* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download independent work of the students
Survey
Document related concepts
Neuroendocrine tumor wikipedia , lookup
Metabolic syndrome wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Hypothyroidism wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Graves' disease wikipedia , lookup
Hyperandrogenism wikipedia , lookup
Diabetic ketoacidosis wikipedia , lookup
Hypothalamus wikipedia , lookup
Pituitary apoplexy wikipedia , lookup
Complications of diabetes mellitus wikipedia , lookup
Diabetes in dogs wikipedia , lookup
Transcript
Bukovinian State Medical University
Department of Developmental Pediatrics
METHODICAL INSTRUCTIONS
to the practical class for medical students of 3-rd years
Modul 1: Child’s development
Submodul 2:
Topic 4:
Subject: PHYSIOLOGICOANATOMICAL PECULIRIATIES OF
ENDOCRINE SYSTEM. METHODICS OF ENDOCRINE
GLANDS INVESTIGATION. SEMIOTICS OF HYPOAND HYPERFUNCTION OF SOME ENDOCRINE
GLANDS. TAKING CARE OF THE CHILDREN WITH
THE DISEASES OF THE ENDOCRINE SYSTEM
It is completed by:
MD, MSc, PhD Strynadko Maryna
Chernivtsy – 2007
SUBJECT: Developmental Pediatrics.
TOPIC:
OBJECTIVES:
PROFESSIONAL MOTIVATION:
BASIC LEVEL: Basic knowledge of pediatrics.
INTEGRATED SKILL ACTIVITY:
1. Care of the children. 2. Anatomy. 3. Histology. 4. Pysiology.
STUDENT’S PRACTICAL SKILLS:
THE BASIC THEORETICAL ITEMS OF INFORMATION
The major chemical regulators of the body are the internal secretions and their
secreting cells, which are collectively known as the endocrine system.
Ordinarily the endocrine system of the newborn is adequately developed, but
its functions are immature. For example, the posterior lobe of the pituitary gland
produces limited quantities of antidiuretic hormone (ADH), or vasopressin, which
inhibits diuresis. This renders the neonate highly susceptible to dehydration.
The effect of maternal sex hormones is particularly evident in the newborn
because it causes a miniature puberty. The labia are hypertrophied, and the breasts
may be engorged and secrete milk during the first few days of life. Female
newborns sometimes have pseudomenstruation from the sudden drop in the levels
of progesterone and estrogen.
The endocrine system is adequately developed at birth,but its functions are
immature. The interrelatedness of all the endocrine organs has a major effect on
the function of any one gland. The lack of homeostatic control because of various
functional deficiencies renders the infant especially vulnerable to imbalances in
fluid and electrolytes, glucose concentration, and aminoacid metabolism.
For example, corticotropin (ACTH) is produced in limited Quantities during
infancy. ACTH acts on the adrenal cortices to produce their hormones, particularly
the glucocorticoids and aldosterone. Because the feedback mechanism between
ACTH and the adrenal cortex is immature during infancy, there is much less
tolerance for stressful conditions, which affect fluid and electrolytes and the
metabolism of fats, proteins, and carbohydrates. In addition, although the islets of
Langerhans produce insulin and glucagon during fetal life and early infancy, blood
sugar levels tend to remain labile, particularly under conditions of stress.
The function of the endocrine system is:
• to secrete intracellularly synthesized hormones into the circulation,
• to serve as pacemaker substances for metabolic processes,
• together with the closely related but more rapidly reacting nervous system,
• to serve to integrate the various physiologic functions of the organism in
adjusting to external and internal environmental demands.
Endocrine substances even in extremely small concentrations are effective in
modifying metablism, behavior, and development. The endocrine system consists
of three components:
(1) the cell, which sends a chemical message by means of a hormone;
(2) the target cells, or end organs, which receive the chemical message;
(3) the environment through which the chemical is transported (blood, lymph,
extracellular fluids) from the site of synthesis to the sites of cellular action.
Some hormones, such as acetylcholine, have specific local effects; others are
secreted by specific endocrine glands and then transported by the fluids to create
their effects on target tissues at locations distant from the secreting glands. Some
of the general hormones, such as thyroid hormone and growth hormone, affect
most cells of the body, whereas the effect of others, such as the tropic hormones, is
chiefly restricted to some specific tissues.
Fig - 1. Anterior pituitary hormones and their organs. Tropic hormones:
ACTH (adrenocorticotropic hormone); TSH (thyroid-stimulating hormone); FSH
(follicle-stimulating hormone); LH (luteinizing hormone); ICSH (male analogue of
LH); MSH (melanocyte-stimulating hormone); GH (STH) (growth hormone)
Neuroendocrine interrelationships
Homeostasis is maintained by two regulatory systems: the endocrine and the
autonomic nervous systems (also called collectively the neuroendocrine system).
The endocrine system traditionally consists of seven glands located throughout the
body. Three additional structures are also considered endocrine glands, although
for the following reasons they are not usually included. The functions of the pineal
body (epiphysis cerebri), which is located in the cranial cavity behind the midbrain
and third ventricle, are largely speculative. The thymus, located behind the sternum
and below the thyroid gland, plays an important role in immunity, but only during
fetal life and early childhood. The placenta, which secretes ovarian hormones and
chorionic gonadotropin, is only a temporary endocrine gland. The endocrine glands
secrete chemicals known as hormones directly into the bloodstream. Because the
glands have no ducts, they are sometimes called ductless glands, in contrast to
exocrine, or duct glands.
The autonomic nervous system consists of the sympathetic and
parasympathetic systems. It controls nonvoluntary functions, specifically of
smooth muscle, myocardium, and glands. The parasympathetic system is primarily
involved in regulating digestive processes, whereas the sympathetic system
functions to maintain homeostasis during stress. The higher autonomic centers,
located in the hypothalamus and limbic system, help control both sympathetic and
parasympathetic functioning. The autonomic chemical transmitters are
acetylcholine, released by cholinergic fibers, and nor-epinephrine, released by
adrenergic fibers. Neural release of norpinephrine into the plasma produces the
same effects as secretion of this substance by the adrenal medulla. This similarity
in chemical activity demonstrates the interrelatedness between the two systems.
