* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Function of prostaglandins
Human digestive system wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Signal transduction wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Butyric acid wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Biosynthesis wikipedia , lookup
Cryobiology wikipedia , lookup
12-Hydroxyeicosatetraenoic acid wikipedia , lookup
Epoxyeicosatrienoic acid wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
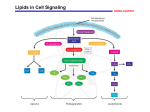
Lipid signaling wikipedia , lookup
15-Hydroxyeicosatetraenoic acid wikipedia , lookup
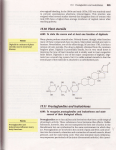
Membrane phospholipids and Inflammatory mediators MSS Module- Lecture 14 All of us know the famous drug “ASPIRIN” and why we use it But do you know how it works? It works by inhibiting an enzyme called cyclooxgenease (it is also called prostaglandin endoperoxide G/H synthetase). So, what is cyclooxygenase enzyme? It is an enzyme acting on a component of membrane phospholipids ( namely arachidonic acid) resulting in formation of biologically active compounds known as eicosanoids that include: prostaglandins (mainly PGE and PGFά) , prostacyclin (PGI) and thromboxanes (TX) . Many factors control the synthesis and secretion of different eicosanoids, for example: in pregnancy they are produced under the effect of oxytocin hormone, in the thermoregulatory center of the hypothalamus they are secreted by the effect of pyrogens. Corticotrophin releasing hormone stimulates their synthesis while glucocorticoids inhibit their synthesis. In the body, fatty acids, including arachidonic acid; a C20 polyunsaturated f.a.; are found incorporated in membrane phospholipids: phosphatidylcholine, phosphatidyl-ethanol-amine, phosphatidylinositol. Arachidonic acid is released from phospholipids in response to specific signals(compare to the formation of second messengers) One of the enzymes responsible of this release is phospholipase A2 whose activity is inhibited by lipocortin, annexins released under the influence of the glucocorticoids ( e.g. cortisol) Many stimuli (e.g. epinephrine, thrombin and bradykinin) activate phospholipase A2 The immediate dietary precursor of arachidonate is linoleic acid. Linoleic acid (arachidonate precursor) and ά- linolenic acid (eicosapentaenoate precursor) are essential fatty acids, so they must be taken in the diet otherwise the body can not synthesize the eicosanoids. Minor eicosanoids are eicosopentaenoic acid, e.g.TXA3 derived from All cells with the exception of RBCs can produce eicosanoids. All eicosanoids are locally active compounds and mediate their action through receptor-mediated Gprotein linked signaling pathways leading to an increase ( or sometimes a decrease) in cAMP levels. They differ from hormones in the following aspects: 1. They are produced in small amounts in almost all tissues rather than specialized glands. 2. They act locally rather than after transport to target tissues 3. They are not stored, have extremely short half life, and are metabolized rapidly to inactive products at their site of synthesis. 4. Their biological effects are mediated by plasma and nuclear membrane receptors, which are different in different organ systems. Biosynthesis of Eicosanoids. Two main pathways are involved in the biosynthesis of eicosanoids. The prostaglandins, prostacyclin, and thromboxanes are synthesized by the cyclic pathway involving the cyclooxygenases, while the leukotrienes are synthesized by the linear pathway involving lipoxygenases. Both types of enzymes are iron metalloenzymes. Cyclooxygenases (COX) Cyclooxygenases (COX) are called thus because they lead to the formation of a cyclopentanic cycle.They are also called PGH synthases because they lead to formation of prostaglandin H. There are two major different forms (isoenzymes) of cyclooxygenase; cyclooxygenase 1 (COX1) and cyclooxygenase 2 (COX2). The following table summarizes the characters of both of them: COX 1 COX 2 Continuously produced in gastric mucosa, kidney, platelets and vascular endothelial cells Inducible form (not present normally in the cells) and expressed mainly in macrophages and monocytes. Used for signaling pain and inflammation, and produces prostaglandins in inflammatory responses. Its production is stimulated by inflammatory cytokines (IL-1) and growth factors (e.g. PAF) Important for formation of prostaglandins required for normal physiological functions. It is important in many tissues such as stomach (production of mucous secretion and regulation of gastric acidity), and in the kidney for water regulation. Synthesis of prostaglandins prostacyclins and thromboxanes from arachidonic acid. Many stimuli (e.g. epinephrine, thrombin and bradykinin) activate phospholipase A2 which hydrolyzes arachidonic acid from membrane phospholipids, while corticosteroids inhibit it. Function of prostaglandins 1. 2. 