* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Exercise Physiology Study Guide-Test 1 History of Exercise
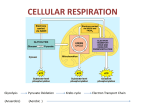
Electron transport chain wikipedia , lookup
Butyric acid wikipedia , lookup
Metalloprotein wikipedia , lookup
Biosynthesis wikipedia , lookup
Light-dependent reactions wikipedia , lookup
Mitochondrion wikipedia , lookup
Phosphorylation wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Microbial metabolism wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Adenosine triphosphate wikipedia , lookup
Biochemistry wikipedia , lookup
Exercise Physiology Study Guide-Test 1 History of Exercise Physiology o First research paper in 1973, Seguin and Lavoisier-oxygen consumption o First textbook, “The Physiology of Bodily Exercise”, Lagrange 1898 o Modern Day Olympics, 1896, Athens, Greece Exercise Physiology Pioneers o AO Atwater-developed first cycle ergometer, 1903 o John Haldane-Haldane apparatus, 1917 o August Krogh-Father of Exercise Physiology, Nobel Prize 1920 (blood flow, O2) o AV Hill-muscle physiologist, Nobel Prize 1922 (heat production in muscle), force-velocity relationship o David Bruce Dill-born in Kansas, 40-40-40 club, Director of Harvard Fatigue Lab, Environmental research, Army American College of Sports Medicine o Founded in 1954 Metabolism o Sum of all chemical reactions in the body that take place in a living organism Catabolism-break down Anabolism-build up Bioenergetics-Chemical conversion of foodstuffs into biological energy Thermodynamics o Energy can be neither created nor destroyed Energy in (food)=energy out (work) + energy out (heat) ± energy stored (fat) o Processes move from a higher to a less order Conversion processes is inefficient; 60-70% of the energy used by the body is released as heat; remaining energy is used for muscle activity and cellular processes ΔEntropy=solid<liquid<gas=↑Entropy Concept of Free Energy (ΔG) o Helps determine if a chemical reaction will occur Energy for Cellular Activity o Carbohydrate (glucose and glycogen) o Fat (triglycerides) o Protein (amino acids) At rest, body uses CHO and fats for energy With mild to severe effort=CHO Protein provides little energy Enzymes provide a catalyst for metabolism Carbohydrate o Readily available and easily metabolized by muscles o o Fat o o o Ingested, converted to glucose, taken up by the liver and muscles, then converted to glycogen Glycogen is stored in the liver and is converted back to glucose as needed Advantages: High energy yield per liter of O2 uptake (5.2kcal/LO2) Metabolized both aerobically and anerobically Rapid activation Glycogen concentration can be greatly increased by training and diet Can be the sole source of energy during heavy exercise Disadvantages: Stored with a lot of water (reduces caloric value of storage form) Small amount of glycogen stored Accumulation of lactate with anaerobic use of glycogen Muscle cells are dependent upon internal glycogen stores Provides substantial energy during prolonged, low intensity activity Larger reserves than carbohydrates Less accessible for metabolism Advantages: Highest energy value of any fuel (9.3kcal/g) Fat can be stored in large amounts Disadvantages Total caloric value of intramuscular fiber lipid is small compared to glycogen Energy release from fat only occurs with O2 uptake Oxidation of fat yields less energy per liter of O2 consumption than CHO Majority of fat is stored outside muscle Fats cannot serve as the sole energy source CHO vs Fat o Each gram of CHO yields 17 KJ (4 kcal) o Each gram of Fat yields 37 KJ (9 kcal) o For every 1 g of glycogen 2.7 g of H2O are stored Protein o Can be used as energy source if converted to glucose via glucogenesis o Can generate FFAs in times of starvation through lipogenesis o Only basic units