* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download McLovin`s Wisdom #1 – The Kidney, Diabetes Type 1 DM Type 2
Basal metabolic rate wikipedia , lookup
Photosynthesis wikipedia , lookup
Photosynthetic reaction centre wikipedia , lookup
Genetic code wikipedia , lookup
Lactate dehydrogenase wikipedia , lookup
Nicotinamide adenine dinucleotide wikipedia , lookup
Butyric acid wikipedia , lookup
Mitochondrion wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Renal function wikipedia , lookup
Light-dependent reactions wikipedia , lookup
Microbial metabolism wikipedia , lookup
Biosynthesis wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Electron transport chain wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
NADH:ubiquinone oxidoreductase (H+-translocating) wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Adenosine triphosphate wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
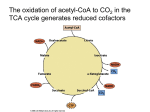
McLovin’s Wisdom #1 – The Kidney, Diabetes Definition Epidemiology (prevalence in Australia) Onset Aetiology Pathology Type 1 DM Insulin deficient <1% in population (10%) Type 2 DM Insulin resistant 8% <40 (Kumar: <20) Takes weeks-months from the initial autoimmune Genetic predisposition Trigger >30 Years (insidious) Destruction of ß-cells (autoimmune destruction) insulin deficiency Symptoms/signs Polyuria, polydipsia, weight loss, wasting, glycosuria, ketoacidosis/coma, fatigue, vomiting (ketones – hangover)… if uncontrolled then get the hyperglycaemic signs Treatment Insulin replacement Lifestyle: Obesity/Lack of exercise Genetic predisposition Age (Mnemonic = LAG) Insulin resistance ß-cell exhaustion Neuropathy tingling, loss of sensation, foot ulcers Macrovascular/microvascular disease (esp. blindness) Diet/exercise (lifestyle), metformin (oral medications), insulin injection (sometimes), bariatric surgery Kidney arterial progression: Renal a. segmental interlobar arcuate interlobular Two kidneys are different heights, s From the front to the back: vein, then ureter, then a. Post = a. Mid = u. Ant = v. The macula densa has its effect on the afferent arteriole. Label: o PCT o Thick dLH o Thin dLH o Thin aLH o Thick aLH o DCT Collecting duct Papilla Urinary pole Vascular pole Afferent a. Efferent a. Bowman’s capsule Parietal layer Visceral layer (podocytes) PCT has brush border, whereas DCT has a clean, large lumen. Collecting duct has more cells (distal collecting duct becomes more columnar ?) Thick tubules are thicker because of their cuboidal histology, versus the squamous histology of thin tubules Podocytes act as a sieve o The glomerular capillaries are fenestrated and covered in a glycocalyx layer o Outside the capillaries are a basement membrane Macula densa detect NaCl changes in the afferent a. o Act on the juxtaglomerular cells, which renin o Renin effects the conversion of angiotensinogen to angiotensin I, which is then converted by ACE to angiotensin o Salt concentration decreases, want to increase the GFR (because if the RPF and hence GFR drop, then the plasma going through the tubule has greater chance to have the salt reabsorbed, so low salt means our GFR is too low). We increase GFR through: Autoregulation (altering vasoconstriction of afferent/efferent a’s) Renin release (note AT2 has several Macula densa releases NO – also contributes to the autoregulation that occurs (e.g. afferent/efferent vasoconstriction control) RPF decreases GFR decreases Functions of different parts: o PCT 2/3 water reabsorbes 2/3 salt reabsorbed (basolaterial Na-K ATPase and an apical Na-amino acid cotransport OR Na-glucose cotransporter OR Na-H+ proton pump). Then Cl- follows due to electrostatic movement. Water follows by osmosis 50% of urea is reabsorbed – increases extracellular osmolality in the medulla 100% of glucose is reabsorbed (via SGLT-2 with GLUT2 then SGLT-1 with GLUT1) o Thin dLH Impermeable to salts, urea 15% water reabsorption o Thin aLH Impermeable to water Passive reabsorption of NaCl o o o o o o o Small amount of urea then goes into the tubule o Thick aLH Impermeable to water Active transport of NaCl Na-2Cl-K symporter o DCT Impermeable to water Active transport of NaCl o Collecting duct ADH AQP2 (changing whether NH3/NH4+ deal (check acid-base lecture) Sodium ion channels (Na-2Cl-K transporters with the Na-KATPase) Still concentrating urine and adjusting water reabsorption