* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cells, Tissues
Multielectrode array wikipedia , lookup
Subventricular zone wikipedia , lookup
Development of the nervous system wikipedia , lookup
Electrophysiology wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Neuroregeneration wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Neuroanatomy wikipedia , lookup
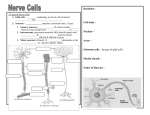
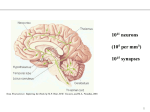
INTRODUCTION TO CELLS & TISSUES By Vijay Kapal Graduate Studies Course CMM 5001 The Pathological Basis Of Disease Fertilization Fertilization of egg by the sperm Sperm Egg + (23 Chromo) Sperm (23 Chromo) Fertilized egg (Zygote) (46 Chromosomes) Ovum (Egg) Human body Sperm Zygote Implantation Zygote Blastocyst Uterus Uterine glands Maternal blood vessels 3-layered Flat Embryo Ectoderm (1) Mesoderm (3) Endoderm (2) Fertilized egg or Zygote (Single cell) 3-layers of cells All Tissues & Organs of Human body Human Genome Nucleus Cytoplasm Cell membrane Cell Each cell has 46 chromosomes Form 23 homologous pairs Each parent contributes = 23 Autosomes = 44 Chromosomes (2N = 46) Sex chromosomes = 2 Each autosome of a homologous pair look alike (Male = XY, Female = XX) But each sex chromosome do not look alike Cell Cycle Paclitaxel Vincristine Vinblastine Colchicine Nondividing cells (Fixed postmitotics) M G0 G1 Resting cells (Reverting postmitotics) G2 Bleomycin Etoposide S Methotrexate Mitosis & Meiosis A Homologous Pair (2 Chromosomes) 1 1 pair 2 23 pair 1st Division 46 2nd Division Daughter Somatic Cells (2) Gametes (4) Meiosis Takes place only in testes and ovaries Is a reductional division Main purpose is to reduce the number of chromosomes from 2N to 1N in sperms & eggs (Chromosomes of each homologous pair will separate from each other) Homologous pair = 1 chromosome from each parent (at fertilization) 2N = 46 chromosomes (2 sets) 1N = 23 chromosomes (1set) So Sperm = 1N chromosomes (23) Egg = 1N chromosomes (23) Fertilization restores chromosome number again to 2N = 46 chromosomes (2 sets) Human Body Cells Tissues Cell Organs Human body Tissue Cell Organelles • Nucleus • Rough ER • Smooth ER • Golgi Complex • Lysosomes • Peroxisomes • Mitochondria • Cell Membrane • Cell cytoskeleton Chomatin, Transcription Protein synthesis & Segregation Fat & Steroid synthesis & Detoxification Concentrating, Modifying & Packaging of secretory products Intracellular digestion Contain oxidative enzymes; Use catalase to degrade H2O2 = H2O + O2 Oxydative phosphorylation & ATP production Lipid bilayer layer with intramembranous proteins Actin filaments, Microtubules, intermediate filaments Cell Organelles Mitochondria Lysozome Golgi Nucleus Rough ER Cells, Tissues & Various Topics Of Research • • • • • • • • • • • Subcellular localisation & trafficking of molecules and oganelles Cell-cell and cell-extracellular matrix interactions Cell cytoskeleton and receptor dynamics and functions Cell and tissue differentiation and remodelling Genetically engineered cells and tissues Three-dimensional reconstructions, particularly of expression patterns over time Cell cycle and cell lineage analysis involving gene expression profiles Apoptosis Gene expression analysis from histological preparations Functional genomics & proteomics Techniques used in molecular histology Epithelial Tissue Outer layer of skin Inner lining of trachea Inner lining of ducts of sweat glands General Features • • • • • • • • Diversity Metaplasia Lining and Covering Basal Lamina Renewal Avascularity Cell Packing Derivation Classifying Principles 1. Number of cell layers: 1. Simple epithelia 2. Stratified epithelia 3. Pseudostratified epithelia 2. Shape of the surface cells: 1. Squamous cells 2. Cuboidal cells 3. Columnar cells 3. Luminal surface modifications: 1. Microvilli (Brush border) 2. Cilia 3. Stereocilia Specific Epithelial Types • • • • • Simple squamous epithelium: Simple cuboidal epithelium: Simple columnar epithelium: Pseudostratified epithelium: Stratified Squamous epithelium: a) Keratinized b) Nonkeratinized • Stratified cuboidal epithelium: • Stratified columnar epithelium: • Transitional epithelium: Types of Epithelia Simple squamous Stratified squamous Simple cuboidal stratified cuboidal Simple columnar Pseudostratified Transitional Full Empty Bladder Kidney (Epithelium) Simple squamous Simple cuboidal Kidney Tubules Small Intestine (Simple Columnar) Absorptive cells Nucleus Brush border Lamina propria Lumen of gut Esophagus (Stratified Squamous) Epithelium Lamina propria Skin (Stratified Squamous) Epidermis (Epithelium) Dermis (Connective tissue) Trachea (Pseudostratified Epithelium) Epithelium Cilia Ciliated cells Goblet cells Basal lamina Lamina propria Ureter (Transitional Epithelium) Epithelium Lumen Basal lamina Lamina propria Basal Lamina • • Next to epithelia an acellular sheet like structure is the Basal Lamina. Component Layers & Constinuent Macromolecules: A. Component Layers Lamina lucida Lamina densa B. Constituent Macromolecules Lamina lucida (Laminin that binds to cell surface integrins, collagen IV) Lamina densa (Type IV Collagen) Basement Membrane: Basal lamina accompanied by reticular lamina (Type III Collagen) is called the basement membrane. Functions: Forms sieve-like selective barrier between the epithelia & connective tissue. Aids in cell organization, cell adhesion & maintainence of cell shape. Has a role in maintaining specific cell function. Helps guide migrations of cells during development and regeneration of injured tissue Polarity & Specialization of Epithelial Cells A. B. C. D. Specialization of the Apical Surface: 1. Microvilli (Enterocytes & Proximal convoluted tubule cells)) 2. Cilia (Trachea, Bronchus etc.) 3. Stereocilia (Epididymis) 4. Flagella Specialization of the Lateral Surfaces: 1. Zonula occludens (Tight junctions) 2. Zonula adherens (Intermediate junctions) 3. Macula adherens (Desmosomes) 4. Gap junction (Nexus) Specialization of the Basal Surface: 1. Basal lamina 2. Hemidesmosome 3. Sodium-potassium ATPase Intracellular Polarity: Cell Junctions Microvilli Zonula occludens Zonula adherens Terminal web Macula adherens Gap junction Nucleus Hemidesmosome Mucous Membranes • Components of Mucous Membrane: 1. Epithelium 2. Basement membrane 3. Lamina propria Mucous Membrane Epithelium Basal lamina Lamina propria Serous Membranes A. Components of Serous Membrane: 1. Epithelium called mesothelium 2. Basement membrane 3. Submesothelial connective tissue layer 1. Protection from: Functions of Epithelia Mechanical trauma Dehydration Pathogens 2. Secretion of: Hormones, milk, sweat etc. Enzymes, HCl, glycoproteins, Mucous & serous products 3. Lubrication of: Contents of GI tract Fetus in birth canal Joints 4. 5. 6. 7. Filtration of wastes: (Urine) Absorption of food: (Aminoacids, Glucose, Fatty acids) Neuroepithelium: (Taste, Smell, Hearing) Reproduction: (Germ cells) Major Types of Epithelial Cells A. Epithelial Cells Specialized for Transport: 1. Ion-transporting cells (Kidney tubules, Gall bladder etc.) 2. Cells that transport by pinocytosis (Endothelial cells of blood capillaries B. Absorption: (Enterocytes, Proximal convoluted tubule cells) C. Secretion: 1. Protein-secreting cells (Acinar cells of pancreas, Hepatocytes) 2. Polypeptide-secreting cells (APUD cells) 3. Mucous cells (Goblet cells) 4. Serous cells (Acinar cells of pancreas & secretory cells of parotid salivary glands. 5. Steroid-secreting cells (Adrenal cortex, Leydig cells etc.) D. Contractile Epithelial Cells: (Myoepithelial cells of glands) GLANDS A. B. Exocrine & Endocrine Glands: Classification of Exocrine Glands: 1. By structure: a) Number of cells b) Duct system c) Secretory portion 2. By secretory product a) Mucous secretion b) Serous secretion c) Seromucous secretion 3. By mode of secretion a) Merocrine b) Apocrine c) Holocrine Unicellular Multicellular Simple tubular Coiled tubular Branched Simple branched Simple acinar Compound tubular Compound tubulo-alveolar Salivary Glands Mucous acini Serous acini Mode of Secretion Active transport Merocrine Apocrine Holocrine Endocrine Connective Tissue Fat Fat cells