* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download review neurochemical markers of alcoholism vulnerability in humans
Behavioral epigenetics wikipedia , lookup
Heritability of IQ wikipedia , lookup
Signal transduction wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
State-dependent memory wikipedia , lookup
Aging brain wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Effects of alcohol on memory wikipedia , lookup
Neurotransmitter wikipedia , lookup
Impact of health on intelligence wikipedia , lookup
Neuroeconomics wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Biology of depression wikipedia , lookup
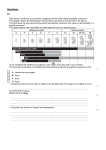
Alcohol & Alcoholism Vol. 37, No. 6, pp. 522–533, 2002 REVIEW NEUROCHEMICAL MARKERS OF ALCOHOLISM VULNERABILITY IN HUMANS JOELLE E. RATSMA*, ODIN VAN DER STELT1 and W. BOUDEWIJN GUNNING Academic Center for Child and Adolescent Psychiatry, University of Amsterdam, P. O. Box 12474, 1100 AL Amsterdam, The Netherlands and 1 Department of Psychiatry, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina, USA (Received 22 March 2002; accepted 10 May 2002) Abstract — This review considers several neurochemical characteristics or trait markers that may be related to a genetic vulnerability to alcoholism. These potential neurochemical markers of alcoholism vulnerability include indices of activity of five neurotransmitter systems, namely γ-aminobutyric acid, serotonin, dopamine, noradrenaline and β-endorphin. This review evaluates whether potential abnormalities in these neurochemical indices, as assessed in alcoholics and in the children of alcoholics, meet three criteria for the identification of a vulnerability marker of alcoholism: (1) heritable; (2) associated with alcoholism in the general population; (3) state independent. It is concluded that, at present, indices of increased baseline activity of the serotonin transporter in platelets and of increased responsiveness of the pituitary β-endorphin system may fulfil each of these three criteria. Additional research efforts should be devoted to the evaluation of trait marker properties of neurochemical indices in individuals at high risk for alcoholism. INTRODUCTION obscure the relation between a marker and a clinical syndrome. Family studies are required to determine whether the trait marker co-segregates with alcoholism within families, since all members of a family are part of the same population. However, there is as yet little information on the cosegregation of neurochemical markers with alcoholism in affected families. This review evaluates whether abnormalities in certain neurochemical indices, as assessed in alcoholics and in COA, meet the three above-mentioned criteria for the identification of a trait marker of alcoholism. Thus, the issue is addressed whether a certain neurochemical abnormality is associated with alcoholism, or with a given subtype of alcoholism, in the general population. To clarify this issue, studies are reviewed in which measures of neurochemical activity are compared between alcoholics and unrelated non-alcoholic controls. In addition, to evaluate whether a certain neurochemical abnormality is heritable, this review focuses on twin and adoption studies to find out whether the abnormality is mediated largely by genetic, as opposed to environmental, factors. Finally, to evaluate whether the neurochemical abnormality is state independent, that is, not reflecting the current state of alcoholism but present throughout an individual’s lifetime, studies are reviewed in which the neurochemical measure of interest is compared between individuals at high risk for alcoholism and low-risk controls. As opposed to this high-risk research, studies of (abstinent) alcoholics cannot distinguish between state and trait markers of alcoholism. Even after many years of abstinence from alcohol, the prolonged abuse of alcohol may have had long-term neurotoxic effects, potentially affecting neurochemical trait markers in abstinent alcoholics. This review will focus on indices of neurochemical markers. These are indices of changes in neurotransmitter systems that are studied as trait markers in alcoholism, in accordance with the three above-mentioned criteria. The state effect of alcohol on changes in neurotransmission has been widely studied within neurotransmitter systems. It has, for example, been the main approach adopted in studies of the N-methyl-D-aspartate receptor of the glutamatergic system. Alcoholism is generally assumed to be a multifactorial disease, in which polygenic influences and environmental influences interact (Goldman, 1995). This conceptualization of alcoholism has been inferred from adoption studies (Goodwin et al., 1973; Bohman et al., 1981; Cadoret et al., 1985; Cloninger et al., 1985) and twin studies (Romanov et al., 1991; Kendler et al., 1994, 1997; Reed et al., 1996; Treu et al., 1996; Heath et al., 1997). The question arises as to what is inherited in alcoholism? Over the past two decades, research on so-called phenotypic trait or vulnerability markers of alcoholism has attempted to shed light on this basic issue. This research has focused on various behavioural, electrophysiological, and neurochemical characteristics that may be related to alcoholism vulnerability (Begleiter and Porjesz, 1988; Farren and Tipton, 1999; Schuckit, 1999; Van der Stelt, 1999). This review evaluates whether abnormalities in certain neurochemical indices, as assessed in alcoholics and in the children of alcoholics (COA), may serve as neurochemical markers of alcoholism vulnerability. A trait or vulnerability marker may be defined as a ‘heritable trait, associated with a causative pathophysiological factor in an inherited disease’ (Gershon and Goldin, 1986). As opposed to a diagnostic marker, a vulnerability or pathophysiological marker is not required to have high sensitivity or high specificity to a certain clinical disorder (Nurnberger, 1992). While sensitivity and specificity are not critical criteria, it has been proposed that a certain behavioural or biological trait should meet at least three basic criteria in order to be considered as a trait marker (Goldin et al., 1986): (1) heritable; (2) associated with the disease in the general population; (3) state independent. The reason for these requirements is to prevent false-positive or false-negative conclusions about the validity of a certain characteristic as a trait marker due to certain conditions, particularly population stratification, which may *Author to whom correspondence should be addressed. 522 © 2002 Medical Council on Alcohol NEUROCHEMICAL MARKERS OF ALCOHOLISM VULNERABILITY However, this review focuses on indices of changes within five neurotransmitter systems that may have a trait effect on alcoholism. This includes the following neurotransmitters: (1) γ-aminobutyric acid (GABA) (Frye and Breese, 1982; Koob et al., 1986); (2) 5-hydroxytryptamine (serotonin; importantly, the impaired functioning of CNS serotonin may result in diminished impulse control, a neurobiological feature of type II alcoholism) (Linnoila et al., 1983; Cloninger, 1987); (3) dopamine (Gessa et al., 1985; Imperato and Di Chiara, 1986; Wise and Bozarth, 1987); (4) noradrenaline (Cloninger, 1994); (5) β-endorphin. This last topic is the subject of two contradictory hypotheses. The endorphin compensation or deficiency hypothesis states that alcohol use compensates for a predisposed or acquired deficiency of endorphinergic receptor activity (Blum, 1983; Volpicelli et al., 1985; Erickson, 1990), whereas the opioid surfeit hypothesis states that alcohol use is increased by a surfeit of opioidergic receptor activity, rather than a deficit (Reid and Hunter, 1984; Hubbell et al., 1986; Reid et al., 1991). Both hypotheses are equally applicable to other neurotransmitter systems. G-proteins and adenylyl cyclase (or any other secondary messenger systems) have not been included in this review as they are not neurotransmitters. GENERAL PRINCIPLES AND OBSERVATIONS FROM ANIMAL STUDIES This review focuses on central and peripheral indices of activity of the five neurotransmitter systems, GABA, serotonin, dopamine, noradrenaline and β-endorphin. On the basis of findings mainly from animal research, each of these neurotransmitter systems has been implicated in the aetiology and pathophysiology of alcoholism. The requisite theoretical background was provided by animal studies carried out in the 1950s, which reported that changes in neurotransmission in rat brains led to addiction-related behaviour. Olds and Milner (1954) found that intracranial stimulation of the hypothalamus and associated structures can act to reinforce operant conditioning. Brain stimulation itself activated systems that were normally activated by a reinforcing stimulus, such as feeding or drinking (Deutsch and Howarth, 1963). Brain selfstimulation (using electrodes placed in the vicinity of dopaminergic neurons) was accompanied by locomotor activation and positive reinforcement (Routtenberg, 1978). Similarly, it has been hypothesized that euphoria and drugseeking behaviour (whether induced by alcohol or other commonly abused substances) arise from activation of the mesolimbic dopaminergic reward pathways of the brain (Gessa et