The neuroendocrine system acts by synthesizing and releasing various
chemical substances that regulate body functions. Information is carried by means
of neural impulses in the autonomic system and by the blood in the endocrine
system. In general, neural responses are more rapid and localized; endocrine
responses are more lasting and widespread. The two systems function
synergistically because neural impulses transmitted to the central nervous system
stimulate the hypothalamus to manufacture and release several releasing or
inhibiting factors. These substances are transferred to the anterior pituitary gland,
where they lead to the release of certain tropic hormones.
Control of the endocrine system
The endocrine system controls or regulates metabolic processes governing
energy production, growth, fluid and electrolyte balance, response to stress, and
sexual reproduction. Hormones (chemical transmitters) are released by the
endocrine gland into the bloodstream, in which they are carried to tissues that are
responsive to them (target cells). The target may be another endocrine gland or an
organ or tissue. Regulation of hormonal control is based on a feedback system.
Usually the feedback control is one of negative function, which means that an
increase in one hormone results in a decrease in another substance.
The main endocrine gland controlling the release of other hormones is the
pituitary gland (hypophysis). For this reason it is often called the "master gland."
The anterior lobe of the pituitary secretes tropic (which literally means "turning")
hormones that regulate the secretion of hormones from various target organs.
Decreased levels of target cell hormones result in increased secretion of tropic
hormones. As blood concentrations of the target hormones reach normal levels, a
negative message is sent to the anterior pituitary to inhibit its production of the
tropic hormone. For example, thyroid-stimulating hormone (TSH) responds to low
levels of circulating thyroid hormone (TH). As blood levels of thyroid hormone
reach normal concentrations, a negative feedback message is sent to the anterior
pituitary, resulting in a diminished release of thyroid-stimulating hormone.
The pituitary gland is under the influence of the hypothalamus. Especially in
times of stress, the hypothalamus receives messages from the central nervous
system that result in the synthesis and secretion of certain hypothalamic chemicals
called neurosecretions or releasing factors. These chemicals are transported by way
of the pituitary portal system to the anterior pituitary, where they stimulate the
secretion of tropic hormones. An example of this is the secretion of corticotropinreleasing factor (CRF) by the hypothalamus, which stimulates the pituitary to
secrete adrenocorticotropic hormone (ACTH). In this instance the anterior pituitary
is the target of the hypothalamus and secondarily effects a response from another
target gland, the adrenals. The adrenals in turn secrete glucocorticoids, which have
multiple target sites throughout the body.
Not all hormones are dependent on other hormones for their release. For
example, insulin production depends on blood glucose concentrations. Other
hormones not under the control of the pituitary gland are glucagon, parathyroid
hormone (PTH), antidiuretic hormone (ADH), and aldosterone.
Because of the interdependent relationship of these glands, a malfunction in
one gland produces effects elsewhere in the body. Endocrine dysfunction may
result because of an intrinsic defect in the target gland (primary) or because of a
diminished or elevated level of tropic hormones (secondary). Endocrine problems
occur from hypofunction or hyperfunction of the glands. Primary hypofunction is
usually associated with a more profound deficiency of the target gland hormone
because little or no hormone is secreted. In secondary dysfunction the target glands
secrete some of their hormones but in smaller amounts and less rapidly.
Hyperfunction may be the result of an increase in the tropic hormones (primary)
with a consequent increase in the target gland hormones (secondary) or a
hypersecretion of the target glands.
The major hormones that promote physical growth are thyroid hormone,
growth hormone, and sex hormones. Insulin can be said to promote growth by its
effect on carbohydrate metabolism, whereas cortisol inhibits growth. Therefore,
deficiencies of growth-promoting hormones or an excess of cortisol can cause
growth retardation in children. Endocrine deficiencies can be the result of
abnormal secretory function in the glands responsible for their production, the
pituitary hormones that stimulate their secretion; or the releasing factors from the
hypothalamus. In some instances growth retardation may be the result of increased
production of factors that inhibit hormone secretion.
Thyroid hormone deficiency. Thyroid hormone deficiency is always
associated with poor growth and delayed bone maturation. Hypothyroidism that is
present from birth causes severe stunting of linear growth, which is evident early in
life. When the deficiency begins before the skeletal age of 9 or 10 years, the child
maintains infantile proportions with short legs compared to the length of the spine;
he tends to be pale, sluggish, inactive, and obese; and intellectual achievement at
school deteriorates. Acquired hypothyroidism varies with the degree and duration
of the deficiency, but skeletal age is delayed if the condition has been present more
than 12 months.
Growth hormone deficiency. Growth hormone deficiency, associated with
hypopituitarism, inhibits somatic growth in all cells of the body. Although children
with hypopituitarism are normal at birth, they show growth patterns that
progressively deviate from the normal growth rate, often beginning in infancy. The
chief complaint
in most instances is short stature. Of those who seek help, boys outnumber
girls three to one. Skeletal proportions are normal for the age, but these children
appear younger than their chronologic age, tend to be relatively inactive,and are
less apt to participate in aggressive, sporting type activities. Bone age is nearly
always retarded but is closely related to height age; the degree of retardation
depends on the duration and extent of the hormonal deficiency. Diminished
function of recent onset may show little retardation in skeletal age, whereas
children with a long-standing deficiency may evidence a skeletal age only 40% to
50% of their chronologic age. In children with a partial growth hormone
deficiency, the growth retardation is less marked than in children with a growth
hormone deficiency.
Growth hormone deficiency may be attributed to an idipathic or organic
etiology. The extent of idiopathic growth hormone deficiency may be complete or
partial, but the cause is unknown. It is frequently associated with other pituitary
hormone deficiences, such as deficiences of thyroid-stimulating hormone and
ACTH; thus it is theorized that the disorder is probably secondary to hypothalamic
deficiency. It has also been observed that there is a higher than average frequency
in some families,which indicates a possible genetic etiology in a number of
instances.
The most common organic causes of growth hormone deficiency are tumors
of the pituitary or hypothalamic region, in which case the child may evidence
growth retardation for quite some time before developing any symptoms or signs
of increased intracranial pressure, local compression, or destructive effects of the
tumor. Other causes sometimes include encephalitis, head trauma (rarely), and
congenital hypoplasia of the hypothalamic area.