Tanden Fibroblasts Bone Osteocytes Connective Tissue • Is one of the 4 basic tissues of the body. • Structurally it is made up of cells and large amount of intercellular space containing extracellular matrix. • Matrix is the dominating component of this tissue. • It forms framework, connecting, supporting and packing tissue of the body. • It also plays a dynamic role in the development, growth and homeostasis of other tissue types. Connective Tissue Loose connective tissue Dense connective tissue Fibroblasts Extracellular matrix Epithelial tissue Mammary Glands Composition • Cells • Extracellular matrix Types of Cells in Loose Connective Tissue 1. Residents: Fibroblasts Macrophages Reticular cells Mesenchymal cells 2. Visitants: Mast cells Plasma cells Leukocytes Fat cells Melanocytes Loose Connective Tissue Macrophage Adipocyte Elastic fibers Capillary Neutrophil Plasma cell Mast cell Lymphocyte Fibroblast Collagen fibers Fibroblast (Ultrastructure) Nucleus Rough ER Collagen Extracellular matrix Collagen Producing Cells 1. 2. 3. 4. 5. Fibroblast-More than one type of collagen Chondroblast- Type II collagen Osteoblast-Type I Reticular cell- Type III Smooth muscle-Type I & III Extracellular Matrix • Extracellular matrix (Fibers & Ground substance) is synthesized and secreted mainly by the fibroblasts & the fibers are assembled in the extracellular space. • Fibers Prime function is support & plays strengthing role in • Ground substance Functions are 1. Acts as a molecular sieve & stops the spread of noxious substances 2. Plays very important role in cellular nutrition & waste removal 3. Plays a vital role in aging. Its amount diminishes with age and wrinkles start appearing. Fiberous Components Connective tissue fibers are long, slender protein polymers that are present in variable proportions in different types of connective tissue. In many cases the predominant fiber type is responsible for conferring specific properties on the tissue. • Collagen Fibers: • Elastic Fibers: • Reticular Fibers: Collagen Fibers Collagen Fibers: Most abundant protein in the body. Synthesis & assembly: Collagen typesType I- most abundant & occurs in loose and dense connective tissue & bone. Type II- occurs in cartilage. Type III- occurs in hematopoitic tissues. Type IV- occurs in basal laminae & does not form fibers or fibrils. Type V- in placental basement membranes & blood vessels. Type X- around hypertrophic, degenerating chondrocytes of the growth plate where bone formation is to occur. Synthesis of Collagen Collagen’s main amino acids Glycine (34%) Fibroblast Intracellular Extracellular Proline (12%) Hydroxyproline (10%) Procollagen (Triple-helical units) Procollagen peptidase Tropocollagen Collagen fibril Collagen fiber Ground Substance Proteoglycans: They are made up of a core protein to which glycosoaminoglycans (GAGs) are attached. GAGs are polysacharides that contain aminosugars. GAGs-Chondroitin sulphate, Dermatan sulphate, Keratan sulphate & Heparin sulphate. Hyaluronic acid is a GAG but do not form proteoglycans. Matrix viscosity and rigidity are determined by the amount and types of GAGs, their association with the core protein to form proteoglycans, GAG-fiber association, and GAG-GAG associations. Glycoproteins: Fibronectin-mediates the attachment of cells to the extracellular matrix. Laminin-a component of basal laminae that mediates the attachment of epithelial cells. Tissue fluids: Salts: Connective Tissue Types A. Connective Tissue Proper: 1. Loose connective tissue 2. Dense connective tissue a) Dense regular connective tissue b) Dense irregular connective tissue B. Reticular connective tissue: C. Elastic connective tissue: D. Mucous connective tissue: Connective Tissue Proper A. Connective Tissue Proper: 1. Loose connective tissue (lamina propria) 2. Dense connective tissue a) Dense regular connective tissue (Tendon, ligament) b) Dense irregular connective tissue (Dermis, organ capsule) Loose CT Dense CT Elastic Connective tissue Elastic fibers consist of an amorphous protein called elastin and numerous protein microfibrils