al., 1985; Imperato and Di Chiara, 1986; Wise and Rompre, 1989). Endogenous opioids were also reported to be involved in reward processes during brain self-stimulation (Schaefer, 1988). The intracerebroventricular self-administration of β-endorphin in rats has demonstrated that this substance acts as an endogenous positive reinforcer of behaviour. Thus, it might intrinsically control behaviour such as the selfadministration of addictive drugs (Van Ree et al., 1979). In addition, the opioid antagonist naltrexone blocks the release of dopamine at the level of the nucleus accumbens, which follows alcohol administration (Benjamin et al., 1993). However, the results of animal and human studies suggest that the effects of alcohol consumption are not restricted to 523 dopamine and endogenous opioids. Alcohol consumption may also affect several other brain neurotransmitters, including noradrenaline (Ahlenius et al., 1973; Brown and Amit, 1982), serotonin (McBride et al., 1988; Murphy et al., 1988) and GABA (Hwang et al., 1990; McBride et al., 1990). As alcohol seems to activate most neurotransmitter pathways, the question arises whether vulnerability to alcoholism is associated with a pre-existing deficit within neurotransmitter pathways. TYPES OF HUMAN STUDIES Human research on neurochemical vulnerability markers of alcoholism mainly consists of those at baseline, studies assessing neurochemical indices following a pharmacological challenge, and post-mortem studies. Baseline studies attempt to identify individual variations in the trait marker, in the absence of any interference from alcohol. Challenge studies often attempt to identify individual variations of the trait marker after alcohol intake, while some studies use challenge drugs other than alcohol (acting on one or more of the five neurotransmitter systems under review). This is because any individual variation in sensitivity to the effects of alcohol (or other challenge drugs) might be associated with a variation in the risk of alcoholism (Schuckit et al., 1983; Schuckit and Smith, 1996). Generally, post-mortem studies simply reveal that alcohol has a toxic effect on neurotransmitter systems. The reported results do not usually draw a distinction between the trait and the state effects of alcohol. Baseline and challenge studies are not only performed in alcoholics, but also in high-risk individuals, such as COA. COA represent a unique, high-risk group in studies of the state independence of the trait marker. This is because they have a heightened risk of alcoholism, and because the youngest groups do not generally consume alcohol on a regular basis (Eskay and Linnoila, 1991; Hill et al., 1991; Sher et al., 1991). This review includes neurochemical-trait-marker studies that investigated changes in the levels of neurotransmitters (or their metabolites) in cerebrospinal fluid (CSF) or plasma, and changes in the number, activity and affinity of receptors in the brain. Also included in this review are studies performed on the brain either directly or indirectly (by means of peripheral assessments). There is still some doubt concerning the degree of correspondence between the latter measurements and neurotransmitter activity in the central regions. However, there are problems associated with making some of the abovementioned measurements in neurobiological studies on humans. For example, it may be ethically problematic to subject one particular group of high-risk individuals — the young COA — to invasive or extensive examinations. This is because such examinations include investigations of the CSF, alcohol challenge tests, and various brain-imaging techniques that use radioactive substances. Neurobiological research in high-risk groups, on the other hand, can be carried out with the aid of peripheral blood samples, using platelets for example (Ratsma et al., 1999). In this review, results from challenge studies, baseline studies, and post-mortem studies of alcoholics and their children are evaluated to determine whether certain neurochemical abnormalities meet the three criteria outlined above for the identification of a vulnerability marker of alcoholism. J. E. RATSMA et al. 524 γ-AMINOBUTYRIC ACID Pharmacological properties GABA acts on the GABAA receptor, which is a transmittergated chloride channel. GABAA receptors are composed of three subunits: α, β, and γ. Fourteen variants have been identified to date, six α variants, three β variants, three γ variants and two δ variants. Alcohol and benzodiazepines act on the γ subunit of the GABAA receptor (Suzdak et al., 1986), whereas GABA acts on the α subunit. Changes in the subunit expression of GABAA receptors are reflected in the pharmacological properties of the receptors (Levitan et al., 1988). By contrast, GABAB receptor is a G-protein-coupled receptor without a benzodiazepine binding site. Research findings In the post-mortem frontal cortex, expression of mRNA for the GABAA receptor’s α1 and β3 subunits is higher in alcoholics than in controls (Lewohl et al., 1997; Mitsuyama et al., 1998). These findings are consistent with the results of two post-mortem studies, in which non-cirrhotic alcoholics were found to have more GABA receptors in their cerebral cortex and superior frontal gyrus than the control subjects (Tran et al., 1981; Dodd et al., 1992). Brain imaging studies using single-photon emission computed tomography (SPECT) (Abi-Dargham et al., 1998; Lingford-Hughes et al., 1998) have found that, in alcoholics and type II alcoholics, the benzodiazepine receptor distribution volume in the anterior cingulate, the prefrontal, frontal, parietal and temporal cortices and in the cerebellum was reduced, relative to controls. Similarly, challenge studies using positron emission tomography (PET) revealed the existence of a blunted glucose utilization response to lorazepam in alcoholics (in the basal ganglia and thalamus) and in COA (in the cerebellum), relative to controls (Volkow et al., 1993, 1995). These SPECT and PET findings indicate abnormalities in brain GABA– benzodiazepine receptor reactivity in alcoholics and individuals at high risk for alcoholism. Finally, in alcoholics in the early phase of abstinence and those who had been abstinent for 1–2 years, a challenge with γ-hydroxybutyric acid (a GABA agonist) showed a blunted growth-hormone (GH) response, relative to controls (Vescovi and Coiro, 1995, 1997). This also may represent reduced GABA neurotransmitter reactivity. In apparent contrast to these findings of blunted, postchallenge GABA responses in alcoholics and COA, one study has reported that GABA plasma levels of COA increased much more in response to alcohol than was the case in controls (Moss et al., 1990). Another study, however, found no significant difference in the GABA plasma levels between COA and controls following a diazepam challenge (Cowley et al., 1996). A twin study (Berrettini et al., 1982) showed that the interindividual differences in baseline plasma level of GABA are heritable. Abstinent adult male alcoholics were found to have a lower baseline plasma GABA level than non-alcoholics (Coffman and Petty, 1985; Petty et al., 1993). In COA, one study showed similarly that COA had lower baseline plasma levels of GABA than controls (Moss et al., 1990), but another study found no significant group difference (Cowley et al., 1996). The young adult COA in the latter study were selected for having no history of alcohol or drug abuse at ages 18–25 years. This may mean that they were at reduced risk of an early onset of alcoholism, which, in turn, may have biased the sample. In conclusion, a lower baseline plasma level of GABA seems to fulfil two criteria for the identification of a vulnerability marker of alcoholism. Inter-individual differences in measures of baseline plasma level of GABA appear to be heritable and alcoholics show reduced levels of GABA in their plasma (see Tables 1 and 2). It remains to be determined, however, whether a lower baseline plasma level of GABA in alcoholics represents a state marker or a trait marker that can also be detected in individuals at high risk for alcoholism. Similarly, measures of decreased GABA receptor responsiveness appear to fulfil two trait marker criteria. Decreased GABA receptor responsiveness seems to characterize both alcoholics and their children. It remains to be clarified whether this characteristic is genetically mediated, though. 