N. B. (1975)Annu. Rev. Med. 26,245-258 Ruderman, N. B. & Berger, M. (1974)J. Biol. Chem. 249,5500-5506 Ruderman, N. B., Ross, P. S., Berger, M. & Goodman, M. N. (1974) Biochem. J. 138, 1-10 Ruderman, N. B., Schmahl, F. W. & Goodman, M. N. (1977)Am. J. Physiol. 233,E109-Ell4 Safer, B. & Williamson, J. R. (1973)J.Biol. Chem. 248,2570-2579 Sherwin, R. S., Hendler, R. G. & Felig, P. (1975)J. Clin. Invest. 55, 1382-1 390 Shinnick, F. L. & Harper, A. E. (1977)J.Nutr. 107,887-895 Snell, K. (1976)Biochem. SOC.Trans. 4,287-288 Snell, K. (1975)in Normal and Pathological Development of Energy Metabolism (Hommes, F. A. & Van den Berg, C. J., eds.), pp. 7795,Academic Press, New York Snell, K. (1978)Biochem. SOC.Trans. 6,157-159 Snell, K. (1979)Trends Biochem. Sci. 4, 124-128 Snell, K. & Duff, D. A. (19770)Biochem. J. 162,339-403 Snell, K. & Duff, D. A. (19776)Biochem. Biophys. Res. Commun. 77, 925-931 Snell, K. & Duff, D. A. (1979)Znt. J. Biochem. 10,423-426 Spydevold, O., Davis, E. J. & Bremer, J. (1976)Eur. J. Biochem. 71, 155- 165 Stacpoole, P. W. & Felts, J. M. (1970)Metab. Clin. Exp. 19,7 1-78 Sugden, M. C., Sharples, S. C. & Randle, P. J. (1976)Biochem. J. 160, 817-8 19 Taegtmeyer, H., Peterson, M. B., Ragavan, V. V., Ferguson, A. G. & Lesch, M. (1977)J.Biol. Chem. 252,5010-5018 Taylor, R. T., Shakespeare, V. & Jenkins, W. T. (1970)J. Biol. Chem. 245,4880-4885 Wahren, J., Felig, P., Cerasi, E. & Luft, R. (1972)J. Clin. Invest. 51, 1870-1878 Wahren, J., Felig, P., Havel, R., Jorfeldt, L., Pernow, B. & Saltin, B. (1973)N. Engl. J. Med. 288, 774-777 Wahren, J., Felig, P. & Hagenfeldt, L. (1976)J. Clin. Invest. 57,987999 Watford, M., Lund, P. & Krebs, H. A. (1979)Biochem. J. 178, 589596 Windmueller, H. G. & Spaeth, A. E. (1974)J. Biol. Chem. 249,50705079 Windmueller, H. G. & Spaeth, A. E. (1975)Arch. Biochem. Biophys. 171,662-672 Windmueller, H. G. & Spaeth, A. E. (1978)J.Biol. Chem. 253,69-76 Wise, J. K., Hendler, R. & Felig, P. (1972)Science 178,5 13-5 14 Wise, J. K., Hendler, R. & Felig, P. (1973a)N. Engl. J. Med. 288,487490 Wise, J. K.,Lyall, S. S., Hendler, R. & Felig, P. (1973b)J.Clin. Endocrinol. Metab. 37,34 1-344