Sex hormone deficiency. Sex hormone deficiency that causes delayed
puberty can occur as a result either of pituitary dysfunction or of hypogonadism. A
hypofunctioning pituitary gland, as briefly discussed in the preceding segment on
endocrine dysfunction, can produce a deficiency in either the gonadotropic
hormones, which retards maturation of the gonads, or growth hormone, which will
diminish total growth during childhood. In addition, there are a large variety of
disorders that cause absence or deficiency of sex hormone secretion by their effect
on the gonads directly. These may be genital abnormalities that are related to
defective gonadal differentiation or those that are associated with functional
abnormalities of the already differentiated fetal gonad. The largest group of
disorders in which deficient gonadal development is a prominent feature includes
the sex chromosomal aberrations, e.g. Klinefelter's and Turner's syndromes.
Cortisol excess. Cortisol excess as a result of organic causes or of prolonged
cortisone therapy also has an adverse effect on growth in children. This effect is
produced by direct action on growing cartilage, interference with production of
growth hormone, or interference with the response to or production of
somatomedin. Because of the growth-suppressing effect of cortisone in excess of
minimal requirements, therapy is limited to short-term administration whenever
possible.
Syndromes of primary gonadal failure. The most frequently seen disorders
associated with primary gonadal failure are the sex chromosomal defects
categorized collectively as gonadal dysgenesis, principally Turner's syndrome.
Chromosomal impairment of male sexual function is most commonly caused by
Klinefelter's syndrome. Derangements that become apparent at puberty are more
common. Clinical presentation in the female may be masculinization, sexual
infantilism or hypoplasia, primary absence of menstruation (amenorrhea), or
abnormally scanty or infrequent menstruation (oligomenorrhea or hypomenorrhea).
Psychosocial dwarfism. Psychosocial, or deprivation, dwarfism is a term
applied to children who are significantly retarded in growth because of
environmental circumstances. Children from homes in which they receive little, if
any, psychosocial stimulation display markedly delayed skeletal development, and
various tests in these children for growth hormone release are consistent with those
that indicate a pituitary dysfunction. When these children are removed from the
deprived environment, their growth proceeds at a normal or increased rate. This
has been repeatedly demonstrated in infants and very young children. Some
investigations attribute the growth retardation to malnutrition. Although this may
be a factor in infants, it may also be a contributing factor in adolescents with short
stature and delayed puberty secondary to psychosocial factors, particularly in the
loss of appetite related to the disorder anorexia nervosa.
Although the mechanism is not entirely clear, it is hypothesized that
deprivation dwarfism occurs as a response to increased cortisol secretion that
results from the prolonged stress of a disturbed environment or unsettled patterns
of sleep. Evidence indicates that deprivation dwarfism is also associated with sleep
abnormalities. Since growth hormone is secreted in largest amounts during sleep, it
follows that anything interfering with normal sleep patterns will interfere with the
hormone secretion.
"For each anterior pituitary hormone there is a corresponding hypothalamic
releasing factor. A deficiency in these factors caused by inhibiting anterior
pituitary
hormone synthesis produces the same effects (see text for more detailed
information).
In the male, LH is sometimes known as interstitial cell-stimulating hormone
(ICSH).
Disorders of pituitary function. The pituitary gland (hypophysis) actually
consists of two separate glands: the anterior pituitary (adenohypophysis) and the
posterior pituitary (neurohypophysis). Since each of these lobes secretes different
hormones, they are discussed separately. In general the more common pituitary
disorders during childhood affect one lobe rather than both.
The anterior pituitary secretes seven hormones: growth hormone (GH),
adrenocorticotropic hormone (ACTH), thyrotropin or thyroid-stimulating hormone
(TSH), two gonadotropins - follicle-stimulating hormone (FSH) and luteinizing
hormone (LH) in females or interstitial cell-stimulating hormone (ICSH) in males,
prolactin, and melanocyte-stim-ulating hormone (MSH). With the exception of
melanocyte-stimuiating hormone, each of these hormones controls somatic and
sexual development.
Growth hormone or somatotropin. Growth hormone promotes growth of
bone and soft tissues without affecting sexual development. Its direct effect on
protein anabolism promotes cellular growth. It accelerates fat catabolism and
utilization for energy. Although its exact effect on carbohydrate metabolism is not
known, it tends to increase the blood glucose concentration a hyperglycemic
response.
The secretion of growth hormone is under the influence of somatotropinreleasing factor (SRF) from the hypothalamus. Hyposecretion of growth hormone
during the years of skeletal growth results in a condition called dwarfism. If it
occurs after epiphyseal closure (during late adolescence) it causes a rare condition
known as Simmonds' disease (pituitary cachexia). Hypersecretion during the years
of active bone growth produces gigantism, whereas excess growth hormone during
adult life results in acrotnegaly.
Criteria for diagnosis of GHD
• Height below 3rd percentile
• Prepubertal growth velocity less than 4 cm per year.
• Bone age below the chronological age.
• Abnormal 24-hour GH secretory pattern.
• Peak GH levels less than 10 ng/ml during provocative stimulation tests.
• Low IGF-1 and IGFBP-3 levels for age.
• Resumption of growth following GH administration.
Acromegaly main symptoms
• weakness
• enlargement of the distal parts of the body
• thickening of facial features
• widening of the fingers
• hypogonadism
• narrower field of vision
• increase of the level of somatotropin hormone in the plasma
• excessive hairiness
Adrenocorticotropic hormone. The main function of adreno-corticotropic
hormone is to control the adrenal gland's secretion of the glucocorticoids and, to a
lesser extent, of androgen. The control of adrenocorticotropic hormone secretion is
under the influence of the hypothalamic chemical corticotropin-releasing factor.
Hyposecretion or hypersecretion of adrenocorticotropic hormone results in clinical
manifestations directly attributable to a lack or excess of hormones from the target
gland, the adrenal cortex.
Adison disease
• brown colour of the skin
• progressive fatigue
• loss of weight
• anerexia
• loss of blood pressure
• anemia
Thyrotropin or thyroid-stimulating hormone. As its name implies, thyroidstimulating hormone promotes and maintains growth of the thyroid gland and
stimulates its secretion of thyroid hormone (thyroxine and triiodo-thyronine). The
secretion of thyroid-stimulating hormone is controlled by thyro-tropin-releasing
factor (TRF) from the hypothalamus. Hyposecretion or hypersecretion of thyroidstimulating hormone produces symptoms directly attributable to a lack or excess of
thyroid hormone.