5-HYDROXYTRYPTAMINE Pharmacological properties 5-Hydroxytryptamine (5-HT, serotonin) acts on 15 known subtypes of 5-HT receptors, which fall into four structural and functional ‘families’ of receptors. Three types (5-HT1, 5-HT2 and 5-HT4) are coupled to G-proteins, whereas the 5-HT3 receptor acts as a 5-HT-gated ion channel. Although the genes of three other types (5-HT5, 5-HT6 and 5-HT7) have been cloned, their physiological functions are as yet unknown. The 5-HT transporter is located in the serotonergic axon terminals, where it terminates 5-HT action in the synapse, and in platelet membranes, where it takes up 5-HT from the blood (Blakely et al., 1991). The synthesis of serotonin is influenced by the amount of the precursor tryptophan in the brain. In order to gain entry to the brain, tryptophan has to compete with other amino acids. The extent to which tryptophan in the blood circulation is available to the brain may be decreased in alcoholics with a positive family history (see review by Badawy, 1999). The concentration of 5-hydroxyindol-3-yl-acetic acid (5-HIAA; the major metabolite of serotonin) in CSF seems to reflect central serotonergic activity (Banki and Molnar, 1981). Research findings Post-mortem studies of brain tissue from alcoholics have revealed reduced 5-HT transporter binding in the hippocampus (Gross-Isseroff and Biegon, 1988; Chen et al., 1991). Similarly, binding was found to be reduced in the 5-HT1A receptors of alcohol consumers relative to those of subjects who did not (Dillon et al., 1991). Following a challenge with a mixed serotonin partial agonist, m-chlorophenylpiperazine (mCPP), the adrenocorticotropic hormone response and the serotonergic activation in the basal ganglia circuits (involving orbital and prefrontal cortices) were found to be lower in alcoholics, than in nonalcoholics (Krystal et al., 1994; George et al., 1997; Hommer et al., 1997). These findings were reflected by a decrease in the brain’s utilization of glucose, as shown by PET. This suggests that 5-HT2C receptors in alcoholics exhibit reduced sensitivity. Other studies reported challenges in which GH, prolactin and cortisol exhibited blunted responses to fenfluramine (releasing serotonin as an indirect agonist), NEUROCHEMICAL MARKERS OF ALCOHOLISM VULNERABILITY 525 Table 1. Trait marker criteria for neurochemical baseline activities and responses to challenges Neurochemical markers GABA-ergic activity Baseline (plasma GABA) Challenge (receptor reactivity) Serotonergic activity Baseline (5-HT transporter activity) Challenge (receptor reactivity) Dopaminergic activity Baseline (plasma or CSF HVA) Challenge (receptor activity) Noradrenergic activity Baseline (CSF noradrenaline) Challenge (receptor reactivity) β-Endorphinergic activity Baseline (plasma or CSF β-endorphin) Challenge (pituitary reactivity) Presence in alcoholics (compared with controls) Heritable State independent (presence in high-risk groups, compared with controls) Yes — Decreased Decreased Inconsistent Decreased Yes Increased — Increased (long abstinence) Decreased — Inconsistent Inconsistent — Decreased (long abstinence) — — Decreased — — Decreased — — Decreased Yes Increased Decreased (receptor density) Increased Increased (one study) GABA, γ-aminobutyric acid; 5-HT, serotonin or 5-hydroxytryptamine; CSF, cerebrospinal fluid; HVA, homovanillic acid. Table 2. γ-Aminobutyric acid (GABA) studies GABA post-mortem studies Alcoholics vs controls: Increased expression of GABAA receptors in frontal cortex (Lewohl et al., 1997; Mitsuyama et al., 1998) Alcoholics vs controls: Increased number of GABA receptors; frontal and cerebral cortex studies (Tran et al., 1981; Dodd et al., 1992) GABA challenge studies Alcoholics vs controls: Decreased glucose utilization response to agonist lorazepam in basal ganglia, thalamus (Volkow et al., 1993) Alcoholics vs controls: Decreased growth hormone response to agonist GHB (Vescovi and Coiro, 1995, 1997) COA vs controls: Decreased glucose utilization response to agonist lorazepam in cerebellum (Volkow et al., 1995) COA vs controls: Increased plasma GABA levels after alcohol (Moss et al., 1990) COA vs controls: Indifferent plasma GABA levels after agonist diazepam (Cowley et al., 1996) GABA baseline studies Alcoholics vs controls: Decreased benzodiazepine receptor density in the cortex (Lingford-Hughes et al., 1998) Alcoholics type II vs controls: Decreased benzodiazepine receptor density in the cortex and cerebellum (Abi-Dargham et al., 1998) Alcoholics vs controls: Decreased GABA plasma levels (Coffman and Petty, 1985; Petty et al., 1993) COA vs controls: Decreased plasma GABA levels (Moss et al., 1990) COA vs controls: Indifferent plasma GABA levels (Cowley et al., 1996) GHB, γ-hydroxybutyric acid; COA, children of alcoholics. mCPP and sumatriptan (a 5-HT1D receptor agonist). The subjects in question were active alcoholics and abstaining alcoholics who had not used alcohol for 1–2 years (Balldin et al., 1994; Krystal et al., 1996; Vescovi and Coiro, 1997). Conversely, an elevated cortisol response was reported after a challenge with fenfluramine in a high-risk group of attentiondeficit hyperactivity disorder (ADHD) boys, versus ADHD boys with a low risk of alcoholism; the assessed degree of risk was based on the presence or absence of parental alcoholism (Schulz et al., 1998). The results of a study using SPECT showed a reduction in brain-stem serotonin transporters in alcoholics (after 3–5 weeks of abstinence) relative to controls (Heinz et al., 1998). A decrease in alcoholism-related serotonin transport was associated with a decrease in the 5-HT content of platelets in alcoholics (Banki, 1978). It also corresponded to a decrease 526 J. E. RATSMA et al. (relative to controls) in the uptake of [3H]5-HT by platelets in alcoholics undergoing a 2-week period of detoxification (Kent et al., 1985). A twin study found that 5-HT uptake in blood platelets is moderated by genetic factors (Meltzer and Arora, 1988). Alcoholics who had abstained from alcohol for periods of 1 month to 22 years (and their children) were found to have a higher [3H]5-HT platelet uptake than controls (Ernouf et al., 1993). This is contrary to the findings in active alcoholics and in those who had only recently started practising abstinence. In addition, male COA were found to have a higher Vmax (capacity) of platelet serotonin uptake than controls (Rausch et al., 1991). As a result, it was suggested that an increase (rather than a decrease) in platelet serotonin transport was a trait marker for alcoholism (Ernouf et al., 1993). It is important to note that earlyonset alcoholics exhibit higher platelet-serotonin-transporter activity than late-onset alcoholics (Javors et al., 2000). With regard to 5-HIAA, the levels of this metabolite in CSF taken from abstinent alcoholics of both sexes were shown to be lower than in controls (Ballenger et al., 1979; Banki, 1981; Borg et al., 1985). Alcoholic impulsive offenders had lower CSF 5-HIAA levels than alcoholic non-impulsive offenders, whereas the controls had intermediate levels (Virkkunen et al., 1994). Early-onset alcoholics had lower 5-HIAA levels than late-onset alcoholics (Fils-Aime et al., 1996). This was consistent with studies demonstrating low precursor serotonin availability in early-onset alcoholism (Buydens-Branchey et al., 1989). CSF 5-HIAA concentrations might be a staterelated phenomenon, since essential dietary fatty acids could cause changes in CSF 5-HIAA concentrations (Hibbeln et al., 1998). However, an animal study of CSF 5-HIAA levels in monkeys revealed a high degree of intra-individual stability (Raleigh et al., 1992). The above-mentioned CSF 5-HIAA studies, which were only performed in alcoholics, were consistent with the hypothesis that decreased CSF 5-HIAA levels represent a central serotonergic deficit in a subgroup of earlyonset male alcoholics (Linnoila et al., 1983). In conclusion, the inter-individual differences in baseline serotonin transporter activity in platelets seem to be heritable. There are also indications that baseline serotonin transporter activity is elevated in COA and in alcoholics who have been abstinent for a protracted period of time. The measurement of increased baseline serotonin transporter activity in platelets would therefore appear to fulfil three of the criteria for trait markers for alcoholism. Challenge studies of serotonin receptor responsiveness have shown (albeit inconsistently) a decreased 5-HT response in alcoholics. There is also one report of an elevated response in COA, thus one criterion may have been met (Tables 1 and 3). Table 3. Serotonin studies Serotonin post-mortem studies Alcoholics vs controls: Decreased binding 5-HT transporter (Gross-Isseroff and Biegon, 1988; Chen et al., 1991) Alcohol consumers vs controls: Decreased binding 5-HT1A receptor (Dillon et al., 1991) Serotonin challenge studies Alcoholics vs controls: Decreased glucose utilization in basal ganglia circuits and ACTH response to partial 5-HT agonist mCPP (Hommer et al., 1997) Alcoholics vs controls: Decreased ACTH response to mCPP (Krystal et al., 1994; George et al., 1997) Alcoholics vs controls: Decreased prolactin and cortisol response to serotonin (Balldin et al., 1994; Krystal et al., 1996), Alcoholics vs controls: Decreased growth hormone response to 5-HT1D receptor agonist sumatriptan (Vescovi and Coiro, 1997) COA with ADHD vs controls with ADHD: Increased cortisol response to 5-HT agonist fenfluramine (Schultz et al., 1998) Serotonin baseline studies Alcoholics vs controls: Decreased brainstem serotonin transporters (SPECT) (Heinz et al., 1998) Alcoholics vs controls: Decreased platelet serotonin uptake and content (Banki, 1978; Kent et al., 1985) Alcoholics vs controls: Increased platelet serotonin uptake (Ernouf et al., 1993) (long-term abstinence) COA vs controls: Increased platelet serotonin uptake (Rausch et al., 1991; Ernouf et al., 1993) Early-onset vs Late-onset alcoholics: Increased platelet serotonin uptake (Javors et al., 2000) Alcoholics vs controls: Decreased CSF 5-HIAA level (Ballenger et al., 1979; Banki, 1981; Borg et