* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lecture 37
Point mutation wikipedia , lookup
Enzyme inhibitor wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Metalloprotein wikipedia , lookup
Proteolysis wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Oligonucleotide synthesis wikipedia , lookup
Lipid signaling wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Peptide synthesis wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Butyric acid wikipedia , lookup
Biochemistry wikipedia , lookup
Specialized pro-resolving mediators wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Biosynthesis wikipedia , lookup
Citric acid cycle wikipedia , lookup
Biosynthesis of doxorubicin wikipedia , lookup
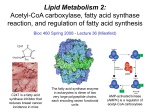
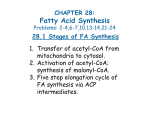
Lecture 37 Lipid Metabolism 2 Fatty Acid Synthesis Prostaglandins Key Concepts • Overview of fatty acid synthesis • Synthesis of palmitate from malonyl CoA • Regulation of fatty acid synthesis • Eicosanoids: Prostaglandin (PGH2) synthesis Overview of fatty acid synthesis Fatty acids are synthesized and degraded by different pathways. Difference FA Synthesis FA Degradation subcellular location cytosol mitochondrial matrix carrier protein acyl carrier protein (ACP) coenzyme A (CoA) enzymes all activities on a single multiple enzymes polypeptide chain required redox reductant is NADPH oxidants are NAD and FAD building block malonyl-CoA (formed by carboxylation of acetyl-CoA) Acetyl-CoA The commitment step in fatty acid synthesis is the carboxylation of acetyl-CoA to form malonyl-CoA by the enzyme acetyl-CoA carboxylase. Acetyl-CoA carboxylase uses a two-step mechanism that follows the ping-pong mechanism of substrate addition and product release. Two carbon units are sequentially added to the growing fatty acid chain by a large protein complex called fatty acid synthase. Palmitate (C16 ) is the end-product of the FA synthase reaction. The net reaction of palmitate synthesis is: 8 acetyl-CoA + 7 ATP + 14 NADPH + 14 H+ → palmitate + 14 NADP+ + 8 CoA + 7 ADP + 7 Pi + 6 H2O Note that excess acetyl-CoA units in the mitochondria are transported to the cytosol by the citrate shuttle. Moreover, an important component of this shuttle is the generation of NADPH in the cytosol which can be used for FA synthesis. This shuttle will produce 8 NADPH in the synthesis of palmitate since 8 acetyl-CoA units need to be transported. The synthesis of palmitate requires 14 NADPH as shown above in the net reaction. Where do the additional 6 NADPH come? Synthesis of palmitate from malonyl-CoA ATP-dependent caboxylation of acetyl-CoA by the enzyme acetyl-CoA carboxylase forms malonyl-CoA in the commitment step of the pathway. Subsequent decarboxylation of malonyl-CoA by fatty acid synthase results in the addition of C2 acetyl units to the growing fatty acid chain. Eight rounds are required to form palmitate. Note that the ATP-dependent carboxylation of acetyl CoA stores bond energy in malonyl CoA that is then used to drive fatty acid synthesis through the subsequent decarboxylation step. Indirectly, ATP hydrolysis therefore drives the fatty acid synthase reaction through the addition and removal of CO2. Malonyl CoA must be covalently attached to the acyl carrier protein (ACP) through a sulfhydral linkage at cysteine 163 prior to elongation: malonyl-CoA + ACP ↔ malonyl-ACP + CoA Once the enzyme is "primed" then the first synthesis step condenses C2 acetyl-ACP, with C3 malonylACP, and release of CO2: 1st round: C2 + C3 → CO2 + C4 2nd round: C4 + C3 → CO2 + C6. Reduction, dehydration and reduction steps then follow, regenerating an acyl-ACP that is ready for another cycle. The growing fatty acid chain is translocated between the condensing enzyme (CE) and acyl carrier protein (ACP). Putting it all together: Acetyl CoA Carboxylase Reactions: 7 acetyl-CoA + 7 CO2 + 7 ATP → 7 malonyl-CoA + 7 ADP + 7 Pi Fatty Acid Synthase Reactions: acetyl-CoA + 7 malonyl-CoA + 14 NADPH + 14 H+ → palmitate + 7 CO2 + 14 NADP+ + 8 CoA + 6 H2O The Combined