Gonadotropic hormones. The gonadotropic hormones follicle-stimulating
hormone, luteinizing hormone, interstitial cell-stimulating hormone, and prolactin
are responsible for the growth and maturation of the gonads at puberty and for the
ongoing stimulation of germ cell production during adulthood. The function of
these hormones is discussed in relation to puberty and will not be elaborated here.
Disorders of thyroid function
Etiological classification of goiter
1. Physiologic: puberty goiter.
2. Inflammatory: acute suppurative thyroditis, subacute viral thyroditis.
3. Autoimmune: graves disease, chronic lymphocytic thyroditis.
Fig. 2. Regulation of thyroid hormone secretion.
4. Dysgenetic: thyroglossal duct cyst, ectopic thyroid gland, agenesis of one
lobe.
5. Compensatory: dyshormonogenesis, iodine deficiency (endemic), drug
induced.
6. Neoplastic: Benign-adenoma, teratoma; malignant- carcinoma.
7. Colloid goiter.
Estimation of thyroid size by palpation
STAGE 0: no goiter
STAGE 1-a: goiter detectable only by palpation and not visible even when the
neck is fully extended.
STAGE 1-b: goiter palpable but visible only when the neck is fully extended.
STAGE 2: goiter visible when the neck is in normal position; palpation not
needed for diagnosis.
STAGE 3: very large goiter, which can be recognize at a considerable
distance.
Technique of palpation of thyroid gland
Thyroid gland is an endocrinal gland that is situated on the anterior surface of
neck, so it is easy to palpate it.
• During palpation the doctor stands at the back of the child.
• Put the fingers onto the front side of the musculus sterno-cleidomastoideus
of the same side.
• Find soft mass of the gland under skin with gentle moving.
• Ask the child to make swallow moving for more clear feeling of the gland.
• Make assessment of the gland according to such criteria:
- painful or not;
- smooth or not;
- consistency: soft, elastic, hard;
- movable or not;
- size: what is palpable - isthmus, lobes, their sizes.
The thyroid gland secretes two types of hormones: thyroid hormone and
thyrocalcitonin. Thyroid hormone actually consists of two hormones: thyroxine
(T4) and triiodothyronine (T3). The synthesis of these hormones depends on
available sources of dietary iodine and tyrosine. The thyroid is the only endocrine
gland capable of storing excess amounts of the hormone and releasing it as needed
for oxi-dative purposes. During circulation in the bloodstream thyroxine and
triiodothyronine are bound to carrier proteins (thyroxine-binding globulin [TBG]).
They must be unbound before they are able to exert their metabolic effect.
The main physiologic action of thyroid hormone is to regulate the basal
metabolic rate and thereby control the processes of growth and tissue
differentiation, as outlined in the following list.
Physiologic effects of thyroid hormone
• Regulates metabolic rate of all cells; protein, fat, and carbohydrate
catabolism; and nitrogen excretion
• Regulates body heat production and heat-dissipating mechanisms
• Regulates protein synthesis and catabolism, ammoacid incorporation into
protein, and transcription of messenger RNA
• Increases gluconeogenesis and peripheral utilization of glucose
• Maintains appetite and secretion of gastrointestinal substances
• Maintains calcium mobilization
• Stimulates cholesterol synthesis and hepatic mechanisms that remove
cholesterol from the circulation; stimulates lipid turnover and free fatty acid release
• Regulates hepatic conversion of carotene to vitamin A
• Maintains growth hormone secretion, skeletal maturation, and tissue
differentiation
• Is necessary for muscle tone and vigor and normal skin constituents
• Maintains cardiac rate, force, and output
• Affects respiratory rate, depth of oxygen utilization, and carbon dioxide
formation
• Affects central nervous system development and cerebration during first 2 to
3 years
• Affects milk production during lactation and menstrual cycle fertility
• Maintains sensitivity to insulin and insulin degradation
• Affects red cell production
• Affects cortisol secretion, probably caused by direct effect on adrenal glands
and by increasing ACTH secretion
Unlike somatotropin, thyroid hormone is involved in many more diverse
activities influencing the growth and development of body tissues. Therefore a
deficiency of thyroid hormone exerts a more profound effect on growth than that
seen in pituitary dwarfism.
The secretion of thyroid hormone is controlled by thyroid-stimulating
hormone of the anterior pituitary, which in turn is regulated by the hypothalamic
thyrotropin-releasing factor (TRF). This negative feedback mechanism follows the
same principles as were described earlier. Consequently hypothyroidism or
hyperthyroidism may result from a defect in the target gland or from a disturbance
in the secretion of thyroid-stimulating hormone or thyrotropin-releasing factor.
Thyrocalcitonin helps maintain blood calcium levels by decreasing the
calcium concentration. Its effect is opposite that of parathormone, in that it inhibits
skeletal demineralization and promotes calcium deposition in the bone.
THYROID HYPOFUNCTION
Hypothyroidism is one of the most common endocrine problems of
childhood. It may be either congenital, such as in cretinism, or acquired,such as
from autoimmunization (Hashimoto's thyroiditis). Hypothyroidism from dietary
insufficiency of iodine is now rare because the use of iodized salt has permitted a
readily available source of the nutrient.
Congenital hypothyroidism (cretinism)
Cretinism is usually caused by failure of embryonic development of the
thyroid gland, but it may also be a result of inborn enzymatic defects in the
synthesis of thyroxine. The seventy of the disorder depends on the amount of
thyroid tissue present. Usually the neonate does not exhibit obvious signs of
hypothyroidism, probably because of the exogenous source of thyroid hormone
supplied by means of the maternal circulation. Manifestations are delayed in
breast-fed infants. In another type of cretinism, transfer of goitrogens (substances
that can induce a goiter), such as the antithyroid drugs phenylbutazone,
paraaminosalicylic acid, and cobalt, may inhibit thyroid secretion, thereby
resulting in congenital cretinism. Although the latter is self-limiting, it is a
potentially fatal condition because once the maternal supply is terminated the
infant's thyroid is unable to produce its own hormones. In addition, a large goiter in
a neonate may cause total obstruction of the airway.