embedded in it. Diameter range 0.1-10um. Elastic fibers are collected in thick, wavy, parallel bundles & seperated by loose collagenous tissue with fibroblasts. Ground substance is sparse. Elastic connective tissue provides flexible support. Predominates in the ligamentum flava of the vertebral column & the suspensory ligament of the penis. Reticular Connective Tissue These fibers look very similar to collagen but are thinner than them (0.1-1.5um). More highly glycosylated. Form delicate silver-staining network instead of thick bundles. Composed mainly of type III collagen and some glycoprotein. These fibers are covered by long processes of the reticular cells. There is very little ground substance. Reticular connective tissue supports motile cells & filters body fluids. It is found mainly in hematopoietic tissue (bone marrow, spleen and lymph nodes). Reticular Connective Tissue Reticular cell Nu Reticular fibers Reticular cells Lymphocyte Lymph Node Mesenchyme Mesenchyme is embryonic connective tissue. Its stellate and fusiform cells (mesenchymal cells) are derived from mesoderm. They give rise to all the connective tissue of of the body. These are multipotential cells and persist in adults to give rise to new generations of connective tissue cells especially during wound healing, bone repair and tissue fibrosis. Mesenchymal Tissue (Embryo) Neural tube Mesenchyme Somite Notochord Neural tube Extracellular matrix Mesenchymal cells Histophysiology A. Functions: 1. Support. 2. Defense. a) Physical b) Immunologic 3. Repair. 4. Storage. 5. Transport B. Edema: C. Hormonal Effects: D. Nutritional Factors: E. Collagen Renewal: Special Types of Connective Tissues • • • • Adipose tissue Blood & lymph Cartilage Bone Blood White Blood Cells (Granulocytes) Neutrophil Eosinophil Basophils Functions:Neutrophils act as first line of defense in infections. Eosinophils respond to allergic states & parasitic infection Basophils release heparin & histamine Defense System ADAPTIVE DEFENSES INNATE DEFENSES (Requires immunization) (Do not require immunization) Physical barriers (Skin, mucous membranes) Chemical barriers (Low pH, Mucous) Soluble factors (Lysosomes, Interferons, Acute phase proteins, Complements) Cytotoxic T lymphocytes Help B lymphocytes Facilitates CELLS (Macrophages, Granulocytes) Directly kill infected cells Facilitate ANTIBODIES Delayed response Fast response Limited Flexibility Non-specific No memory Highly flexible Highly specific Memory, lasting immunity Mast Cells Mast cells Functions:Produce heparin, an anticoagulant Produce histamine to render blood vessels permeable Monocytes Nucleus Cytoplasm RBC Nucleus Cytoplasm Phagocytized RBC Nucleus LYMPHOCYTES B Lymphocytes deliver antibodies-mediated immune response T lymphocytes deliver cell-mediated immune response Natural killer cells kill tumor & nonself cells Plasma Cells Plasma cells Lymphocyte Plasma cells produce antibodies to fight the infections Immunoglobulins IgG, IgA, IgM, IgE & IgD Macrophage Macrophage Functions:Phagocytose, process & present antigens to lymphocytes Act as scavengers etc. Unilocular Adipose Tissue Adipocytes Nucleus Multilocular Adipose Tissue Cartilage Perichondrium Chondroblasts Chondrocytes Lacuna Cartilage matrix Isogenous group of chondrocytes Primary Bone Periosteum Osteoblasts Osteocytes Bone matrix Bone trabecula Nervous Tissue Cerebellum Cortical neurons Spinal cord Motor neurons Spinal ganglion Sensory neurons Divisions of the Nervous System • Central Nervous System (CNS) • Peripheral Nervous System (PNS) • Autonomic Nervous System (ANS) Nervous System General Features • Two Classes of Cells: 1. Neurons 2. Supporting cells • Impulse Conduction: • Synapses: • Divisions of the Nervous System: • Embryonic Development of Nervous Tissue: • Aging and Repair: • Meninges: • Blood-Brain barrier: Cells of the Nervous Tissue Two Classes of Cells: 1. Neurons. 