of protein used for energy (Amino Acids) o Approximately 20% of human body is protein Time to Exhaustion (at 70% VO2max) o CHO:2-2.5 hours o Fat:3-5 days o Protein:2.5 days Basic Energy Systems for APT production o ATP-PCr system-quick explosive energy source o Glycolytic system-short, high intensity energy source Anaerobic breakdown of CHO (glucose/glycogen) o Oxidative System-long term aerobic energy production (CHO and fat metabolism) Glycolysis, Krebs Cycle, ETC, Beta-Oxidation ATP-PCr System o Can prevent energy depletion by forming more ATP Rapid, no O2 required o Occurs in cytosol of the cell o Provides energy (ATP) for only a few seconds (3-15 seconds) during intense muscular effort o 1 mole of ATP is produced per 1 mole of phosphocreatine Immediate Energy Sources o ATP Ca2+ 2+ ATP+Actin+MyosinActomyosin+Pi+ADP+Energy ATPase o ATP+H2OADP + Pi Creatine Phosphate (CP) or Phosphocreatine (PCr) Creatine kinase o PCr+ADPATP+Cr Adenylate kinase/myokinase reaction Adenylate kinase ADP+ADPATP+AMP Glycolysis o Breakdown of glucose, may be anaerobic or aerobic o Requires 12 enzymatic reaction to breakdown glucose and glycogen into ATP o When it occurs in glycolytic system is anaerobic o Glycolysis occurs in the cytosol of the muscle cell o Glycogenesis-process by which glycogen is synthesized from glucose to be stored in the liver o Glycogenolysis-process by which glycogen is broken into glucose-1-phosphate o Glucose is broken down into two 3 carbon structures called pyruvic acid Crossroad for aerobic metabolism (with O2) or lactic acid (without O2) o Pyruvic acid is then converted to lactic acid o Breakdown of glucose yields 2 ATP, 3 ATP if glycogen Lactic Acid Formation o Pyruvic AcidLactic AcidLactate ↘H+ LDH Oxidative System o o o o Relies on O2 to breakdown fuels for energy Produces ATP in mitochondria of cells Can yield much more energy (ATP) than anaerobic systems Primary method of energy production during endurance events Oxidation of Carbohydrate Glycolysis, Kreb’s cycle, ETC Oxidation of Fat Beta Oxidation, Kreb’s cycle, ETC Glycolysis-Kreb’s Cycle Link o Glycolysis occurs in the cytosol of the cell o Kreb’s cycle occurs in the mitochondria of the cell o With O2 pyruvic acid is converted to acetyl coenzyme A (Acetyl CoA) o Acetyl CoA enters Kreb’s cycle Krebs Cycle Energy Production o For each molecule of glucose: 2 ATP 6 NADHETC 1 NADH=3 ATP 2 FADHETC 1 FADH=2 ATP Electron Transport Chain o ETC is coupled to the Krebs cycle o Hydrogen ions produced from glycolysis and krebs cycle combine with NAD and FAD and form NADH and FADH2 Accomplishes: Prevention of H+ ions Carries H+ ions to ETC H+ combines with O2 to form water End products of oxidative carbohydrate metabolism are carbon dioxide and water Glycolysis 2 ATP 2 ATP 2 NADH 6 ATP Acetyl CoA 2 NADH 6 ATP Krebs Cycle 2 ATP 2 ATP 6 NADH 18 ATP 2 FADH 4 ATP 2 Total 38 ATP (glucose) 39 ATP (glycogen) Oxidation of Fat (Beta-Oxidation) o Lypolysis-breakdown of triglyericde into glycerol and free fatty acids (FFA’s) o Acetyle CoA enters Krebs cycle and ETC o Fat oxidation requires more oxygen and generates more energy than CHO oxidation o Once acetyl CoA enters Krebs cycle, it follows the same fate as CHO 2-carbon compounds o FFA’s can produce more ATP than CHO o Example: Pamatate is a 16 carbon compound 8 Acetyl CoA molecules 96 ATP 7 NADH 21 ATP 7 FADH 14 ATP 2 Subtotal 131 ATP - 2 for activation TOTAL 129 ATP 3 FFA per triglyceride, therefore total ATP produced is 387 ATP Lipids o Predominate fuel for heart and muscle at rest. o Storage form of fat: triglycerides, diglycerides, monoglycerides o Primary storage: adipose tissue o “trans fats”: make liquid fats solid, increase LDL, decrease HDL o Esterification: formations of triglycerides from fatty acids; uses O2 o Hydrolysis: breakdown