Reactions 8 acetyl-CoA + 7 ATP + 14 NADPH + 14 H+ → palmitate + 14 NADP+ + 8 CoA + 7 ADP + 7 Pi + 6 H2O Regulation of fatty acid synthesis Fatty acid metabolism is stringently controlled to balance synthesis and degradation in response to physiological demands. Acetyl-CoA carboxylase activity is controlled by numerous signals. This reaction is the key commitment step in fatty acid synthesis (formation of malonylCoA). Two mechanisms control acetyl-CoA carboxylase activity phosphorylation and dephosphorylation allosteric control by citrate binding Just as we have seen before with glycogen phosphorylase, allosteric control can partially activate the inactive form. In this case, phosphorylated acetyl-CoA carboxylase can be allosterically activated by citrate binding. Note that dephosphorylated acetyl-CoA carboxylase is nearly fully active and not appreciably stimulated by citrate binding. Explain the metabolic logic of citrate activation of acetyl-CoA carboxylase. Does this take place in the mitochondrial matrix or the cytosol? Why does it make sense that glucagon and epinephrine inhibit the activity of acetyl-CoA carboxylase, whereas, insulin stimulates its activity? Eicosanoids: Prostaglandin (PGH2) synthesis Arachidonate is a C20 unsaturated fatty acid (four C=C bonds) that is the major precursor to a class of signaling molecules collectively called eicosanoids (eye-cose-anoids), which signifies the presence of 20 carbons from the Greek word "eikosi" which means twenty. Eicosanoids are considered local hormones because they activate signaling pathways in nearby cells and are short-lived molecules. Prostaglandins are a type of eicosanoids that stimulate the inflammatory response. Prostaglandin H2 (PGH2) is the product of the enzymatic reaction catalyzed by Prostaglandin Synthase. This enzyme functions as a cyclooxygenase and the two known isoforms are called COX-1 and COX-2. These enzymes are pharmacologic targets of non-steroidal antiinflammatory drugs (NSAIDs) such as aspirin and ibuprofen. Aspirin and ibuprofen inhibit the production of PGH2 by irreversibly blocking the cycloxygenase activity of prostaglandin synthase. It turns out that aspirin and ibuprogen inhibit both COX-1 and COX-2, although ibuprofen is more potent than aspirin. The COX-2 isoform is considered the key proinflammatory enzyme in many human pathophysiologies and was discovered by Donald Young, M.D., a University of Rochester biochemist. Alternatively, COX-1 is an important enzyme in the stomach that produces prostaglandins required for regulation of gastric mucin. Therefore, a major side effect of aspirin and ibuprofen is gastrointestinal bleeding due to low amounts of mucin which are required to protect the stomach against acids and pepsin. COX-1 is sometimes called the "good" isoform and COX-2 the "bad" isoform. COX-2 is responsible for pain and inflammation. COX-2 specific inhibitors such as Celebrex and Vioxx have been shown to very effective for the treatment of arthritis. However, they have also been associated with an increased risk of death from cardiovascular disease and are currently undergoing re-evaluation by the Federal Drug Administration (FDA). The selectivity of Cox-2 inhibitors is due to fact that they are larger than aspirin and ibuprofen, both of which inhibit both Cox-1 and Cox-2. Aspirin, also known as acetylsalicylate, is an acetylating agent that irreversibly inhibits both COX-1 and COX-2 by acetylating a serine residue in the active site of the enzyme. In contrast, drugs like Celbrex are large and can only bind tightly to Cox-2, thus avoiding the side effects associated with Cox-1 inhibition. Aspirin, in small doses, dose have as a beneficial role as a anticoagulator. This is because PGH2 is the precursor of thrombaxane A2 (TXA2), a potent aggregator of blood platelets. Small amounts of aspirin taken on a daily basis decrease TXA2 production by inhibiting PGH2 synthesis. Low doses of aspirin do not cause significant stomach bleeding. Do you know where aspirin was originally found? In a plant, the willow tree!