2. Supporting, neuroglial or glial cells. Neurons • • • • Cell Body Dendrites Axon Classification of Neurons Neuron Neuromuscular Junction Skeletal muscles Axon Motor end plate Neuron Blood capillary Glial cells Dendrites Nissl bodies Axon hillock Nucleus Nucleolus Myelinated axons • Neuron (Cell body) Cell Body: -It is also called soma or perikaryon -It is the synthetic & trophic center of cell -It can receive signals from axons of other neurons through synaptic contacts on its cell membrane and relay them to its axon -Nucleus usually large, central, spherical and euchromatic -Nucleus with prominent nucleolus -Cytoplasm contains many organelles like mitochondia, lysosomes etc. -Cytoplasm has abundant free polyribosomes & rough endoplasmic reticulum, appears as basophilic purplish-blue clumps called Nissl bodies -Well developed Golgi to pack & often glycosylates neurotransmitters in neurosecretory, or synaptic vesicles -Abundant neurotubules (microtubules) & neurofilaments (intermediate filaments) in soma, dendrites & axon Neuron (Dendrites) • Dendrites: -Extensions of cell body, specialized to increase the surface area for incoming signals -Synaptic contacts are made on them -Some synaptic sites on them look like sharp projections called dendritic spines gemmules -Proximal ends has some Nissl bodies • Axon: Neuron (Axon) -One axon per neuron, its cytoplasm called axoplasm & its plasma membrane, the axolemma. -A complex cell process (uniform diameter) carries impulses away from the soma. -The part of the cell body where axon exits the soma is called the axon hillock and it lacks Nissl bodies. -Axon can be myelinated or unmyelinated. -Myelin sheath in CNS is provided by the oligodendrocyte , while in PNS by the Schwann cell -Axon diameter & myelin thickness determines the speed of nerve impulse. Internode (Myelin –covered) & Node (without myelin) -Some axons have branches called collaterals. -Terminal branching of axon is called terminal arborization. -Each branch ends as a bulb-like sac called terminal bouton, each bouton contains many mitochondria & neurosecretory vesicles. Specialized region of plasma membrane of bouton that take part in the formation of synapse is called as presynaptic membrane. Nerve (Myelinated axons) Perineurium Endoneurium Nodes of Ranvier Axon Myelin Axon Myelinated Axon (E.M.) Neurilemma Myelin Axoplasm Node of Ranvier Synapses (Chemical) Synapses are specialized junctions by which a stimulus is transmitted from a neuron to its target cell. 1. Presynaptic Membrane: This is part of plasma membrane of terminal bouton. 2. Synaptic Cleft: Fluid-filled space between pre and post synaptic membranes. 3. Postsynaptic Membrane: This is part of plasma membrane of the target cell. It is thicker than presynaptic membrane due to the presence of receptors for neurotransmitters. When enough receptors are occupied, hydrophilic channels open, resulting in depolarization of the postsynaptic membrane. Neurontransmitter like acetylcholine that remains in the synaptic cleft is degraded by acetylcholinesterase. This removal of extra acetylcholine allows postsynaptic mambrane to reestablish its resting potential and prevents continuous firing of the postsynaptic neuron in response to a single stimulus. Types of Synapses • Axodendritic (Between an axon & a dendrite) • Axosomatic (Between an axon & a cell body) • Dendrodendritic (Between dendrites) • Axoaxonic (Between axons) Neuron (Types) • Based upon Configuration of cell processeses: Multipolar (Motor neurons of spinal cord) Bipolar (Retina, olfactry mucosa) Unipolar (Photoreceptors, rods & cones of retina) Pseudounipolar (Sensory neurons of dorsal root ganglia) • Based upon Cell size: Golgi type I (Motor neurons of spinal cord) Golgi type II (Interneurons of spinal cord) • Based upon Function Motor neurons (Multipolar neurons of ventral horn etc.) Sensory neurons (Pseudounipolar neurons of dorsal root ganglia) Interneurons (Golgi type II neurons) • Based upon Neurotransmitter released Cholinergic neurons (Most somatic motor neurons) Adrenergic & noradrenergic neurons (Postganglionic sympathatic neurons) Dopaminergic (Some neurons of hypothalamus) GABAergic (Some neurons of the brain) Types of Neurons Unipolar Bipolar Pseudounipolar