* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Adrenergic Transmission
Node of Ranvier wikipedia , lookup
Biochemical cascade wikipedia , lookup
Lipid signaling wikipedia , lookup
Proteolysis wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Paracrine signalling wikipedia , lookup
Vesicular monoamine transporter wikipedia , lookup
Western blot wikipedia , lookup
Signal transduction wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
SNARE (protein) wikipedia , lookup
History of catecholamine research wikipedia , lookup
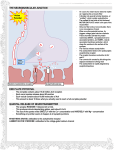
Saquiba Yesmine, PhD 1 Major Neurotransmitters in the Body Neurotransmitter Role in the Body Acetylcholine A neurotransmitter used by the spinal cord neurons to control muscles and by many neurons in the brain to regulate memory. In most instances, acetylcholine is excitatory. Dopamine The neurotransmitter that produces feelings of pleasure when released by the brain reward system. Dopamine has multiple functions depending on where in the brain it acts. It is usually inhibitory. GABA (gamma-aminobutyric acid) The major inhibitory neurotransmitter in the brain. Glutamate The most common excitatory neurotransmitter in the brain. Glycine A neurotransmitter used mainly by neurons in the spinal cord. It probably always acts as an inhibitory neurotransmitter. Norepinephrine Norepinephrine acts as a neurotransmitter and a hormone. In the peripheral nervous system, it is part of the flight-or-flight response. In the brain, it acts as a neurotransmitter regulating normal brain processes. Norepinephrine is usually excitatory, but is inhibitory in a few brain areas. Serotonin A neurotransmitter involved in many functions including mood, appetite, and sensory perception. In the spinal cord, serotonin is inhibitory in pain pathways. NIH Publication No. 00-4871 Cholinergic Transmission Adrenergic Transmission Cell Signaling and Synaptic Transmission Most cell-to-cell communication in the CNS involves chemical transmission. Chemical transmission requires several discreet specializations: • Transmitter synthesis. Small molecules like ACh and NE are synthesized in nerve terminals; peptides are synthesized in cell bodies and transported to nerve terminals. • Transmitter storage. Synaptic vesicles store transmitters, often in association with various proteins and frequently with ATP. • Transmitter release. Release of transmitter occurs by exocytosis. Depolarization results in an influx of Ca2+, which in turn appears to bind to proteins called synaptotagmins. An active zone is established to which vesicles dock and then fuse with scaffolding proteins on the presynaptic membrane. After fusing with the membrane and exocytotic release of their contents, synaptic vesicle proteins are recycled through endocytosis. Cell Signaling and Synaptic Transmission •Transmitter recognition. Receptors exist on postsynaptic cells, which recognize the transmitter. Binding of a neurotransmitter to its receptor initiates a signal transduction event, as previously described. •Termination of action. A variety of mechanisms terminate the action of synaptically released transmitter, including hydrolysis (for acetylcholine and peptides) and reuptake into neurons by specific transporters such as NET, SERT, and DAT (for NE, 5-HT, DA). Inhibitors of NET, SERT, and DAT increase the dwell time and thus the effect of those transmitters in the synaptic cleft. Inhibitors of the uptake of NE and/or 5-HT are used to treat depression and other behavioral disorders Cell Signaling and Synaptic Transmission A cholinergic neuroeffector junction showing features of the synthesis, storage, and release of acetylcholine (ACh) and receptors on which ACh acts. The synthesis of ACh in the varicosity depends on the uptake of choline viaa sodiumdependent carrier. This uptake can be blocked by hemicholinium. Choline and the acetyl moiety of acetyl coenzyme A, derived from mitochondria, form ACh, a process catalyzed by the enzyme choline acetyl transferase (ChAT). ACh is transported into the storage vesicle by another carrier that can be inhibited by vesamicol. ACh is stored in vesicles along with other potential cotransmitters (Co-T) such as ATP and VIP at certain neuroeffector junctions. Cell Signaling and Synaptic Transmission Release of ACh and the Co-T occurs on depolarization of the varicosity, which allows the entry of Ca2+ through voltagedependent Ca2+ channels. Elevated [Ca2+]in promotes fusion of the vesicular membrane with the cell membrane, and exocytosis of the transmitters occurs. This fusion process involves the interaction of specialized proteins associated with the vesicular membrane (VAMPs, vesicle-associated membrane proteins) and the membrane of the varicosity (SNAPs, synaptosome-associated proteins). The exocytotic release of ACh can be blocked by botulinum toxin. Once released, ACh can interact with the muscarinic receptors (M), which are GPCRs, or nicotinic receptors (N), which are ligandgated ion channels, to produce the characteristic response of the effector. ACh also can act on presynaptic mAChRs or nAChRs to modify its own release. Cholinergic Transmission Choline is transported into the presynaptic nerve terminal by a sodium-dependent carrier (A). This transport can be inhibited