* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Learning Objectives Chapter 10
Vectors in gene therapy wikipedia , lookup
Biochemical cascade wikipedia , lookup
Magnesium transporter wikipedia , lookup
Protein–protein interaction wikipedia , lookup
Two-hybrid screening wikipedia , lookup
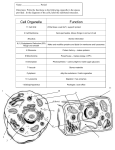
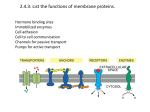
Evolution of metal ions in biological systems wikipedia , lookup
G protein–coupled receptor wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Paracrine signalling wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
SNARE (protein) wikipedia , lookup
Lipid signaling wikipedia , lookup
Proteolysis wikipedia , lookup
Signal transduction wikipedia , lookup
Western blot wikipedia , lookup
Jimmy Kimber LECOM – Seton Hill OMS1 Biochemistry Chapter 10 Learning Objectives 1. What is a source of Vibrio cholera? It grows well under alkaline conditions found in seawater, attaches to chitin in shellfish 2. How does one test uric acid levels? Enzyme uricase converts uric acid to allantoin and hydrogen peroxide. Uric acid has a strong light absorbance at 293 nm, so test a sample before and after treatment with uricase. Alternately, determine the amount of hydrogen peroxide formed during the course of the reaction. 3. What is the difference between gram-negative, gram-positive? Gram-negative: plasma membrane surrounded by a thin cell wall composed of proteinpolysaccharide structure, peptidoglycan Gram-positive: membrane surrounded by a thick peptidoglycan cell wall that retains the gram stain 4. By what mechanism does Clostridium perfringens work? It contains a lipase that hydrolyzes phosphocholine from phosphatidylcholine and from sphingomyelin. The lysis of the cell membrane releases intracellular contents that provide bacteria with nutrients for rapid growth. These bacteria are strict anaerobes. 5. What is the effect of ethanol of membrane fluidity? It increases membrane fluidity caused when ethanol intercalates between membrane lipids. Changes in fluidity affect proteins that span the membrane like ion channels and receptors for neurotransmitters. 6. How does Vibrio Cholera use carbohydrates to bind their target? Glycolipids serve as binding sites for viruses and bacterial toxins (like the A B and O blood group carbohydrates). In this case, cholera AB toxin binds to GM1-gangliosides on the surface of the intestinal epithelial cells. 7. What are the 3 classifications of proteins in the plasma membrane? Integral proteins – channels or transporters for the movement of compounds across membrane, or act as receptors, or structural proteins (Band 3 – binds spectrin) Peripheral membrane proteins – spectrins Lipid-Anchored proteins – use the glycophosphatidylinositolglycan (GPI) anchor: proteins anchored with palmityl, myristyl, fatty acyl groups or with geranylgeranyl or farnesyl isoprenyl groups. Jimmy Kimber LECOM – Seton Hill OMS1 8. What is simple diffusion, Examples? Net movement from a region of high concentration to low concentration. Ex: O2 and CO2 Aquaporins allow water to flow in great quantity. 9. What is facilitative diffusion, examples? Requires a carrier protein in the membrane. The protein undergoes a conformational change that allows molecule to be released on the other side: like enzymes, exhibits saturation kinetics. Example: glucose transporters, which are acted upon by insulin 10. What is a gated channel, examples? Transmembrane proteins form a pore for ions that is either opened or closed in response to a stimulus. Ex: CFTR (cystic fibrosis transmembrane conductance regulator) is a Cl- channel that is a member of the adenine nucleotide-binding cassette (ABC) superfamily. It has two domains that form a closed channel, each connected to ATP. When the domain is phosphorylated, it moves away from the ATP, and it is hydrolyzed to open the channel. Despite the use of ATP, this is still considered diffusion. 11. What is the mutation in cystic fibrosis? How is this related to cholera? Cystic fibrosis mutation is in the gene encoding CFTR, resulting in dried mucus accumulation in the airways and pancreatic ducts. This is similar to cholera toxin, which indirectly activates phosphorylation of the regulatory domain of CFTR by protein kinase A. The channel stays open and Cl- and H2O flow from the cell into the intestinal lumen. 