Multipolar Supporting Cells • Provide structural and functional support to neurons. • Take part in the formation of blood-brain barrier, thus monitoring the passage of materials from blood to neurons. Supporting cells of CNS 1. Astrocytes:- (Blood-Brain Barrier) a) Protoplasmic astrocytes b) Fibrous astrocytes 2. Oligodendrocytes:- (Myelin to axons in CNS) 3. Ependymal cells:- (Produce the CSF) 4. Microglial cells:- (Macrophages of the nervous system) Supporting Cells of PNS 1. Schwann cells: A Schwann cell may envelop segments of several unmyelinated axons or provide a segment of a single myelinated axon with its myelin sheath. Each mylinated axon segment (internode) is wrapped around by layers of a Schwann cell process with most of its cytoplasm squeezed out. This multilayered Schwann cell plasma membrane (mainly of phospholipids) is called myelin. The gaps between myelin sheath segments are the nodes of Ranvier. 2. Satellite cells: Each neuron outside the CNS is surrounded by a single layer of cells, called satellite cells. Aging and Repair • A neuron is a terminally differentiated cell. • And is incapable of undergoing mitosis. • Aging neurons accumulate more of lipofuscin pigment. • Neurons lost through injury or surgery cannot be replaced. • If the cell body remains intact, the injured axon can regenerate itself. • If stimulated by injury, supporting cells, unlike neurons, can divide. Blood-Brain Barrier • Components of the barrier: 1. Endothelial cells of continuous type capillaries (Tight junctions) 2. Basal lamina 3. Cytoplasmic processes of astrocytes. Blood-brain Barrier Peripheral nerve Peripheral Nerve (Fascicle) Perineurium Endoneurium Myelinated axons Response of Nerve Tissue to Injury A. Damage to the Cell Body: A neuron is a terminally differentiated cell & is unable to divide. So damaged or dead neurons can’t be replaced. B. Damage to the Axon: 1. Degenaration:- Distal to the site of injury, axon & myelin degenerate. Within 2-3 days, they are removed & these clear endoneurial channels are occupied by Schwann cells. Proximal to the site of injury, retrograde degeneration of axon goes up to 2 internodes, then injured axon is sealed. Cell body also undergoes changes in response to the injury. The Nissl bodies disappear (chromatolysis) & nucleus moves to the periphery. (2 Weeks) 2. Regeneration:- Begins at 3rd week, Nissl bodies reappear, protein synthesis starts. Axon’s proximal stump gives off a number of small processes called neurites. One of these enters and grows in an endoneurial channel and synaptic contacts are remade with the target cell. The target cell or organ deprived of innervation often atrophy. Nerve Injury & Recovery A Cell body B C D E Nissl bodies Axon Schwann cells Motor end plate Muscle Before injury 2 weeks 3 weeks 3 months No healing Muscle Tissue Cardiac muscle Skeletal muscle Visceral muscle Basic Properties of Muscle Tissue 1. Excitability- ability to respond to a stimulus 2. Conductivity- ability to propagate a limited response 3. Contractility- ability to shorten 4. Relaxability- ability to relax (return to original shape after contraction) IC Disc Nucleus Cardiomyocyte in Longitudinal Section Endomysium Capillary Nucleus Myofibrils Cardiomyocyte Purkinje Cell In Cross Section Smooth Muscle Skeletal Muscle Cardiomyocyte (Long. Section) Endomysium Cardiomyocytes Nucleus Cardiomyocytes (Cross section) Cardiomyocytes Nucleus Myofibrils Endomysium Capillaries Comparison Of Types Of Muscles Property Location Skeletal Muscle Muscles of skeleton Heart Cell size/shape Long; cylindrical Nuclei Cardiac Muscle Smooth Muscle Visceral organs Short, branched Variable, fusiform Many; peripherally Single; centrally Single: central located located Striations Z lines Yes Yes T tubules & Sarcoplasmic reticulum Triads at A-I junctions Cell junctions None Yes N Yes Dense bodies Diads at Z line Caveolae replace T tubules; sparse Intercalated disks (Adherens, Nexi (Gapjunctions) occludens & nexi) EM of Cardiac muscle (IC disc) Macula adherens Gap junction Fascia adherens EM of Skeletal muscle