by hemicholinium drugs. ACh is transported into the storage vesicle by a second carrier (B) that can be inhibited by vesamicol. Release of transmitter occurs when voltage-sensitive calcium channels in the terminal membrane are opened, allowing an influx of calcium. The resulting increase in intracellular calcium causes fusion of vesicles with the surface membrane and exocytotic expulsion of ACh into the junctional cleft. This step is blocked by botulinum toxin. Acetylcholine's action is terminated by metabolism by the enzyme acetylcholinesterase. Receptors on the presynaptic nerve ending regulate transmitter release. Cholinergic Transmission The terminals of cholinergic neurons contain large numbers of small membrane-bound vesicles concentrated near the synaptic portion of the cell membrane as well as a smaller number of large dense-cored vesicles located farther from the synaptic membrane. The large vesicles contain a high concentration of peptide cotransmitters, while the smaller clear vesicles contain most of the acetylcholine. Vesicles are initially synthesized in the neuron soma and transported to the terminal. They may also be recycled several times within the terminal. Acetylcholine is synthesized in the cytoplasm from acetyl-CoA and choline through the catalytic action of the enzyme choline acetyltransferase (ChAT). Acetyl-CoA is synthesized in mitochondria, which are present in large numbers in the nerve ending. Choline is transported from the extracellular fluid into the neuron terminal by a sodiumdependent membrane carrier (carrier A). This carrier can be blocked by a group of drugs called hemicholiniums. Once synthesized, acetylcholine is transported from the cytoplasm into the vesicles by an antiporter that removes protons (carrier B). This transporter can be blocked by vesamicol. Acetylcholine synthesis is a rapid process capable of supporting a very high rate of transmitter release. Storage of acetylcholine is accomplished by the packaging of "quanta" of acetylcholine molecules (usually 1000–50,000 molecules in each vesicle). Continuation of Cholinergic Transmission Release of transmitter is dependent on extracellular calcium and occurs when an action potential reaches the terminal and triggers sufficient influx of calcium ions. The increased Ca2+ concentration "destabilizes" the storage vesicles by interacting with special proteins associated with the vesicular membrane. Fusion of the vesicular membranes with the terminal membrane occurs through the interaction of vesicular proteins (vesicleassociated membrane proteins, VAMPs), eg, synaptotagmin and synaptobrevin, with several proteins of the terminal membrane (synaptosomeassociated proteins, SNAPs), eg, SNAP-25 and syntaxin. Fusion of the membranes results in exocytotic expulsion of — in the case of somatic motor nerves—several hundred quanta of acetylcholine into the synaptic cleft. The amount of transmitter released by one depolarization of an autonomic postganglionic nerve terminal is probably smaller. In addition to acetylcholine, several cotransmitters will be released at the same time. The ACh vesicle release process is blocked by botulinum toxin through the enzymatic removal of two amino acids from one or more of the fusion proteins. Continuation of Cholinergic Transmission •The final step in the synthesis occurs within the cytoplasm, following which most of the ACh is sequestered within synaptic vesicles. • Moderately potent inhibitors of choline acetyltransferase exist, they have no therapeutic utility, because the uptake of choline is the rate-limiting step in ACh biosynthesis. Continuation of Cholinergic Transmission •After release from the presynaptic terminal, acetylcholine molecules may bind to and activate an acetylcholine receptor (cholinoceptor). Eventually (and usually very rapidly), all of the acetylcholine released will diffuse within range of an acetylcholinesterase (AChE) molecule. •AChE very efficiently splits acetylcholine into choline and acetate and terminates the action of the transmitter. Most cholinergic synapses are richly supplied with acetylcholinesterase; the halflife of acetylcholine in the synapse is therefore very short. Continuation of Cholinergic Transmission Two pools of acetylcholine appear to exist: - One pool, the "depot" or "readily releasable" pool, consists of vesicles located near the plasma membrane of the nerve terminals; these vesicles contain newly synthesized transmitter. Depolarization of the terminals causes these vesicles to release ACh rapidly or readily. - The other pool, the "reserve pool,“ replenish the readily releasable pool and may be required to sustain ACh release during periods of prolonged or intense nerve stimulation Adrenergic Transmission Adrenergic Transmission Adrenergic neurons transport a precursor molecule into the nerve ending, then synthesize the catecholamine transmitter, and finally store it in membrane bound vesicles. In most sympathetic postganglionic neurons, norepinephrine is the final product. In the adrenal medulla and certain areas of the brain, norepinephrine is further converted to epinephrine. Synthesis terminates with dopamine in the dopaminergic neurons of the central nervous system. Several important processes in these nerve terminals are potential