Clinical manifestations of congenital hypothyroidism
The symptoms of cretinism usually become apparent by 3 to 6 months of age
in bottle-fed infants. However, before this time the earliest symptoms indicating
hypothyroidism include prolonged physiologic jaundice, feeding difficulties,
inactivity (excessive sleeping and minimal crying), anemia, and problems resulting
from hypotonic , abdominal musculature, such as constipation, diastasis recti,
protruding abdomen, and umbilical hernia. The behavioral characteristics often
lead parents to describe the infant as exceptionally "quiet and good."
Impaired development of the nervous system leads to mental retardation. The
severity of the intellectual deficit is related to the degree of hypothyroidism and the
duration of the condition before treatment. Other nervous system manifestations
include slow, awkward movements, somnolence, lethargy, and abnormal deep
tendon reflexes (often referred to as "hung-up" because the relaxation phase after
the contraction is slow).
Because skeletal growth is severely stunted, the child is short. Unlike pituitary
dwarfism, infantile proportions persist in that the length of the trunk remains long
in relation to the legs. The decreased metabolic rate results in weight gain and
often leads to obesity. Characteristic infantile facial features from myxedema
include a short forehead, wide, puffy eyes, wrinkled eyelids, broad, short upturned
nose, and a large protruding tongue. The hair is often dry, brittle, or lusterless and
follows a low hairline. Dentition is delayed and usually defective. Such facial
features give the child a characteristic dull exnression-The skin is yellowish from
carotenemia as a result of the depressed hepatic conversion of carotene to vitamin
A. Loss of heat from reduced metabolism is reflected in a cool skin. Cold
intolerance is another -common consequence. Anemia results in pallor, fatigue, and
lethargy, and vitamin A deficiency causes thickened, coarse, dry, scaly skin.
The cardiovascular changes are slow pulse, decreased circulation, mottling,
and decreased pulse pressure. The decreased cardiac rate and output are directly
related to the decreased oxygen requirements from a low metabolic rate.
Respiratory changes include exertional dyspnea and decreased respiratory effort.
In breast-fed infants the clinical manifestations may be delayed until the child
is weaned, at which time the facial features, skin and hair changes, growth
retardation, muscular hypotonia, and cardiovascular alterations become evident.
Because breast milk contains suboptimum amounts of thyroid hormone, bone age
is greatly retarded, usually comparable to that of a newborn. Significantly,
however, intellectual functioning remains near normal.
Diagnostic evaluation
Several tests are available to assess thyroid activity:
• measurement of protein-bound iodine (PBI),
• measurement of free thyroxine,
• measurement of thyroid-stimulating hormone,
• measurement of
thyrotropin-releasing factor, radioimmu-noassay of
thyroxine and triiodothyronine.
These tests measure the amount of thyroid hormone secreted and the
intactness of the homeostatic mechanisms.
Tests of thyroid gland function usually involve an oral infusion of a
radioactive isotope of iodine131 and measurement of the iodine uptake by the
thyroid, usually within 24 hours. In congenital cretinism protein-bound iodine,
thyroxine, triiodothyronine, and free thyroxine levels are low and thyroid uptake of
Iod131 is decreased. Neonatal screening is now possible with a highly sensitive
and specific radioimmunoassay for thyroxine and thyroid-stimulating factor and is
mandatory in most states. Diagnosis rests on the detection of a high serum level of
thyroid-stimulating factor and a low level of thyroxine during the early days of life.
Roentgenography is employed to assess bone age.
Therapeutic management
Treatment involves indefinite replacement therapy with desiccated thyroid to
abolish all signs of hypothyroidism and reestablish normal physical and mental
development. If adequate thyroid hormone replacement is begun before 3 months
of age, the chance for completely normal growth is possible and the chance for a
normal intelligence quotient is increased. To avoid the risk of overdosage of
thyroid hormones, regular evaluations of thyroxine and triiodothyronine levels
should be assessed. Bone age surveys are also done to ensure optimum growth.
DIABETES MELLITUS
Etiology
Heredity is unquestioned as a prominent factor in the etiology of diabetes
mellitus, although the mechanism of inheritance is unknown. Diabetes may be
actually a syndrome rather than a specific disease. A variety of genetic
mechanisms have been proposed, but most favor a multifactorial inheritance or a
recessive gene somehow linked to the tissue-typing antigens, the human
lymphocyte-A (HLA) system. However, the inheritance of noninsulin-dependent
diabetes and insulin-dependent diabetes appears to be different. Nearly 100% of
offspring of parents who both have noninsulin-dependent diabetes develop that
type of diabetes, but only 45% to 60% of the offspring of both parents who have
insulin-dependent diabetes will develop the disease. There is also an increased risk
of diabetes with obesity. The incidence of the disease doubles with every 20% of
excess weight, and this figure applies to the young as well as to the older diabetic
person. Diabetes is now the sixth leading cause of death by disease in adults and
the first leading cause of new cases of blindness between 20 and 75 years of age.
Vimses have been implicated in the etiology of diabetes. The viral theory states
that the p-cells of some individuals (most specialists believe that the p-cells are
genetically susceptible because of the defects in the HLA system) are attacked by
certain viruses, causing cell damage or death. The body reacts to this damaged or
changed tissue in an autoimmune phenomenon, forming antibodies that "attack"
the p-cells, resulting in cell death. When there are not enough available (3-cells to
supply sufficient insulin to meet the needs of the body, insulin-dependent diabetes
results. Tumors of the pancreas, pancreatitis, stress drugs such as steroids, stress
diseases that involve other endocrine organs such as acromegaly, heredity, and
viral diseases are now believed to play a part in causing diabetes.
In noninsulin-dependent, or type II, diabetes disturbed carbohydrate
metabolism may be a result of a sluggish or insensitive secretory response in the
pancreas or a defect in body tissues that requires unusual amounts of insulin, or the
insulin secreted may be rapidly destroyed, inhibited, or in-activated in affected
persons. A lack of insulin because of reduction in islet cell mass or destruction of
the islets is the hallmark of the person with insulin-dependent, or type I, diabetes.
Pathophysiology
Insulin is needed to support the metabolism of carbohydrates, fats, and
proteins, primarily by facilitating the entry of these substances into the cell. Insulin
is needed for the entry of glucose into the muscle and fat cells, for the prevention
of mobilization of fats from fat cells, and for storage of glucose as glycogen in the
cells of liver and muscle. Insulin is not needed for the entry of glucose into nerve
cells or vascular tissue. The chemical composition and molecular structure of
insulin are such that it fits into receptor sites on the cell membrane. Here it initiates
a sequence of poorly defined chemical reactions that alter the cell membrane to
facilitate the entry of glucose into the cell and stimulate enzymatic systems outside
the cell that metabolize the glucose for energy production.