al., 1985) Early-onset vs late-onset alcoholics: Decreased CSF 5-HIAA level (Fils-Aime et al., 1996) Impulsive vs non-impulsive alcoholics: Decreased CSF 5-HIAA levels (Virkkunen et al., 1994) 5-HT, serotonin or 5-hydroxytryptamine; ACTH, adrenocorticotropic hormone; mCPP, m-chlorophenylpiperazine; SPECT, single-photon emission computed tomography; COA, children of alcoholics; ADHD, attention-deficit hyperactivity disorder; CSF, cerebrospinal fluid; 5-HIAA, 5-hydroxyindol-3-yl-acetic acid. NEUROCHEMICAL MARKERS OF ALCOHOLISM VULNERABILITY DOPAMINE Pharmacological properties Dopamine acts on at least five dopamine receptors, which are divided into two major groups: (1) the D1-like receptors (D1 and D5); (2) the D2-like receptors (D2, D3 and D4). All dopamine receptors are G-protein-coupled receptors, the D1 receptor stimulates adenylyl cyclase activity, whereas the D2 receptor inhibits adenylyl cyclase activity. Homovanillic acid (HVA) is the major metabolite of dopamine. Research findings In one challenge study, male alcoholics who had been abstinent for a period of 7 years exhibited reduced postsynapticdopamine-receptor sensitivity relative to controls. This was expressed as a reduced maximum GH response to the agonist apomorphine (Balldin et al., 1992). This report was consistent with the reduction in GH response (relative to controls) seen in alcoholics who had been abstaining from alcohol for periods ranging from 8 days to 6 months (Dettling et al., 1995). However, an earlier study showed that, after a withdrawal period of 4–7 days, alcoholics exhibited an elevated GH response to dopamine infusion, whereas their GH responses to apomorphine were similar to those of controls (Annunziato et al., 1983; Balldin et al., 1985). The dopamine receptor involved in GH secretion was thought to be a D2-type receptor, whereas D1 receptors are believed to be involved in prolactin secretion (Fabbrini et al., 1988). The reduction in postsynapticdopamine-D2-receptor sensitivity in alcoholics who had been abstaining from alcohol for ≥8 days might be a trait marker for alcoholism. This may be consistent with the dopaminergic hypothesis of alcoholism (Eckardt et al., 1998; Koob et al., 1998; Ikemoto and Panksepp, 1999). It may also account for the fact that, prior to detoxification, active alcoholics exhibit a reduced prolactin response to the antagonist haldol. This response reverted to control values 13 days after detoxification (Markianos et al., 2000). Baseline studies of HVA found that alcoholics had lower levels of this metabolite in their plasma than did control subjects (Fulton et al., 1995). However, the HVA levels found 527 in the CSF of alcoholics and in the plasma of male COA were similar to those found in controls (Roy et al., 1990; Limson et al., 1991; Howard et al., 1996; George et al., 1999; Petrakis et al., 1999). Early-onset alcoholics were found to have lower levels of HVA in their CSF than late-onset alcoholics (FilsAime et al., 1996). These results were contradicted by other studies, however, which found increased CSF HVA levels in early-onset alcoholics relative to late-onset alcoholics (George et al., 1999; Petrakis et al., 1999). In conclusion, these inconsistent baseline studies show that the changes in dopaminergic neurotransmission that are associated with alcoholism do not appear to fulfil either of the reviewed criteria for a trait marker of alcoholism. The challenge studies in alcoholics who had been abstaining for a protracted period of time showed a decreased dopamine receptor response that seems to fulfil one of the criteria for a trait marker, namely that it is present in alcoholics (Tables 1 and 4). NORADRENALINE Pharmacological properties Noradrenaline acts on various adrenergic receptors (two α receptors and two β receptors), all of which are G-protein coupled. The α1 adrenergic receptor is linked to the mobilization of intracellular calcium by phospholipase C, whereas the α2 adrenergic receptor inhibits adenylyl cyclase. The β1 and β2 adrenergic receptors stimulate adenylyl cyclase. A major metabolite of noradrenaline is 3-methoxy-4-hydroxyphenylglycol. Research findings Reduced numbers of melanin-containing noradrenergic neurons were found in the post-mortem locus coeruleus of alcoholics, which indicates a lower level of noradrenergic neurotransmission (Arango et al., 1994). This was inconsistent with the findings of Baker et al., (1994), however, which showed no differences post-mortem. In a baseline study, CSF and plasma were continuously sampled in controls and in alcoholics who had been abstaining for 38–124 days (Geracioti et al., 1994). The results showed that CSF Table 4. Dopamine studies Dopamine challenge studies Alcoholics vs controls: Decreased GH response to apomorphine (Balldin et al., 1992; Dettling et al., 1995) (long-term abstinence) Alcoholics vs controls: Increased GH response to dopamine infusion (Annuziato et al., 1983) (short-term abstinence) Alcoholics vs controls: Indifferent GH response to apomorphine (Balldin et al., 1985) (short-term abstinence) Alcoholics vs controls: Decreased prolactin response to haldol during alcohol intake, indifferent response after detoxification (Markianos et al., 2000) Dopamine baseline studies Alcoholics vs controls: Indifferent CSF HVA levels (Roy et al., 1990; Limson et al., 1991; George et al., 1999; Petrakis et al., 1999) Alcoholics vs controls: Decreased HVA plasma levels (Fulton et al., 1995) COA vs controls: Indifferent HVA plasma levels (Howard et al., 1996) Early-onset vs late-onset alcoholics: Decreased CSF HVA levels (Fils-Aime et al., 1996) Early-onset vs late-onset alcoholics: Increased CSF HVA levels (George et al., 1999; Petrakis et al., 1999) GH, growth hormone; HVA, homovanillic acid; CSF, cerebrospinal fluid; COA, children of alcoholics. J. E. RATSMA et al. 528 noradrenaline was lower in alcoholics than in controls, which was consistent with the findings of Arango et al. (1994). Although there were no differences in terms of the noradrenaline levels in plasma (Geracioti et al., 1994), alcoholics were found to have a lower basal level relative to controls (Ehrenreich et al., 1997). The same study reported that, following a challenge with human CRF or a stress test, the noradrenaline response was unaffected (Ehrenreich et al., 1997). In addition, alcoholics were found to have a blunted GH response to clonidine (an α2 adrenergic receptor agonist) in comparison to controls. The effect was found shortly after detoxification and also after 6 months of abstinence (Glue et al., 1989; Berggren et al., 2000). Similarly, in comparison to controls, alcoholics were found to have an enhanced cortisol response to yohimbine (an α2 adrenergic receptor antagonist). This reflects the downregulation of postsynaptic noradrenergic receptors that is observed in alcoholics (Krystal et al., 1996). In conclusion, both the basal studies of decreased noradrenaline levels in CSF (but not in plasma) and the challenge studies of receptor responsiveness showed that a decrease in noradrenergic neurotransmission seems to fulfil one criterion for a trait marker, that it should be present in alcoholics (Tables 1 and 5). β-ENDORPHIN Pharmacological properties Opioids act on three major classes of opiate receptors: µ, δ and κ. These G-protein-coupled receptors, which inhibit adenylyl cyclase, are distributed throughout the CNS. The distribution of β-endorphin, however, is somewhat restricted. It is primarily confined to neurons in the hypothalamus, which send projections to the periaqueductal grey region and to noradrenergic nuclei in the brain stem. Research findings Baseline studies in humans have shown that, in individuals at risk of alcoholism, the basal activity level of the endogenous opioid system might be lower than in individuals with a low risk of alcoholism (Volpicelli et al., 1990). Such a finding would be consistent with the opioid-deficiency hypothesis. This was supported by the fact that the β-endorphin levels in the plasma and CSF of alcoholics were lower than those found in controls (Genazzani et al., 1982; Aguirre et al., 1990). It was reported in one study that alcohol may have an equally strong effect on the central levels of β-endorphin as it does on peripheral levels (Peterson et al., 1996). A lower dose of naloxone completely blocked any reduction in synaptic opioid content and/or opioid receptor density in high-risk individuals. This indicates that endogenous hypothalamic opioid activity levels in these individuals are lower than those in low-risk subjects (Wand et al., 1998). Using a placebo, it was found that cortisol levels in high-risk subjects were higher than in low-risk subjects. This indicates that there is probably no increase in opioid receptor affinity, as this would result in more inhibitory tone, and lower cortisol levels. With regard to challenge studies, the opioid antagonist naloxone produced higher cortisol and β-endorphin responses in alcoholics than in controls. It also caused alcoholics to reduce their consumption of ethanol (Kemper et al., 1990; O’Malley et al., 1992; Volpicelli et al., 1992). The ingestion of a moderate dose of ethanol induced a dose-dependent increase in plasma β-endorphin levels in high-risk subjects, but not in low-risk