of fatty acids from triglycerides Mobilization o Lipolysis-breakdown of triglycerides to fatty acids Important enzymes in adipose tissue o ATGL-adipose tissue lipase o HSL-hormone sensitive lipase Stimulated by o Fast-catecholamines o Slow-growth hormone Epinephrine, SNS (norepinephrine), hGH, cortisol increases Insulin, ketones, lactate decreases Circulation o Fatty acids exit adipocytes o Fatty acids circulate bound to albumin o Must increase blood flow through tissue Uptake o FFA released from albumin and binds to fatty acid binding protein o Lipoprotein lipase (LPL) o Increased by endurance training Activation o Occurs in cytosol o Fatty acid is attached to coenzyme A (CoA) o Requires ATP Translocation o Outer mitochondrial membrane – carnitine replaces CoA o Inner membrane – CoA replaces carnitine o Carnitine acyl transferase I Inhibited by malonyl CoA an intermediate of fatty acid synthesis o Carnitine acyl transferase II o Enzyme content increases with training due to increased mitochondrial density Beta oxidation o Cleaves 2 carbons at a time from fatty acyl CoA o Rate limiting enzyme is B-ketoacyl-CoA thiolae o Results in acetyl CoA and NADH and FADH2 Lipid Oxidation o Activation costs 2 ATP o 1 FADH2 x 2 ATP o 1 NADH x 3 ATP o N represents the # of carbons in a fatty acid chain ((n/2) - 1) FADH2 x 2 ATP ((n/2) - 1) NADH x 3 ATP (n/2) acetyl CoA x 12 ATP Activation = - 2 ATP 129 net ATP Intramuscular Fat o Lipoprotein lipase (LPL) Hydrolyzes intramuscular triglycerides for β oxidation Endurance training increases LPL activity Regulated by: o Glucagon (+) o Growth hormone (+) o Insulin (-) o Uptake of FAs during exercise is low, but training increases FA uptake and oxidation – glycogen sparing o o o o o IMTG likely recruited following glycogen depletion IMTG mobilized during recovery from prolonged exercise – leads to glycogen depletion Primarily occurs in the heart and liver Brain/red blood cells rely mostly on glycolysis Skeletal muscle cells White fibers (Type IIb; “Fast glycolytic”) also rely on glycolysis o Low blood supply o Low mitochondrial density o Low [FABPs] Red skeletal muscle (Type I) better equipped to use fat as fuel o High blood supply o Innervated with high number of capillaries o High myoglobin/mitochondrial content o Endurance training ↑ mitochondrial capacity to use fat o Fuel Selection Exercise onset – increased uptake/oxidation LCFA Low intensity exercise – enhanced lipid utilization at expense of CHO as energy fuel Increased intensity – increased CHO/decreased fat utilization Endurance training – shifts towards lipid utilization o Crossover concept Rest – lipid oxidation dominates As exercise starts and intensity increases – crossover from lipid to CHO utilization Endurance training=higher cross over o Increases lactate clearance capability o Reduced epinephrine secretion o Increased mitochondrial mass Glycogen sparing-reduced glycogenolysis Keotacidosis o Ketogenolysis – usage of ketone bodies for energy o Ketogenesis – creating of ketone bodies o Occurs mostly in the liver o Utilized by kidney, brain, and muscle o Ketone Bodies: Acetone Acetoacetic acid 3-hydroxybutyrate o Generated during fasting, starvation, diabetes, endurance exercise or low carbohydrate intake o Acidic-decreases blood pH o Made in liver o Ketoacidosis: Fruity breath Acetone excreted in urine Lipid oxidation summary o Lipid oxidation predominates at rest and decreases with exercise o Beta oxidation breaks down fatty acids 2 carbons at time o Intramuscular fat used during exercise o Ketone bodies-alternative fuel source o Mitochondrial adaptations occur with endurance training Protein metabolism o Skeletal muscle proteins Major storehouse for AA’s Liver, intestinal wall, blood o Skeletal muscle can catabolize its own protein content into