With a deficiency of insulin, glucose is unable to enter the cell and its
concentration in the bloodstream increases. The increased concentration of glucose
(hyperglycemia) produces an osmotic gradient that causes the movement of body
fluid from the intracellular space to the extracellular space and into the glomerular
filtrate in oder to "dilute" the hyperosmolar filtrate. When the glucose
concentration in glomerular filtrate exceeds the threshold (180 mg/ dl), glucose
"spills" into the urine along with an osmotic diversion of water (polyuria), a
cardinal sign of diabetes. The urinary fluid losses cause the excessive thirst
(polydipsia) observed in diabetes. As might be expected, this water washout results
in a depletion of other essential chemicals.
Ketoacidosis. When insulin is deficient, glucose is unavailable {or cellular
metabolism and the body chooses alternate sources of fuel,principally fat.
Consequently fats break down into fatty acids and glycerol in the fat cells and in
the liver and are converted to ketone bodies (3-hydroxybutyric acid, acetoacetic
acid, acetone). The ketone bodies are used as the alternative to glucose as a source
of fuel but are utilized in the cells at a limited rate. Any excess is expelled in the
urine (ketonuria) or the lungs (acetone breath).
Protein is also wasted during insulin deficiency. Since glucose is unable to
enter the cells, protein is broken down and converted to glucose by the liver
(glucogenesis), which glucose further contributes to the hyperglycemia. These
mechanisms are similar to those seen in starvation when substrate (glucose) is
absent. The body is actually in a state of starvation during insulin deficiency.
Without the use of carbohydrates for energy, fat and protein stores are depleted as
the body attempts to meet its energy needs. The hunger mechanism is triggered,
but the increased food intake (polyphagia) enhances the problem by further
elevating the blood glucose.
Ketones are organic acids that readily produce excessive quantities of free
hydrogen ions, causing a fall in plasma pH. Chemical buffers in the plasma,
principally bicarbonate, combine with the hydrogen ions to form carbonic acid,
which readily dissociates into water and carbon dioxide. The respiratory system
attempts to eliminate the excess carbon dioxide by increased depth and rate Kussmaul's respirations, the hyperventilation characteristic of metabolic acidosis.
The ketones are buffered by sodium and potassium in the plasma. The kidney
attempts to compensate for the increased pH by increasing tubular secretion of
hydrogen and ammonium ions in exchange for fixed base, thus depleting the base
buffer concentration.
Potassium is also a problem and was once the cause of unexplained deaths
shortly after insulin therapy was instituted. With cellular death, potassium is
released from the cell into the bloodstream and excreted by the kidney where the
loss is accelerated by the osmotic diuresis. The total body potassium is then
decreased, even though the serum potassium level may be elevated as a result of
the decreased fluid volume in which it circulates. Alteration in serum and tissue
potassium can make cardiac arrest a potential problem.
If these conditions are not reversed by insulin therapy in combination with
correction of the fluid deficiency and electrolyte imbalance, progressive
deterioration occurs with dehydration, electrolyte imbalance, acidosis, coma, and
death. Diabetic ketoacidosis should be diagnosed promptly in a seriously ill patient
and therapy instituted.
Long-term pathologic conditions. The problems that shorten life in the
individual with diabetes are related to damage to the vascular and nervous system
(retinopathy, nephropathy, neuropathy). There has for some time existed a major
controversy as to whether the long-term problems of diabetes are a concomitant of
the disease, genetically predetermined and unalterable by control of the blood
glucose, or whether they are complications somehow related to the reduction of
insulin and/ or hyperglycemia and are thus preventable by careful and meticulous
control of the blood glucose level (the more accepted therapy).
With poor diabetic control vascular changes appear as early as 2,5 to 3 years
after diagnosis; however, with good to excellent control, changes have been
postponed for 20 or more years. Changes before puberty are uncommon, but after
puberty the poorer the control, the more rapid the vascular changes, with kidney
damage, blindness, and neuropathy. The damage in the young diabetic person is to
the small blood vessels (microangiopathy), and it has been demonstrated that the
elevated blood glucose level - not the genetics - causes the vascular disease.
Clinical manifestations
The symptomatology of diabetes is more readily recognizable in children than
in adults, so it is surprising that the diagnosis may sometimes be missed or
delayed. Diabetes is a great imitator: influenza, gastroenteritis, and appendicitis are
the conditions most often diagnosed, only to find that the disease was really
diabetes. Those families with a strong family history of diabetes should suspect
diabetes, especially if there is one child in the family with diabetes. Main
manifestations are:
• polyuria
• polydipsia
• polyphagia
• progressive cachexia
• glucosuria
• hyperglicemia
• increasing of specific gravity of urine
The sequence of chemical events described previously results in
hyperglycemia and acidosis, which in turn produce the three "polys" of diabetes polyphagia, polydipsia, and polyuria - the cardinal symptoms of the disease. In
noninsulin-dependent diabetes (which has also been found in older children), the
insulin values are found to be elevated, 80% to 90% of this population have been
found to be overweight, and there is often tiredness and frequent infections (such
as monilial infections in females).
The insulin-dependent diabetic has markedly decreased insulin levels and, as
diabetes becomes complete, there is no demonstrable insulin at all. The child may
start wetting the bed, become grouchy and "not himself," or act overly tired.
Abdominal discomfort is common. Weight loss, though quite observable on the
charts, maybe a less frequent presenting complaint because of the fact that the
family might not have noticed the change. Another outstanding feature of diabetes
is thirst. One couple reported that their child, during a trip from California to
Kansas, drank the contents of a gallon jug of water between each gas station stop.
At a certain point in the illness the child may actually refuse fluid and food, adding
to the increasing state of dehydration and malnutrition. Other symptoms include
dry skin, blurred vision, and sores that are slow to heal. More commonly in
children, tiredness and bed-wetting are the chief complaints that prompt parents to
take their child to the physician.
The child may be hyperglycemic, with elevated blood glucose levels and
glucose in the urine; may be in diabetic ketosis, with ketones as well as glucose in
the urine but not noticeably dehydrated; may be in diabetic ketoacidosis, with
dehydration, electrolyte imbalance, and acidosis.