sites of drug action. Adrenergic Transmission Adrenergic Transmission Tyrosine is transported into the noradrenergic ending by a sodium-dependent carrier (A). Tyrosine is converted to dopamine, which is transported into the vesicle by a carrier (B) that can be blocked by reserpine. The same carrier transports norepinephrine (NE) and several other amines into these granules. Dopamine is converted to NE in the vesicle by dopaminehydroxylase. Release of transmitter occurs when an action potential opens voltage-sensitive calcium channels and increases intracellular calcium. Fusion of vesicles with the surface membrane results in expulsion of norepinephrine, cotransmitters, and ATP Catecholeamines biosynthesis •The conversion of tyrosine to dopa, is the rate-limiting step in catecholamine transmitter synthesis. It can be inhibited by the tyrosine analog metyrosine. •A high-affinity carrier for catecholamines located in the wall of the storage vesicle can be inhibited by the reserpine alkaloids. • Another carrier transports norepinephrine and similar molecules into the cell cytoplasm (reuptake 1). It can be inhibited by cocaine and tricyclic antidepressant drugs, resulting in an increase of transmitter activity in the synaptic cleft. Continuation of Adrenergic Transmission In addition to the primary transmitter (norepinephrine), ATP, dopamine- -hydroxylase, and peptide cotransmitters are also released into the synaptic cleft. Indirectly acting sympathomimetics—eg, tyramine and amphetamines—are capable of releasing stored transmitter from noradrenergic nerve endings. These drugs are taken up into noradrenergic nerve endings by uptake 1. In the nerve ending, they may displace norepinephrine from storage vesicles, inhibit monoamine oxidase, and have other effects that result in increased norepinephrine activity in the synapse. Biosynthesis of catecholamines •The rate-limiting step, conversion of tyrosine to dopa, •It can be inhibited by metyrosine (amethyltyrosine). • TH deficiency has been reported in humans. • Characterized by generalized rigidity, hypokinesia, and low cerebrospinal fluid (CSF) levels of NE and DA metabolites homovanillic acid and 3-methoxy-4hydroxyphenylethylene glycol. •DβH deficiency in humans is characterized by orthostatic hypotension, ptosis of the eyelids, retrograde ejaculation, and elevated plasma levels of dopamine. •In the adrenal medulla, catecholamines are stored in chromaffin granules. These vesicles contain extremely high concentrations of catecholamines (21% dry weight), ascorbic acid, and ATP, as well as specific proteins such as chromogranins, The adrenal medulla has two distinct catecholaminecontaining cell types: a. those with NE and b. those with primarily epinephrine. The b cell population contains the enzyme phenylethanolamine-N-methyltransferase (PNMT). In these cells, the NE formed in the granules is methylated in the cytoplasm to epinephrine. Epinephrine then reenters the chromaffin granules, stored until released. In adults, epinephrine accounts for 80% of the catecholamines of the adrenal medulla, with NE making up most of the remainder. The adrenal medulla has two distinct catecholaminecontaining cell types: a. those with NE and b. those with primarily epinephrine. The b cell population contains the enzyme phenylethanolamine-N-methyltransferase (PNMT). In these cells, the NE formed in the granules is methylated in the cytoplasm to epinephrine. Epinephrine then reenters the chromaffin granules, stored until released. In adults, epinephrine accounts for 80% of the catecholamines of the adrenal medulla, with NE making up most of the remainder. •A major factor that controls the rate of synthesis of epinephrine, is the level of glucocorticoids secreted by the adrenal cortex. •The intra-adrenal portal vascular system carries the corticosteroids directly to the adrenal medullary chromaffin cells, where they induce the synthesis of PNMT. •The activities of both TH and DβH also are increased in the adrenal medulla when the secretion of glucocorticoids is stimulated. •Thus, any stress that persists sufficiently to evoke an enhanced secretion of corticotropin mobilizes and release epinephrine. Metabolism of catecholamines by catechol-Omethyltransferase (COMT) and monoamine oxidase (MAO). Norepinephrine and epinephrine metabolized by - MAO and COMT Termination of the Actions of Catecholamines The actions of NE and epinephrine are terminated by: - reuptake into nerve terminals by NET - dilution by diffusion out of the junctional cleft and uptake at extraneuronal sites by ENT, OCT 1, and OCT 2 Following uptake, catecholamines can be metabolized or re-stored in vesicles. Two enzymes – monoamine oxidase (MAO) and catechol-O-methyltransferase (COMT). Termination of the Actions of Catecholamines • The inhibitors of neuronal reuptake of catecholamines potentiate the effects of the neurotransmitter; e.g., cocaine and imipramine. • Inhibitors of MAO and COMT have relatively little effect. However, MAO metabolizes transmitter that is released within the nerve terminal. • COMT, particularly in the liver, plays a major role in the metabolism of endogenous circulating and administered catecholamines. Termination of the Actions of Catecholamines Adrenergic Transmission Nicotinic Ach Receptors