subjects. Although these elevated levels were not produced by the peripheral adrenal cortisol system, the more central pituitary β-endorphin system showed an increased sensitivity to ethanol. This might mediate ethanol’s reinforcing effects in high-risk subjects (Gianoulakis et al., 1989, 1996). These baseline and challenge studies are consistent with the opioid-deficiency hypothesis. In a twin study, the inter-individual difference in β-endorphin response to alcohol was found to be heritable (Froehlich et al., 2000). In conclusion, the measurement of decreased β-endorphin baseline activity appears to fulfil two of the reviewed criteria for a trait marker of alcoholism. These are lower β-endorphin levels in alcoholics and decreased opioid receptor density in COA. However, the measurement of increased β-endorphin responsiveness seems to fulfil three such criteria in that it is heritable, it is present in alcoholics and it is state independent (present in COA). (Tables 1 and 6). Table 5. Noradrenaline studies Noradrenaline post-mortem studies Alcoholics vs controls: Decreased number of noradrenergic neurons in locus ceruleus (Arango et al., 1994) Alcoholics vs controls: Indifferent number of noradrenergic neurons in locus ceruleus (Baker et al., 1994) Noradrenaline challenge studies Alcoholics vs controls: Indifferent response of noradrenaline in plasma after CRF or a stress test (Geraciotti et al., 1994; Ehrenreich et al., 1997) Alcoholics vs controls: Increased cortisol response to antagonist yohimbine (Krystal et al., 1996) Alcoholics vs controls: Decreased growth hormone response to agonist clonidine (Glue et al., 1989; Berggren et al., 2000) CSF, cerebrospinal fluid; CRF, corticotropin-releasing factor. Noradrenaline baseline studies Alcoholics vs controls: Decreased levels of noradrenaline in CSF (Geraciotti et al., 1994) Alcoholics vs controls: Indifferent levels of noradrenaline in plasma (Geraciotti et al., 1994) Alcoholics vs controls: Decreased levels of noradrenaline in plasma (Ehrenreich et al., 1997) NEUROCHEMICAL MARKERS OF ALCOHOLISM VULNERABILITY 529 Table 6. β-Endorphin studies β-Endorphin challenge studies Alcoholics vs controls: Increased cortisol response to naloxone (Kemper et al., 1990) Alcoholics vs controls: Increased β-endorphin response to naloxone (O’Malley et al., 1992) Alcoholics vs controls: Decreased alcohol consumption with naloxone (Volpicelli et al., 1992) COA vs controls: Increased β-endorphin response to alcohol (Gianoulakis et al., 1989, 1996) β-Endorphin baseline studies Alcoholics vs controls: Decreased basal level of β-endorphin in plasma (Aguirre et al., 1990) Alcoholics vs controls: Decreased basal level of β-endorphin in CSF (Genazzani et al., 1982) COA vs controls: Decreased opioid receptor density (Wand et al., 1998) CSF, cerebrospinal fluid; COA, children of alcoholics. GENERAL CONCLUSIONS AND COMMENTS The present report reviewed five neurotransmitters: GABA, serotonin, dopamine, noradrenaline and β-endorphin (see Table 1). Two possible neurochemical markers seemed to fulfil the three reviewed criteria of a trait marker of alcoholism. The first possible marker is the measurement of increased baseline activity of the serotonin transporter in platelets. This is heritable, and is present in both long-term abstinent alcoholics and in COA. The second possible marker is the measurement of increased responsiveness of the pituitary β-endorphin system to challenges. This is heritable, and is present in both alcoholics and COA. Both possible neurochemical markers have yet to be assessed in family cosegregation studies to determine whether the marker segregates with alcoholism within families, to prevent falsepositive conclusions. It can be concluded from the GABA challenge studies in alcoholics and in COA that the measurement of decreased responsiveness in GABA neurotransmission fulfils two of the reviewed criteria for a trait marker: it is present in both alcoholics and in COA. Further studies on the question of heritability are needed. Another possible trait marker is the measurement of reduced baseline GABA levels in plasma. Its properties must be further studied in COA, to assess the state independence of these effects. Studies on serotonin activity in alcoholics and COA have shown that increases in serotonin transporter activity can be masked by the recent consumption of alcohol, which may lead to a decrease in serotonin transporter activity in active and newly abstinent alcoholics. This may also hold true for the use of challenge studies to determine the presence of a decreased postsynaptic-serotonin-receptor response in alcoholics, versus an elevated response in COA. The serotonin post-mortem studies that have been reviewed also showed decreased binding to the serotonin transporter and receptor. This may be consistent with a masking effect produced by alcohol (Menninger et al., 1998). Although the challenge and baseline studies of dopamine activity in alcoholics produced contradictory results, decreased receptor reactivity was found in alcoholics who had been abstaining for a protracted period of time. The measurement of dopamine levels in plasma poses certain problems; however the use of neuro-imaging techniques (which measure central dopaminergic functions) holds considerable promise for the future. Indices of changes in the noradrenaline system all corresponded to a fall in noradrenaline baseline levels, and to a reduction in postsynaptic-α2-adrenergic-receptor reactivity. There may be reduced activity in the noradrenaline system, of which the assessment might represent a trait marker for alcoholism. However, further studies are required on the presence of these possible markers in COA, and on their heritability. The reduced baseline level of β-endorphin in alcoholics, together with reduced opioid receptor density in COA and an elevated β-endorphin response to alcohol and naloxone in alcoholics and COA, might be consistent with the opioiddeficiency hypothesis. The finding that inter-individual differences in challenged β-endorphin levels are heritable suggests that the measurement of increased responsiveness of the β-endorphin system may be a trait marker for alcoholism. In the course of producing this review, no familial cosegregation studies were found on possible neurochemical trait markers and alcoholism. Such studies would have been of use in addressing the issue of possible false-positive conclusions. However, many familial and population-based linkage studies have been carried out into candidate, neurochemistryrelated, alcoholism genes. The Collaborative Study of the Genetics of Alcoholism (COGA) has performed linkage analyses in a large number of families with severe alcoholism. The COGA is a multicentre study for the detection and characterization of genes that influence susceptibility to alcohol dependence and related phenotypes. Data from COGA have been used to study the linkage of vulnerability for alcoholism on regions of chromosomes 1, 2 and 7 (Reich et al., 1998). Neurogenetic candidate genes on chromosomes 4 and 11 have been reported in a genome-wide scan for genetic linkage to alcohol dependence in a South-western American Indian Tribe (Long et al., 1998). The regions in question are those near the β1 GABA receptor gene on chromosome 4, and near the tyrosine hydroxylase and dopamine D4 receptor genes on chromosome 11. Genome-wide screenings must be followed by investigations in alcoholics and COA, to determine whether the candidate gene has a real causal relationship with the development of alcoholism over time. As pointed out in the review by Rutter (1994), it is essential that the component of a multidimensional phenotype of alcoholism be accurately defined J. E. RATSMA et al. 530 and that it be strongly homogeneous in genetic terms. This indicates that further research is needed on the aetiological heterogeneity, mode of transmission and incomplete penetrance of the genes involved in alcoholism (Devor et al., 1994). In conclusion, this review presents three main items. First, two possible neurochemical markers fulfil three criteria of a trait marker for alcoholism. The markers in question are the measurements of increased baseline activity of the serotonin transporter in platelets and increased responsiveness of the pituitary β-endorphin system to challenges. Secondly, a description of changes in GABA, dopamine and noradrenaline neurotransmitter systems is presented. As yet, however, these do not fulfil all three reviewed criteria for a trait marker of alcoholism. Thirdly, we would like to emphasize that the use of high-risk groups is essential (a view supported by the many inconsistent studies in COA). Such an approach facilitates investigations into the state independence of a trait marker. This is due to the marked influence of alcohol on neurotransmitter systems, which results in state-dependent changes after alcohol use. It also makes it possible to determine (preferably by the use of longitudinal data) whether an index of a change within a neurotransmitter system has a causal relationship with the development of alcoholism. If so, this would mean that it could serve as a trait marker. Trait markers for alcoholism which do not yet fulfil all of the criteria may do so in the