12. Describe why administering Na, K and glucose is an effective treatment for cholera: The goal of treatment is to pull water back into the cell so that it can be reabsorbed. This can be accomplished by using the secondary active transport of glucose by the Na/glucose cotransporter. On the basal side of the epithelium, there is active transport of sodium molecules that creates a gradient, which then allows sodium to be pulled in from the lumen via facilitated diffusion. The carrier molecule is a cotransporter with glucose. So, both Na and glucose are pulled into the cell. Glucose is relatively large, and Na is positively charged. They pull with them a good deal of water. 13. What are means of vesicular transport. Give an example of a molecule transported in vesicles: Exocytosis, Endocytosis (pinocytosis, phagocytosis) Receptor mediated endocytosis (clathrin-coated vesicles) - Ex: cholesterol uptake, as mediated by LDL receptor 14. Give examples of diseases caused by defects in lysosomal enzymes: Tay-Sachs – accumulation of partially digested gangliosides Pompe Disease (accumulation of glycogen particles) Jimmy Kimber LECOM – Seton Hill OMS1 15. Explain why there is extremely painful swelling of acute gouty arthritis: The body reacts to deposition of monosodium urate crystals in the synovial space by phagocytosis with neutrophils. When this happens, the urate crystals cannot be degraded by the lysosomal enzymes. So, the lysosomal acid hydrolases accumulate in attempt to destroy it, and this causes lysis of the lysosomal membrane, followed by cell lysis and release of lysosomal enzymes into the joint space. This recruits other cells to the joint space and amplifies the inflammatory reaction. 16. Explain why peroxisomes are needed, and what ALD and Zellweger are: Peroxisomes are cytoplasmic organelles that do the oxidative reactions using H2O2 to oxidize VLCFA to shorter chain fatty acids, the conversion of cholesterol to bile acids, and the synthesis of ether lipids. Adrenoleukodystrophy (ALD) – mutation decreasing the content of a transporter in the peroxisomal membrane Zellweger – failure to complete the synthesis of peroxisome 17. What happens to the smooth ER with chronic ingestion of ethanol? Increase the content of microsomal ethanol oxidizing system (MEOS), which is a cytochrome P450 enzyme that catalyzes the conversion of EtOH, NADPH, and O2 to acetaldehyde, NADP+ and 2H20. 18. Where is the cis and trans face of the Golgi network? Cis – near the nucleus Trans – near the plasma membrane 19. Describe the function of G-protein Arf in Cholera infection: Arf is a member of the ras superfamily. It is required for transport of V. cholera A toxin. The toxin is endocytosed in caveolae vesicles that merge with lysosomes where the acidic pH activates it. It is transported through golgi and ER and further processed and activated. Arf forms a complex with the toxin that promotes its travel between compartments. The A toxin is an ADP ribosylase, so the protein is called the ADP-riboslyating factor. 20. What are the two motor proteins on microtubules? Toward which end do they travel? Kinesins – plus end Dyneins – minus end 21. How does colchicine relieve the inflammatory response associated with formation of urate crystals? Colchicine binds to dimers of the alpha and beta subunits of tubulin. When the tubulin dimercolchicine complex binds to microtubules, it stops further polymerization of the microtubules, Jimmy Kimber LECOM – Seton Hill OMS1 so they disassemble. The microtubules are necessary for vesicular movement of urate during phagocytosis. So, no phagocytosis, no movement into lysosomes, no inflammation. 22. Why does colchicine have a narrow therapeutic index? Its therapeutic effect depends on inhibiting tubulin synthesis in neutrophils, but it can also prevent synthesis in other cells. Fortunately, neutrophils concentrate colchicine, so that they are affected at lower intakes than other cell types.