Diagnostic evaluation
Observation and testing are important to the diagnosis of diabetes in children.
If children demonstrate glycosuria, are overweight, or exhibit symptoms of
hypoglycemia, they are candidates for glucose tolerance testing.
The urine test will show positive glucose only when the disease is actually
manifest. The negative urine test does not necessarily rule out early diabetes, nor
does a positive test necessarily indicate diabetes. Renal glycosuria, unrelated to
diabetes, can result in glucose in the urine.
The fasting blood glucose test may miss the diagnosis of early diabetes and
has been known to miss as many as 85 % of children who had an abnormal glucose
tolerance test with asymptomatic disease. The 4-hour glucose tolerance test has
been found to be the most useful test for the diagnosis of early diabetes, whereas
the 6-hour glucose tolerance test is most helpful for the diagnosis of hypoglycemia.
Based on norms established for normal, nondiabetic children of various ages, the
criterion for the diagnosis of early diabetes is two or more abnormal tests with two
or more values in each test that are outside the normal range. However,
standardization of food intake before the test may be important and those preparing
for the test should emphasize the importance of following the directions for diet
supplied by the physician or laboratory. It is difficult to do glucose tolerance
testing in children younger than 3 years of age, since norms for children in this
age-group have not been established.
Problem of diagnosis. Signs, symptoms, and chemical tests may lead to the
conclusion that the child has diabetes, when in reality another condition may be
present. This is true in salicylate intoxication, which can be ruled out easily by
boiling the urine. The acetone, if present, will boil out of the urine, leaving a
negative Acetest if related to diabetes and a positive Acetest if related to salicylate
intoxication. Temporary hyperglycemia may accompany such stressful conditions
as bums, hyperalimentation, pancreatitis, and encephalitis. The glucose tests
usually return to normal once the stress is reversed; however, insulin may be
needed for a short period in the stress illnesses, especially when the child is
undergoing hyperalimentation. Other abnormal conditions that may cause glucose
to appear in the urine are certain renal diseases, some other endocrine disorders
such as hypercortisolism, and lead encephalopathy.
Therapeutic management: insulin
The management program for any child with diabetes mellitus should involve
flexibility and 24-hour insulin coverage and should be able to fit into the child's
life-style. The insulin treatment should be determined by the recognition that the
effective duration of action of insulin in children may be somewhat different from
that in adults. Xhe effective action of insulin is described as the effect of a certain
amount of insulin in lowering the blood glucose level over a period of time. Ideally
the blood glucose level is maintained at less than 140 mg/dl and no lower than 60
mg/dl during the time of specific action of the insulin, based on past information
regarding the duration of action of the intermediate-acting insulins. The accepted
duration of action of intermediate-acting insulins is 24 hours or more, but in
insulin-dependent children it does not appear to be the case. The duration of
effective action for intermediate-acting insulin has been found to be 12 to 14 hours.
Lente insulin is the longest acting of the intermediate-acting insulins, but even it
lasts only 14 to 16 hours.
In working with these insulins, it is wise to remember that lente insulin is
30% semilente and 70% ultralente. Lente insulins that mix with no other insulins
other than regular derive their action from the size and number of crystals - small
and numerous crystals = semilente insulin; large and less numerous crystals =
ultralente insulin. Protamine zinc insulin (PZI) is seldom used today because of its
very long duration of action and its very low tissue insulin levels, which may not
saturate receptor sites on the cell membrane sufficiently well to effectively help the
body utilize the glucose that may be present. The potential overlap of insulin action
is unsuited for children, who are active one minute and very inactive the next. The
balance that needs to be achieved between insulin, diet, and activity is most
difficult when using this type of insulin. The intermediate-acting insulins (other
than lente insulin) derive their delayed action from a protein tag. The most
commonly used insulins are the intermediate-acting insulins, principally isophane,
which are usually given in a single early morning dose combined with a small
amount of short-acting insulin (usually regular).
Other types (including diabetes associated with certain conditions and
syndromes) - this category includes secondary diabetes such as steroid-induced
diabetes as well as primary diabetes associated with genetic syndromes, drug- or
chemical-induced diabetes, and diabetes resulting from pancreatectomy for
hypoglycemia. Syndromes with insulin receptor abnormality are classified in this
group.
Impaired glucose tolerance (IGT) - formerly called "asymptomatic
diabetes," "subclinical diabetes," "borderline diabetes," or "latent diabetes."
Biochemically intermediate between normal and diabetic glucose intolerance, it
probably represents a stage in the development of insulin-dependent or noninsulindependent. Because few of these individuals develop the full-blown disease, this
classification tends to remove the stigma attached to the previous designations,
which affected the child's self-concept as well as insurance and vocational efforts.
Statistical risk classes – individuals who do not have demonstrable
impairment of glucose tolerance but who:
1. Had previous abnormality of glucose tolerance (formerly labeled "latent
chemical diabetes" or "prediabetes") or spontaneous hyper-glycemia but who have
normal glucose tolerance at the time of
classification.
2. Have potential abnormality of glucose tolerance (previously termed
"prediabetes" or "potential diabetes") and includes individuals presumed to be at
risk for diabetes on genetic grounds and individuals who have circulating islet cell
antibodies.
The most common endocrine disturbance in childhood, diabetes mellitus,
caused by defective pancreatic hormone (insulin) secretion, is discussed at length.
CUSHING'S SYNDROME
Classic clinical manifestation in children include progressive central obesity,
marked failure of longitudinal growth, hirsutism, weakness, a nuchal fat pad
(buffalo hump), acne, striae, hypertension, and often hyperpigmentation (if ACTH
is elevated). The etiology can be exogenous glucocorticoid administration or
endogenous causes including adrenal adenoma, carcinoma, nodular adrenal
hyperplasia, an ACTH-secreting pituitary microadenoma, resulting in bilateral
adrenal hyperplasia, or a very rare ACTH-secriting tumor.
Spontaneous Cushing's syndrome is rare in childhood. Iatrogenic Cushing's
syndrome is more common, produceas similar clinical manifestations, and may be
induced by the use of potent glucocorticoids for chronic inflammatory, neoplastic,
and collagen-vascular disorders and for suppression of the immune response.
DIABETES INSIPIDUS
Clinical feature. The cardiaral signs of disease the are polyuria and
polydipsia. Some patient may seek medical attention for nocturnal enuresis.