future, once they have been more extensively studied. REFERENCES Abi-Dargham, A., Krystal, J. H., Anjilvel, S., Scanley, B. E., Zoghbi, S., Baldwin, R. M., Rajeevan, N., Ellis, S., Petrakis, I. L., Seibyl, J. P., Charney, D. S., Laruelle, M. and Innis, R. B. (1998) Alterations of benzodiazepine receptors in type II alcoholic subjects measured with SPECT and [123I] Iomazenil. American Journal of Psychiatry 155, 1550–1555. Aguirre, J. C., Del Arbol, J. L., Raya, J., Ruiz-Requena, M. E. and Irles, J. R. (1990) Plasma beta-endorphin levels in chronic alcoholics. Alcohol 7, 409–412. Ahlenius, S., Carlsson, A., Engel, J., Svensson, T. and Södersten, P. (1973) Antagonism by alpha methyltyrosine of the ethanol-induced stimulation and euphoria in man. Clinical Pharmacology and Therapeutics 14, 586–591. Annunziato, L., Amoroso, S., Di Renzo, G., Argenzio, F., Aurilio, C., Grella, A. and Quattrone, A. (1983) Increased GH responsiveness to dopamine receptor stimulation in alcohol addicts during the late withdrawal. Life Sciences 33, 2651–2655. Arango, V., Underwood, M. D. and Mann, J. J. (1994) Fewer pigmented neurons in the locus coeruleus of uncomplicated alcoholics. Brain Research 650, 1–8. Badawy, A. A. (1999) Tryptophan metabolism in alcoholism. Advances in Experimental Medicine and Biology 467, 265–274. Baker, K.G., Halliday, G. M. and Harper, C. G. (1994) Effect of chronic alcohol consumption on the human locus coeruleus. Alcoholism: Clinical and Experimental Research 18, 1491–1496. Balldin, J., Alling, C., Gottfries, C. G., Lindsted, G. and Langstrom, G. (1985) Changes in dopamine receptor sensitivity in humans after heavy alcohol intake. Psychopharmacology 86, 142–146. Balldin, J., Berggren, U. and Lindstedt, G. (1992) Neuroendocrine evidence for reduced dopamine receptor sensitivity in alcoholism. Alcoholism: Clinical and Experimental Research 16, 822–825. Balldin, J., Berggren, U., Engel, J. and Eriksson, M. (1994) Neuroendocrine evidence for reduced serotonergic neurotransmission during heavy drinking. Alcoholism: Clinical and Experimental Research 18, 822–825. Ballenger, J. C., Goodwin, F. K., Major, L. F. and Brown, G. L. (1979) Alcohol and central serotonin metabolism in men. Archives of General Psychiatry 36, 224–227. Banki, C. M. (1978) 5-Hydroxytryptamine content of whole blood in psychiatric illness and alcoholism. Acta Psychiatrica Scandinavica 57, 232–238. Banki, C. M. (1981) Factors influencing monoamine metabolites and tryptophan in patients with alcohol dependence. Journal of Neural Transmission 50, 89–101. Banki, C. M. and Molnar, G. (1981) Cerebrospinal fluid 5hydroxyindoleacetic acid as an index of central serotonergic processes. Psychiatry Research 5, 23–32. Begleiter, H. and Porjesz, B. (1988) Potential biological markers in individuals at high risk for developing alcoholism. Alcoholism: Clinical and Experimental Research 11, 477–480. Benjamin, D., Grant, E. R. and Pohorecky, L. A. (1993) Naltrexone reverses ethanol-induced dopamine release in the nucleus accumbens in awake freely moving rats. Brain Research 621, 137–140. Berggren, U., Fahlke, C., Norrby, A., Zachrisson, O. and Balldin, J. (2000) Subsensitive alpha-2-adrenoceptor function in male alcoholdependent individuals during 6 months of abstinence. Drug and Alcohol Dependence 57, 255–260. Berrettini, W. H., Nurnberger, J. I., Hare, T., Gershon, E. S. and Post, R. M. (1982) Plasma and CSF GABA in affective illness. British Journal of Psychiatry 141, 483–487. Blakely, R. D., Berson, H. E., Fremeau, R. T., Caron, M. G., Peek, M. M., Prince, H. K. and Bradley, C. C. (1991) Cloning and expression of a functional serotonin transporter from rat brain. Nature 354, 66–70. Blum, K. (1983) Alcohol and central neurosystem peptides. Substance and Alcohol Actions/Misuse 4, 73–87. Bohman, M., Sigvardsson, S. and Cloninger, C. R. (1981) Maternal inheritance of alcohol abuse: cross-fostering analysis of adopted women. Archives of General Psychiatry 38, 965–969. Borg, S., Kvande, H., Liljeberg, P., Mossberg, D. and Valverius, P. (1985) 5-Hydroxyindoleacetic acid in cerebrospinal fluid in alcoholic patients under different clinical conditions. Alcohol 2, 415–418. Brown, Z. W. and Amit, Z. (1982) The effects of selective catecholamine depletions by 6-hydroxydopamine on ethanol preferences in rats. Neuroscience Letters 5, 333–336. Buydens-Branchey, L., Branchey, M. H., Noumair, D. and Lieber, C. S. (1989) Age of alcoholism onset: II. Relationship to susceptibility to serotonin precursor availability. Archives of General Psychiatry 46, 231–236. Cadoret, R. J., Cain, C. A., Troughton, E. and Heywood, E. (1985) Alcoholism and antisocial personality: interrelationships, genetic and environmental factors. Archives of General Psychiatry 38, 965–969. Chen, H.-T., Casanova, M. F., Kleinman, J. E., Zito, M., Goldman, D. and Linnoila, M. (1991) 3H-Paroxetine binding in brains of alcoholics. Psychiatry Research 38, 293–299. Cloninger, C. R. (1987) Neurogenetic adaptive mechanisms in alcoholism. Science 236, 410–416. Cloninger, C. R. (1994) Turning point in the design of linkage studies of schizophrenia. American Journal of Medical Genetics (Neuropsychiatric Genetics) 54, 83–92. Cloninger, C. R., Bohman, M., Sigvardsson, S. and Von Knorring, A. L. (1985) Psychopathology in adopted-out children of alcoholics: the Stockholm adoption study. In Recent Developments in Alcoholism, Galanter, M. ed., pp. 37–51. Plenum Press, New York. Coffman, J. A. and Petty, F. (1985) Plasma GABA levels in chronic alcoholics. American Journal of Psychiatry 142, 1204–1205. Cowley, D. S., Roy-Byrne, P. P., Greenblatt, D. J., Kramer, G. L. and Petty, F. (1996) Effect of diazepam on plasma γ-aminobutyric acid in sons of alcoholic fathers. Alcoholism: Clinical and Experimental Research 20, 343–347. Dettling, M., Heinz, A., Dufeu, P., Rommelspacher, H., Graf, K.-J. and Schmidt, L. G. (1995) Dopaminergic responsivity in alcoholism: trait, state or residual marker? American Journal of Psychiatry 152, 1317–1321. Deutsch, J. A. and Howarth, C. I. (1963) Some tests of a theory of intracranial self-stimulation. Psychological Review 70, 444–460. Devor, E. J. (1994) A developmental-genetic model of alcoholism: implications for genetic research. Journal of Consulting and Clinical Psychology 62, 1108–1115. Dillon, K. A., Gross-Isseroff, R., Israeli, M. and Biegon, A. (1991) Autoradiographic analysis of serotonin 5-HT1A receptor binding in NEUROCHEMICAL MARKERS OF ALCOHOLISM VULNERABILITY the human brain post mortem: effects of age and alcohol. Brain Research 554, 56–64. Dodd, P. R., Thomas, G. J., Harper, C. G. and Kril, J. J. (1992) Amino acid neurotransmitter receptor changes in cerebral cortex in alcoholism: effect of cirrhosis of the liver. Journal of Neurochemistry 59, 1506–1515. Eckardt, M. J., File, S. E., Gessa, G. L., Grant, K. A., Guerri, C., Hoffman, P. L., Kalant, H., Koob, G. F., Li, T.-K. and Tabakoff, B. (1998) Effects of moderate alcohol consumption on the central nervous system. Alcoholism: Clinical and Experimental Research 22, 998–1040. Ehrenreich, H., Schuck, J., Stender, N., Pilz, J., Gefeller, O., Schilling, L., Poser, W. and Kaw, S. (1997) Endocrine and hemodynamic effects of stress versus systemic CRF in alcoholics during early and medium term abstinence. Alcoholism: Clinical and Experimental Research 21, 1285–1293. Erickson, C. K. (1990) Reviews and comments on alcohol research. Alcohol 7, 557–558. Ernouf, D., Compagnon, P., Lothion, P., Narcisse, G., Bénard, J. Y. and Daoust, M. (1993) Platelets 3H 5-HT uptake in descendants from alcoholic patients: a potential risk factor for alcohol dependence? Life Sciences 52, 989–995. Eskay, R. and Linnoila, M. (1991) Potential biochemical markers for the predisposition toward alcoholism. In Recent Developments in Alcoholism, Vol. 9, Children of Alcoholics, Galanter, M. ed., pp. 41–51. Plenum Press, New York. Fabbrini, G., Braun, A., Mouradian, M. M., Tamminga, C. A. and Chase, T. N. (1988) Dopamine D-1 receptor agonist stimulation of prolactin secretion in man. Journal of Neural Transmission 71, 159–163. Farren, C. K. and Tipton, K. F. (1999) Trait markers for alcoholism: clinical utility. Alcohol and Alcoholism 34, 649–665. Fils-Aime, M.-L., Eckhardt, M. J., George, D. T., Brown, G. L., Mefford, I. and Linnoila, M. (1996) Early-onset alcoholics have lower cerebrospinal fluid 5-hydroxyindoleacetic acid levels than late-onset alcoholics. Archives of General Psychiatry 53, 211–216. Froehlich, J. C., Zink, R. W., Li, T.