Equations lecture Diagram: Substance A, B, C, D Completely secreted, Completely reabsorbed, Partially reabsorbed, Partially secreted No secretion/reabsorption = Inulin or creatinine Completely secreted = PAH – paraaminohippuric acid Completely reabsorbed = glucose in non diabetic/non pregnant Partially reabsorbed = NaCl, vitamin C Partially secreted = urea Clearance = UV/P RPF = Clearance of PAH GFR = volume filtered per minute GFR = Clearance of Inulin Filtered load = GFR*(plasma concentration of substance) C>GFR secretion SNGFR = Kf[(P_GC – P_T)-(π_GC-π_T)] o Π_T~0 GFR = ∑SNGFR McLovin’s Wisdom #2 – Biochemistry Tissue Carbs Ketones Muscle Y Y Liver Y N Neurons Y Y Adipose Y Y RBC Y N Fat Y Y N Y N Lactate Y(cardiac) Y N N N Definitions of anabolism and catabolism, and how ATP stores energy Fats Polysaccharides Break down to fatty acids Break down to glucose and glycerol (lipase and and monosaccharides colipase) Proteins Amino acids All of these are converted to acetyl-CoA via a series of reactions that we’ll look at later. The acetyl-CoA then feeds into the TCA cycle Amino acids are split into their carbon skeletons (TCA cycle) and their ammonium groups, which are fed into the urea cycle Starch amylase etc glucose Mg2+ is always a cofactor for an ATP-consuming reaction. PFK2 – inhibited by glucagon. Stimulated by insulin. PFK2 – stimulates PFK1 and inhibits F-bisphosphatase PFK1 – inhibited by ATP. Stimulated by ADP and AMP. G-6-P is where glycogen metabolism fits in. He put up the stoichiometry of glycolysis Pyruvate can do a few things Acetaldehyde ethanol (yeast) Lactate (people) Fructose (DHAP in liver or F-6-P in fat tissue) and galactose enter the pathway earlier on. Essential fructosuria – benign, don’t get energy from fructose. Hereditary fructose intolerance – occurs in a later step in the pathway (after an irreversible step – the substance trapped has a phosphate attached – build up of F-6-P). Galactosemia – past an irreversible step, you have a buildup of G-1-P (cataracts, splenomegaly, mental retardation). Pyruvate acetyl coa with pyruvate dehydrogenase (one NADH produced) Fatty acid fatty acyl-CoA (cytoplasm) fatty acyl-CoA (mitochondria) [canitine transport system, inhibited by malonyl CoA] fatty acyl-CoA (n-1) + acetyl-CoA [beta oxidation] Glycerol enters the pathway at DHAP (via G-3-P; uses ATP and produces either NADH or FADH2) Proteins in the body are not just “stored” – they are always doing something Transamination Alpha keto acid amino acid Transaminase Important because when we break down amino acids to use the carbon backbone in TCA cycle, we produce an ammonium. The ammonium is transported to the liver in a non-toxic form (glutamate), where the urea cycle is carried out. Urea cycle converts the Ordinarily Careless Crappers Are Also Frivolous About Urination NH3 + CO2 + aspartate + 3 ATP + 2 H2O → urea + fumarate + 2 ADP + 2 Pi + AMP + PPi 2 NH3 + CO2 + 3 ATP + H2O → urea + 2 ADP + 4 Pi + AMP TCA cycle Everything is down to acetyl-CoA now. Point = produce NADH and FADH2 (electron carriers) to Can I Keep Selling Sex For Money Officer Pyruvate, Isocitrate, Alpha-ketoglutarate dehydrogenases (are activated by ADH and inhibited by ATP)… except PDH is also inhibited by citrate. Acetyl-CoA + 3NAD+ + FAD+ + GDP + Pi + 2H2O CoA + 3NADH + 3H+ + FADH2 + GTP + 2CO2 Overall: glucose 10 NADH + 2FADH2 + 4ATP/GTP Some of the NADH were produced in the first part of glycolysis (cytoplasm), so need to be moved to the mitochondria (malate/aspartate and glycerol-3-P shuttles), to feed into the electron transport chain. Malate/aspartate = heart and liver. GAP shuttle 10 H+ inside from NADH and 6+ inside from FADH2. Each ATP needs a total of H+ to be produced. Electron transport chain Complex 1: pumps 4H+ Complex 3: pumps 2H+ Complex 4: pumps 4H+ TLDR: NADH pumps 10; FADH2 pumps 6. NADHNAD+ + H+ at the beginning. FADH2 FAD+ at complex 2 At complex 4, 1/2O2 + 2H+ H2O (the H+s are reacted with oxygen to reduce it to water. Hence oxygen is needed). ATP synthase. 4H+ going through ATP synthase produce 1 ATP (3H+ go through there, and 1H+ used to transport the ATP back out into the intermembrane space – the outer mitochondrial membrane is just permeable to ATP) Hence because one NADH produces 10 ATP, there are 2.5 ATP produced per NADH (similarly, FADH2 produces 1.5 ATP). Chemiosmosis = uncoupled nature of the proton pump to the ATP synthase.