AAs Transaminase enzymes o Exchange amine groups to amino and keto acids Net degradation of AAs limited in skeletal muscle Liver major site for AA degradation o Carbon skeletons of AAs are degraded: Converting the carbon atoms to glucose o Glucogenic Converting the carbon to the ketone acetoacetate or acetyl-CoA o Ketogenic After removal of N+ groups, most AA residues appear as: o Pyruvate o Krebs cycle intermediates o Nitrogen Removal Cleave nitrogen from protein Nitrogen removal has 2 major mechanisms o Oxidative deamination Occurs in mitochondrial matrix of liver o Involves NAD+ (oxidizing agent) o Glutamate dehydrogenase o Sufficient substrates: NAD+ NADH = glutamate o Insufficient substrates: Glutamate -ketoglutarate and NADH NADH yields several ATP o Transamination Most common route for exchange of AA’s Transfer amine group o Key transaminases o Glutamate-pyruvate transaminase (GPT) (uses alanine) or alanine aminotransferase Pyruvate + glutamate alanine + Ketoglutarate o Glutamate-oxaloacetate transaminase (GOT) (or aspartate aminotransferase OAA + glutamate aspartate + Ketoglutarate Gluconeogenic AAs AAs can supply carbon for gluconeogenesis o Catabolized AAs from proteins are important Glucose levels (kidney and brain) o Starving o Fasting o Prolonged exercise can simulate fasting o Caloric demands in excess of supply (glucose) Body must find ways to make glucose in these situations o Phosphoenolpyruvate (PEP) o PEP (phosphoenolpyruvate) AAs can supply carbon for gluconeogenesis o AAs that give rise to: Pyruvate Oxaloacetate Malate o Can become precursors for PEP o PEP Glucose Expensive (significant energy input) o PEP Pathways Mitochondria in liver and kidneys Mitochondrial and cytoplasmic processes Pyruvate Oxaloacetate PEP Malate PEP o Glucose-Alanine Cycle Can provide 130g of glucose per day during fasting or starvation o Review of Protein metabolism Protein contributes very little as source of fuel Except for BCAAs, skeletal muscle is NOT a site for degradation Can be site of transaminase reactions only – not net change in concentrations Oxidative deamination occurs in the liver Risk Stratification for exercise testing o o o o High risk: known cardiovascular, pulmonary, or metabolic disease or symptoms—need physician present to supervise sub or max testing cardiovascular- cardiac, peripheral vascular (DVT or claudication), cerebrovascular (stroke) pulmonary- COPD, asthma, lung disease, cystic fibrosis metabolic- diabetes (type 1 or 2), thyroid, renal or liver disease symptoms: o Pain or discomfort in chest, neck, jaw, arms from ischemia o Shortness of breath at rest or mild activity, fatigue o Dizziness or syncope o Ankle edema o Palpitation or tachycardia o Intermittent claudication o Heart murmur Moderate risk: Asymptomatic with 2 or more risk factors- Physician recommended for max testing, recommend to see physician before vigorous training Low risk: Asymptomatic with 1 or less risk factors Risk Factors Age o men 45 and older, women 55 and older Family History o first degree relative (immediate family or grandparents) with MI, coronary revascularization, or sudden death before the age of 55 for men or 65 for women Smoking o Current smoker or stopped within 6 months Sedentary lifestyle o Less than 30 minutes of moderate intensity activity, 3 days a week for 3 months Obesity o BMI over 30 o Waist girth >102 cm (40 inches) for men, >88 cm (35 inches) for women Hypertension o > or= to 140/90 on a least 2 separate occasions o On hypertensive medicine Dyslipedimia o > or= to 130 LDL o <40 HDL, *if > or = 60, then Negative risk factor* o >or= to 200 total CHO o On lipid-lowering medication Prediabetes o Fasting glucose >or = to 100 but less than 126 o Oral glucose tolerance test > or= to 140 but less than 200 on two separate occasions