-K. and Christian, J. C. (2000) Analysis of heritability of hormonal responses to alcohol in twins: beta-endorphin as a potential biomarker of genetic risk for alcoholism. Alcoholism: Clinical and Experimental Research 24, 265–277. Frye, G. D. and Breese, G. R. (1982) GABAergic modulation of ethanol-induced motor impairment. Journal of Pharmacology and Experimental Therapeutics 223, 750–756. Fulton, M. K., Kramer, G., Moeller, F. G., Chae, Y., Isbell, P. G. and Petty, F. (1995) Low plasma homovanillic acid levels in recently abstinent alcoholic men. American Journal of Psychiatry 152, 1819–1820. Genazzani, A. R., Nappi, G., Facchinetti, F., Mazzella, G. L., Parrini, D., Sinforiani, E., Petraglia, F. and Savoldi, F. (1982) Central deficiency of β-endorphin in alcohol addicts. Journal of Clinical Endocrinology and Metabolism 55, 583–586. George, D. T., Benkelfat, C., Rawlings, R. R., Eckardt, M. J., Phillips, M. J., Nutt, D. J., Wynne, D., Murphy, D. L. and Linnoila, M. (1997) Behavioral and neuroendocrine responses to m-chlorophenylpiperazine in subtypes of alcoholics and in healthy comparison subjects. American Journal of Psychiatry 154, 81–87. George, D. T., Rawlings, R. R., Eckardt, M. J., Phillips, M. J., Shoaf, S. E. and Linnoila, M. (1999) Buspirone treatment of alcoholism: age of onset, and cerebrospinal fluid 5-hydroxyindolacetic acid and homovanillic acid concentrations, but not medication treatment, predict return to drinking. Alcoholism: Clinical and Experimental Research 23, 272–278. Geracioti, T. D., Loosen, P. T., Ebert, M. H., Ekhator, N. N., Burns, D., Nicholson, W. E. and Orth, D. N. (1994) Concentrations of corticotropin-releasing hormone, norepinephrine, MPHG, 5-hydroxyindoleacetic acid, and tryptophan in the cerebrospinal fluid of alcoholic patients: serial sampling studies. Neuroendocrinology 60, 635–642. Gershon, E. S. and Goldin, L. R. (1986) Clinical methods in psychiatric genetics. I. Robustness of genetic marker investigative strategies. Acta Psychiatrica Scandinavica 74, 113–118. Gessa, G. L., Muntoni, F., Collu, M., Vargiu, L. and Mereu, G. (1985) Low doses of ethanol activate dopaminergic neurons in the ventral tegmental area. Brain Research 348, 201–203. 531 Gianoulakis, C., Beliveau, D., Angeliogianni, P., Meaney, M., Thavundayil, J., Tawar, V. and Duams, M. (1989) Different pituitary beta-endorphin and adrenal cortical response to ethanol in individuals with high and low risk for future development of alcoholism. Life Sciences 45, 1097–1109. Gianoulakis, C., Krishman, B. and Thavundayil, J. (1996) Enhanced sensitivity of pituitary β-endorphin to ethanol in subjects at high risk for alcoholism. Archives of General Psychiatry 53, 250–257. Glue, P., Sellman, J. D., Nicholls, M. G., Abbott, R., Joyce, P. R. and Nutt, D. J. (1989) Studies of alpha-2-adrenoreceptor function in abstinent alcoholics. British Journal of Addiction 84, 97–102 Goldin, L. R., Nurnberger, J. L. and Gershon, E. S. (1986) Clinical methods in psychiatric genetics. II. The high risk approach. Acta Psychiatrica Scandinavica 74, 119–128. Goldman, D. (1995) Identifying alcoholism vulnerability alleles. Alcoholism: Clinical and Experimental Research 19, 824–831. Goodwin, D. W., Schulsinger, F., Hermansen, L., Guze, S. B. and Winokur, G. (1973) Alcohol problems in adoptees raised apart from alcoholic biological parents. Archives of General Psychiatry 28, 238–243. Gross-Isseroff, R. and Biegon, A. (1988) Autoradiographic analysis of [3H]imipramine binding in the human brain post-mortem: effects of age and alcohol. Journal of Neurochemistry 51, 528–534. Heath, A. C., Bucholz, K. K., Madden, P. A. F., Dinwiddie, S. H., Slutske, W. S., Bierut, L. J., Statham, D. J., Dunne, M. P., Whitfield, J. B. and Martin, N. G. (1997) Genetic and environmental contributions to alcohol dependence risk in a national twin sample: consistency of findings in women and men. Psychological Medicine 27, 1381–1396. Heinz, A., Ragan, P., Jones, D. W., Hommer, D., Williams, W., Knable, M. B., Gorey, J. G., Doty, L., Geyer, C., Lee, K. S., Coppola, R., Weinberger, D. R. and Linnoila, M. (1998) Reduced central serotonin transporters in alcoholism. American Journal of Psychiatry 155, 1544–1549. Hibbeln, J. R., Linnoila, M., Umhau, J. C., Rawlings, R., George, D. T. and Salem, N., Jr (1998) Essential fatty acids predict metabolites of serotonin and dopamine in cerebrospinal fluid among healthy control subjects, and early- and late-onset alcoholics. Biological Psychiatry 44, 235–242. Hill, S. Y., Steinhauer, S. R., Smith, T. R. and Locke, J. (1991) Risk markers for alcoholism in high-density families. Journal of Substance Abuse 3, 351–369. Hommer, D., Andreasen, P., Rio, D., Williams, W., Ruttimann, U., Momenan, R., Zametkin, A., Rawlings, R. and Linnoila, M. (1997) Effects of m-chlorophenylpiperazide on regional brain glucose utilization: a positron emission tomographic comparison of alcoholic and control subjects. Journal of Neuroscience 17, 2796–2806. Howard, M. O., Cowley, D. S., Roy-Byrne, P. P. and Hopfenbeck, J. R. (1996) Tridimensional personality traits in sons of alcoholic and nonalcoholic fathers. Alcoholism: Clinical and Experimental Research 20, 445–448. Hubbell, C. L., Czirr, S. A., Hunter, G. A., Beaman, C. M., LeCann, N. C. and Reid, L. D. (1986) Consumption of ethanol solution is potentiated by morphine and attenuated by naloxone persistently across repeated daily administrations. Alcohol 3, 39–54. Hwang, B. H., Lumeng, L., Wu, J.-Y. and Li, T.-K. (1990) Increased number of GABAergic terminals in the nucleus accumbens is associated with alcohol preference in rats. Alcoholism: Clinical and Experimental Research 14, 503–507. Ikemoto, S. and Panksepp, J. (1999) The role of the nucleus accumbens dopamine in motivated behavior: a unifying interpretation with special reference to reward-seeking. Brain Research — Brain Research Reviews 31, 6–41. Imperato, A. and Di Chiara, G. (1986) Preferential stimulation of dopamine release in the nucleus accumbens of freely moving rats by ethanol. Journal of Pharmacology and Experimental Therapeutics 239, 219–228. Javors, M., Tioururine, M. and Prihoda, T. (2000) Platelet serotonin uptake is higher in early-onset than in late-onset alcoholics. Alcohol and Alcoholism 35, 390–393. Kemper, A., Koalick, F., Thiele, H., Retzow, A., Rathsack, R. and Nickel, B. (1990) Cortisol and beta-endorphin response in alcoholics and alcohol abusers following a high naloxone dosage. Drug and Alcohol Dependence 25, 319–326. 532 J. E. RATSMA et al. Kendler, K. S., Neale, M. C., Heath, A. C., Kessler, R. C. and Eaves, L. J. (1994) A twin-family study of alcoholism in women. American Journal of Psychiatry 151, 707–715. Kendler, K. S., Prescott, C. A., Neale, M. C. and Pedersen, N. L. (1997) Temperance board registration for alcohol abuse in a national sample of Swedish male twins born in 1902–1949. Archives of General Psychiatry 54, 178–184. Kent, T. A., Campbell, J. L., Pazdernik, T. L., Hunter, R., Gunn, W. H. and Goodwin, D. W. (1985) Blood platelet uptake of serotonin in alcoholic men. Journal of Studies on Alcohol 46, 357–359. Koob, G. F., Braestrup, C. and Thatcher Britton, K. (1986) The effects of FG 7142 and RO 15-1788 on the release of punished responding produced by chlordiazepoxide and ethanol in the rat. Psychopharmacology 90, 173–178. Koob, G. F., Roberts, A. J., Schulteis, G., Parsons, L. H., Heyser, C. J., Hyytiä, P., Merlo-Pich, E. and Weiss, F. (1998) Neurocircuitry targets in ethanol reward and dependence. Alcoholism: Clinical and Experimental Research 22, 3–9. Krystal, J. H., Webb, E., Cooney, N. L., Kranzler, H. R. and Charney, D. S. (1994) Specificity of ethanol-like effects elicited by serotonergic and noradrenergic mechanisms. Archives of General Psychiatry 51, 898–911. Krystal, J. H., Webb, E., Cooney, N. L., Kranzler, H. R., Southwick, S. W., Heninger, G. L. and Charney, D. S. (1996) Serotonergic and noradrenergic dysregulation in alcoholism: m-chlorophenylpiperazide and yohimbine effects in recently detoxified alcoholics and healthy subjects. American Journal of Psychiatry 153, 83–92. Levitan, E. S., Schofield, P. R., Burt, D. R., Rhee, L. M., Wisden, W., Köhler, M., Fujita, N., Rodriguez, H. F., Stephenson, A., Darlison, M. G., Barnard, E. A. and Seeburg, P. H. (1988) Structural and functional basis for GABAA receptor heterogeneity. Nature 335, 76–79. Lewohl, J. M., Crane, D. I. and Dodd, P. R. (1997) Expression of the α1, α2, and α3 isoforms of the GABAA receptor in human brain. Brain Research 751, 102–112. Limson, R., Goldman, D., Roy, A., Lamparski, D., Ravitz, B., Adinoff, B. and Linnoila, M. (1991) Personality and cerebrospinal fluid monoamine metabolites in alcoholics and controls. Archives of General Psychiatry 48, 437–441. Lingford-Hughes, A. R., Acton, P. D., Gacinovic, S., Suckling, J., Busatto, G. F., Boddington, S. J., Bullmore, E., Woodruff, P. W., Costa, D. C., Pilowsky, L. S., Ell, P. J., Marshall, E. J. and Kerwin, R. W. (1998) Reduced levels of GABA-benzodiazepine receptor in alcohol dependency in the absence of grey matter atrophy. British Journal of Psychiatry 173, 116–122. Linnoila, M., Virkkunen, M., Scheinin, M., Nuutila, A., Rimon, R. and Goodwin, F. K. (1983) Low cerebrospinal fluid 5-hydroxyindoleacetic acid concentration differentiates impulsive from nonimpulsive violent behavior. Life Sciences 33, 2609–2614. Long, J. C., Knowler, W. C., Hanson, R. L., Robin, R. W., Urbanek, M., Moore, E., Bennet, P. H. and Goldman, D. (1998) Evidence for genetic linkage to alcohol dependence on chromosome 11 from an autosome-wide scan in an American Indian Population. American Journal of Medical Genetics 81, 216–221. Markianos, M., Moussas, G., Lykouras, L. and Hatzimanolis, J. (2000) Dopamine receptor responsivity in alcoholic patients before and after detoxification. Drug and Alcohol Dependence 57, 261–265. McBride, W. J., Murphy, J. M., Lumeng, L. and Li, T.