Polyurea disturbs rest, sleep, play and even schooling. Appetite maybe poor.
Infants with diabetes insipidus may show hyperthermia, dehydration, electrolyte
imbalance, asotemia, dehydration and potentially circulatory collapse. Other signs
depend on the causative lesion and may include retardation, cachexia, obesity,
sleep disturbance, precocious puberty, visual disturbances and emotional disorders.
Syndromes of endocrine system disorders
1. Syndrome of growth inhibition
2. Acromegalia, gigantism
3. Syndromes of metabolism disorders
4. Syndromes of hyperfunction of endocrine gland
5. Syndromes of hypofunction of endocrine gland
6. Syndromes of hyperglycemia
7. Syndromes of hypoglycemia
8. Syndrome of mental retardation
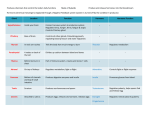
Table 1.
Sexual development of girls
Development of mammary gland
Phase
Mammary glands does not project over the surface thorax
Ма0
Glands something project, alveolla together with nipple form uniform cone Ma1
Glands much project, together with nipple and alveola have cone shape
Ma2
Glands body adopt roundinsh form, nipples rise over the alveola
Ma3
Grows of pubic hair
Absence of hair
Sporadic hair
The hair on the antral part of pubic are few and long
Hair on surface of pubic is long , curly, dense (thick)
Development of hair in axillary fossa
Phase
P0
P1
P2
P3
Absence of hair
Sporadic hair
Hair is scarce on the central part of fossa
Hair is dense, curly on the entire surface of fossa
Phase
Ax0
Ax1
Ax2
Ax3
Formation of menstrual function
Absense of menstrual cycle (menses)
1-2 menstrual cycle before examination
Irregular menstrual cycle (menses)
Regular menstrual cycle (menses)
Phase
Me 0
Me 1
Me 2
Me 3
Table 2.
Sexual development of boys
Development of hair in axillary fossa
Absence of hair
Sporadic hair
Hair is scarce on central part
Dense straight hair on the entire fossa
Dense curly hair on the entire fossa
Phase
Ax0
Ax1
Ax2
Ax3
Ax4
Grows of pubic hair
Phase
Absence of hair
Po
Sporadic hair
P1
Sparse growth of long, straight, downy and slightly pigmented hair at P2
base of penis
Hair darker, coarser and curly and spread sparsely over entire pubis
Р3
Pubic hair more abundant with curling but restricted to pubic area
P4
Hair adult in quantity and type with spread to inner surface of thighs
P5
Grows of thyroid cartilage
Phase
No signs of grows
Lo
Beginning of cartilage projection
L1
Distinct projection of Adam's-apple
L2
Change of voice timbre
Phase
"Childish voice
v0
"Mutation (creaking) of voice
v,
"Male timbre of voice
Grows of facial hair
Phase
Absence of hair
Fo
Beginning of hair grows over the upper lip
F,
Harsh hair over the upper lip and apperence of hair on the chin
F2
Spreading of hair grows over the upper lip and chin with tendency to F3
confluence, beginning on whiskers grows
Confluence of hair over the upper lip and chin, pronounced of F4
whiskers grows
Confluence of all zones of hair grows
F5
Table 13.3.
Term of sexual development
A
boys
girls
ge,
sexual formulas
sexual formulas
yr
Since
Up to
Since
Up to
1
MaoPo
Ma2Pi
0
AxoMeo
AxoMeo
1
MaiPiA
Ma2Pi
1
xoMeo
AxoMeo
1
VoPo
ViPi
MaiPoA
МазРз
2
LoAxoFo LoAxoFo xoMeo
Ах1Ме1
1
V!Po
V2P3
МагРг
МазРз
3
LoAxoFo L1AX2F0 АхоМео
АхгМез
1
V1P2
V2P3
МазРг
МазРз
4
L0AX0F0 L2AX2F, АхгМео
АхзМез
5
6
7
1
V1P4
V2P3
МазРзА
МазРз
L1AX0F0 L2AX3F2 хгМез
АхзМез
1
V2P4
V2P5
L1AX2F1 L2AX4F3
1
V2P2
V2P5
L2AX2F0 L2AX4F3
-
Stage 1 (prepubertal)
Stage 2 (pubertal)
Stage 3
Stage 4
Stage 5
Fig. 13.3. Developmental stages of secondary sex characteristics and genital
development in boys.
Stage 1 (preadolescent)
Stage 4
Stage 5
Fig. 13.4. Growth of pubic hair in girls (stages 4 and 5 are equal to P3).
Stage 2 (pubertal)
Stage 4
Stage 3
Stage 5
Fig. 13.5. Developmental of the breast in girls (stage 2 is equal to Ma,, stage 3
is equal to Ma2, stages 4 and 5 are equal to Ma3)
INDEPENDENT WORK OF THE STUDENTS:
Make a general conclusion on a theme of a class №1 and conducted practical
work.
REVIEW QUESTIONS:
TEST PROBLEMS
Situation tasks.
1.
Anatomy and physiology ROD R.SEELEY 1992 by Mosby-Year
Book.Inc.
2. Nelson Textbook of Pediatrics / edited by Richard E. Behrman, Robert
M. Kliegman, Ann M. Arvin; senior editor, Waldo E. Nelson - 15th ed. W.B.Saunders Company, 1996. - 2200 p.
3. Whaley L.F., Wong D.L.: Nursing care of infants and children, St. Louis,
Toronto, London, 1983.
REFERENCES:
1. Nursing care of Infants and Children / editor Lucille F. Whaley and I. Wong.
Donna L. - 2nd ed. - The C.V. Mosby Company. - 1983. - 1680 p.
2. Nykytyuk S.O. et al. Manual of Propaedeutic Pediatrics. – Ternopil: TSMU,
2005. – P. 6-22.
3. Pediatric Nurse Practitioner Certification Review Guide / editor, Virgina layng
Milloing: contributing authors, Ellen Rudy Clore and all. - 2nd ed. - Health
Leadership Associates,Inc.,1994. - 628 p.
4. Nelson Textbook of Pediatrics / edited by Richard E. Behrman, Robert M.
Kliegman, Ann M. Arvin; senior editor, Waldo E. Nelson - 15th ed. W.B.Saunders Company, 1996. - 2200 p.