3. Different prostaglandins have different (and sometimes opposite) functions depending on tissue location. Prostaglandins Increase cAMP in many endocrine glands; such as pituitary, thyroid and parathyroid; leading to increased hormone production by these glands. On other hand, they decrease formation of cAMP in some tissues such as: Adipose tissues leading to decreased lipolysis The stomach leading to decreased gastric HCL secretion, and The pancreas leading to decreased insulin secretion . Function of prostaglandins(continue) Some prostaglandins cause relaxation of smooth muscles; especially of bronchi and blood vessels( vasodilation lowers systemic arterial pressure); while others cause muscle contraction( stimulate uterine contraction, hence are used to induce labour) . Function of prostaglandins (continue) Some inhibit further release of neurotransmitters, after being released in response to their presence. Some are involved in the inflammatory response, causing oedema, swelling and prolonged erythema by increasing capillary permeability. Some have an effect on platelet aggregation. Some play a role in temperature control. Examples of clinically significant prostaglandins: 1-PGD2 secreted primarily from the mast cells and inhibits platelets aggregation and induces vasodilatation 2-PGE2 secreted by most cells especially the kidney,, the platelets and the heart, increases cAMP production, causes vasodilatation, and platelet aggregation. Used to induce uterine contraction and labour. 3-PGF2ά secreted by most cells, especially the lung, spleen, uterus and heart, causes vasoconstriction, broncho-constriction and smooth muscle contraction e.g. uterine contractions. Function of prostacyclins Prostacyclin(PGI2); produced and secreted primarily by vascular endothelial cells( especially heart) ; It increases cAMP in platelets, and inhibit platelets aggregation, It prevents platelets adherence to healthy blood vessels wall, and It also produces vasodilatation, hence lowers the blood pressure Thus, it impedes thrompogenesis Function of Thrompoxanes Thromboxanes: are produced and secreted primarily by the platelets They cause mobilization of intracellular calcium, vasoconstriction, and contraction of smooth muscles. They also decreases production of cAMP in platelets and cause platelets aggregation,thus promoting the formation of blood clots (thrombi) ( opposite effect to PGI. This limit formation to site of vascular injury) Examples of clinically important TXs: TXA2: secreted from platelets, induces platelets aggregation and vasoconstriction, hence increase BP. TXB2: secreted from platelets and induces vasoconstriction Function of Leukotrienes Leukotrienes produced by leukocytes, platelets, mast cells and heart and lung vascular tissues, are involved in the inflammatory responses such as erythema, oedema and hyperthermia. In skin they are responsible for the ‘weal and flare’ response seen in some allergic responses.Some could lead to fatal side effects of vaccinations,e.g. LTC4, LTD4, LTE4, are components of slow reacting substance of enaphylaxis (SRS-A), induce contraction of smooth muscles, vasoconstriction, bronchoconstriction, and increased vascular permeability. LTB4 increases chemotaxis of polymorphonuclear leukocytes, causes release of lysosomal enzymes, and adhesion of WBCs Prostaglandins, inflammation steroidal and non-steroidal anti-inflammatory drugs. Prostaglandins released by damaged cells and nearby macrophages, cause changes in adjacent cells that carry specific prostaglandin receptors in their membranes. The influence, which prostaglandins have, depends upon the type of tissue they are acting upon. Such action may be direct, or as a result of modifying the actions of other signaling molecules. One of their effects is to stimulate pain receptors (nociceptors). At the same time they intensify the effects of other chemical mediators such as histamine and bradykinin leading to vasodilatation and an increase in the permeability of capillaries supplying the damaged area, helping the migration of phagocytes from the blood through capillary walls into the damaged tissue. As a result of these changes, the blood supply to the area increases, the tissues swell, and pain occurs (signs of inflammation). To combat this their production must be stopped Synthesis of prostaglandins and thromboxanes from arachidonic acid. Many stimuli (e.g. epinephrine, thrombin and bradykinin) activate phospholipase A2 which hydrolyzes arachidonic acid from membrane phospholipids, while corticosteroids inhibit it. The corticosteroidal drugs e.g. cortisol, prednisolone, act to inhibit phospholipase A2, thereby inhibiting the release of arachidonate from membrane phospholipids and the subsequent synthesis of eicosinoids. They also inhibit COX-2 Thus, they have anti-pyretic and antiinflammatory action. However, they have many undesirable side effects because they prevent the synthesis of the eicosinoids needed for normal, healthy body functions. Another class, the non-steroidal antiinflammatory drugs (NSAIDs) ,all act upon the cyclooxygenase activity, inhibiting both COX-1 and COX-2. Examples include: ibuprofen, naproxen, indomethacin, phenylbutazone ( reversible inhibition), and aspirin (irreversible inhibition) Low-dose aspirin therapy is used to lower the risk of stroke and heart attacks by decreasing formation of thrombi. Because of the non selective inhibition of COX-1 activity in the gut , these drugs are associated with gastric ulcerations. Systemic inhibition of COX-1, with subsequent damage to the stomach and the kidneys ,and impaired clotting of blood, is the basis of aspirin’s toxicity. Therefore, Another group of drugs was developed with selective inhibition on COX2 only, e.g. Celebrex (celecoxib), Prexige (lumiracoxib) , Vioxx (rofecoxib) and Bextra (valdecoxib) They are designed to reduce pathologic inflammatory processes while maintaining the physiologic function of COX-1.