-K. (1988) Effects of Ro 15-4513, fluoxetine and desipramine on the intake of ethanol, water and food by the alcohol-preferring (P) and -nonpreferring (NP) lines of rats. Pharmacology, Biochemistry and Behavior 30, 1045–1050. McBride, W. J., Murphy, J. M., Lumeng, L. and Li, T.-K. (1990) Serotonin, dopamine and GABA involvement in alcohol drinking of selectively bred rats. Alcohol 7, 199–205. Meltzer, H. Y. and Arora, R. C. (1988) Genetic control of serotonin uptake in blood platelets: a twin study. Psychiatry Research 24, 263–269. Menninger, J. A., Baron, A. E. and Tabakoff, B. (1998) Effects of abstinence and family history for alcoholism on platelet adenylyl cyclase. Alcoholism: Clinical and Experimental Research 22, 1955–1961. Mitsuyama, H., Little, K. Y., Sieghart, W., Devaud, L. L. and Morrow, A. L. (1998) GABA(A) receptor alpha1, alpha4, and beta3 sub-unit mRNA and protein expression in the frontal cortex of human alcoholics. Alcoholism: Clinical and Experimental Research 22, 815–822. Moss, H. B., Yao, J. K., Burns, M., Maddock, J. and Tarter, R. E. (1990) Plasma GABA-like activity in response to ethanol challenge in men at high risk for alcoholism. Biological Psychiatry 27, 617–625. Murphy, J. M., Waller, M. B., Gatto, G. J., McBride, W. J., Lumeng, L. and Li, T.-K. (1988) Effects of fluoxetine on the intragastric selfadministration of ethanol in the alcohol-preferring P line of rats. Alcohol 5, 283–286. Nurnberger, J. L., Jr (1992) Should a biologic marker be sensitive and specific? Acta Psychiatrica Scandinavica 86, 1–4. Olds, J. and Milner, P. (1954) Positive reinforcement produced by electrical stimulation of septal area and of other regions of rat brain. Journal of Comparative and Physiological Psychology 47, 419–427. O’Malley, S. S., Jaffe, A. J., Chang, G., Schottenfeld, R. S., Meyer, R. E. and Rounsaville, B. (1992) Naltrexone and coping skills therapy for alcohol dependence: a controlled study. Archives of General Psychiatry 49, 881–887. Peterson, J. B., Phil, R. O., Gianoulakis, C., Conrod, P., Finn, P. R., Steward, S. H., LeMarquand, D. G. and Bruce, K. R. (1996) Ethanolinduced change in cardiac and endogenous opiate function and risk for alcoholism. Alcoholism: Clinical and Experimental Research 20, 1542–1552. Petrakis, I. L., Trevisan, L., D’Souza, C., Gil, R., Krasnicki, S., Webb, E., Heninger, G., Cooney, N. and Krystal, J. H. (1999) CSF monoamine metabolite and beta endorphin levels in recently detoxified alcoholics and healthy controls: prediction of alcohol cueinduced craving? Alcoholism: Clinical and Experimental Research 23, 1336–1341. Petty F., Fulton, M., Moeller, F. G., Kramer, G., Wilson, L., Fraser, K. and Isbell, P. (1993) Plasma gamma-aminobutyric acid (GABA) is low in alcoholics. Psychopharmacology Bulletin 29, 277–281. Raleigh, M. J., Brammer, G. L., McGuire, M. T., Pollack, D. B. and Yuwiler, A. (1992) Individual differences in basal cisternal cerebrospinal fluid 5-HIAA and HVA in monkeys: the effects of gender, age, physical characteristics and matrilineal influences. Neuropsychopharmacology 7, 295–304. Ratsma, J. E., Gunning, W. B., Leurs, R. and Schoffelmeer, A. N. M. (1999) Platelet adenylyl cyclase activity as a biochemical marker for predisposition to alcoholism. Alcoholism: Clinical and Experimental Research 23, 600–604. Rausch, J. L., Monteiro, M. G. and Schuckit, M. A. (1991) Platelet serotonin uptake in men with family histories of alcoholism. Neuropsychopharmacology 4, 83–86. Reed, T., Page, W. F., Viken, R. J. and Christian, J. C. (1996) Genetic predisposition to organ specific end points of alcoholism. Alcoholism: Clinical and Experimental Research 20, 1528–1533. Reich, T., Edenberg, H. J., Goate, A., Williams, J. T., Rice, J. P., Van Eerdewegh, P., Foroud, T., Hesselbrock, V., Schuckit, M. A., Bucholz, K., Porjesz, B., Li, T.-K., Conneally P. M., Nurnberger, J. I., Tischfield, J. A., Crowe, R. R., Cloninger, C. R., Wu, W., Shears, S., Carr, K., Crose, C., Willig, C. and Begleiter, H. (1998) Genome-wide search for genes affecting the risk for alcohol dependence. American Journal of Medical Genetics (Neuropsychiatric Genetics) 81, 207–215. Reid, L. D. and Hunter, G. A. (1984) Morphine and naloxone modulate intake of ethanol. Alcohol 1, 33–37. Reid, L. D., Delconte, J. D., Nichols, M. L., Bilsky, E. J. and Hubbell, C. L. (1991) Tests of opioid deficiency hypotheses of alcoholism. Alcohol 8, 247–257. Romanov, K., Kaprio, J. and Rose, R. J. (1991) Genetics of alcoholism: effects of migration on concordances rates among male twins. Alcohol and Alcoholism 26 (Suppl. 1), 137–140. Routtenberg, A. (1978) The reward system of the brain. Scientific American 239, 122–131. Roy, A., Lamparski, D., De Jong, J., Adinoff, B., Ravitz, B., George, D. T., Nutt, D. and Linnoila, M. (1990) Cerebrospinal fluid monoamine metabolites in alcoholic patients who attempt suicide. Acta Psychiatrica Scandinavica 81, 58–61. Rutter, M. (1994) Psychiatric genetics: research challenges and pathways forward. American Journal of Medical Genetics (Neuropsychiatric Genetics) 54, 185–198. NEUROCHEMICAL MARKERS OF ALCOHOLISM VULNERABILITY Schaefer, G. J. (1988) Opiate antagonists and rewarding brain stimulation. Neuroscience and Biobehavioral Reviews 12, 1–17. Schuckit, M. A. (1999) New findings in the genetics of alcoholism. Journal of the American Medical Association 281, 1875–1876. Schuckit, M. A. and Smith, T. L. (1996) An 8-year follow-up of 450 sons of alcoholic and control subjects. Archives of General Psychiatry 53, 202–210. Schuckit, M. A., Parker, D. C. and Rossman, L. R. (1983) Ethanolrelated prolactin response and risk for alcoholism. Biological Psychiatry 18, 1153–1159. Schulz, K. P., McKay, K. E., Newcorn, J. H., Sharma, V., Gabriel, S. and Halperin, J. M. (1998) Serotonin function and risk for alcoholism in boys with attention-deficit hyperactivity disorder. Neuropsychopharmacology 18, 10–17. Sher, K. J., Walitzer, K. S., Wood, P. K. and Brent, E. E. (1991) Characteristics of children of alcoholics: putative risk factors, substance use and abuse, and psychopathology. Journal of Abnormal Psychology 100, 427–448. Suzdak, P. D., Schwartz, R. D., Skolnick, P. and Paul, S. M. (1986) Ethanol stimulates gamma-aminobutyric acid receptor-mediated chloride transport in rat brain synaptoneurosomes. Proceedings of the National Academy of Sciences of the United States of America 83, 4071–4075. Tran, V. T., Snyder, S. H., Major, L. F. and Hawley, R. J. (1981) GABA receptors are increased in brains of alcoholics. Annals of Neurology 9, 289–292. Treu, W. R., Heath, A. C., Bucholz, K., Slutske, W., Romeis, J., Scherrer, J. F., Lin, N., Eisen, S. A., Goldberg, J., Lyons, M. J. and Tsuang, M. T. (1996) Models of treatment seeking for alcoholism: the role of genes and environment. Alcoholism: Clinical and Experimental Research 20, 1577–1581. Van der Stelt, O. (1999) Visual P3 as a potential vulnerability marker of alcoholism: evidence from the Amsterdam study of children of alcoholics. Alcohol and Alcoholism 34, 267–282. Van Ree, J. M., Smyth, D. G. and Colpaert, F. C. (1979) Dependence creating properties of lipotropin c-fragment (β-endorphin): evidence for its internal control of behavior. Life Sciences 24, 495–502. 533 Vescovi, P. P. and Coiro, V. (1995) Gamma-hydroxy-butyric acid is unable to stimulate growth hormone secretion in early abstinent alcoholic men. Alcologia 7, 129–132. Vescovi, P. P. and Coiro, V. (1997) Persistence of defective serotonergic and GABAergic controls of growth hormone secretion in long-term abstinent alcoholics. Alcohol and Alcoholism 32, 85–90. Virkkunen, M., Rawlings, R., Tokola, R., Poland, R. E., Guidotti, A., Nemeroff, C., Bissette, G., Kalogeras, K., Karonen, S. L. and Linnoila, M. (1994) CSF biochemistries, glucose metabolism, and diurnal activity rhythms in alcoholic, violent offenders, fire setters, and healthy volunteers. Archives of General Psychiatry 51, 20–27. Volkow, N. D., Wang, G.-K., Hitzemann, R., Fowler, J. S., Wolf, A. P., Pappas, N., Biegon, A. and Dewey, S. L. (1993) Decreased cerebral response to inhibitory neurotransmission in alcoholics. American Journal of Psychiatry 150, 417–422. Volkow, N. D., Wang, G.-K., Begleiter, H., Hitzemann, R., Pappas, N., Burr, G., Pascani, K., Wong, C., Fowler, J. S. and Wolf, A. P. (1995) Regional brain metabolic response to lorazepam in subjects at risk for alcoholism. Alcoholism: Clinical and Experimental Research 19, 510–516. Volpicelli, J., Davis, M. A. and Olgin, J. E. (1985) Naltrexone blocks the post-shock increase of ethanol consumption. Life Sciences 38, 841–847. Volpicelli, J., O’Brien, C., Alterman, A. and Hayashida, M. (1990) Naltrexone in the treatment of alcohol dependence: initial observations. In Opioids, Bulimia and Alcohol Abuse and Alcoholism, Reid, L. D. ed., pp. 195–214. Springer-Verlag, New York. Volpicelli, J., O’Brien, C., Alterman, A. and Hayashida, M. (1992) Naltrexone in the treatment of alcohol dependence. Archives of General Psychiatry 49, 867–880. Wand, G. S., Mangold, D., El Deiry, S., McCaul, M. E. and Hoover, D. (1998) Family history of alcoholism and hypothalamic opioidergic activity. Archives of General Psychiatry 55, 1114–1119. Wise, R. A. and Bozarth, M. A. (1987) A psychomotor stimulant theory of addiction. Psychological Review 94, 469–492. Wise, R. A. and Rompre, P.-P. (1989) Brain dopamine and reward. Annual Review of Psychology 40, 191–225.