* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Nutrition Support
Evolution of metal ions in biological systems wikipedia , lookup
Metabolomics wikipedia , lookup
Citric acid cycle wikipedia , lookup
Proteolysis wikipedia , lookup
Biosynthesis wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Phosphorylation wikipedia , lookup
Blood sugar level wikipedia , lookup
Metabolic network modelling wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Pharmacometabolomics wikipedia , lookup
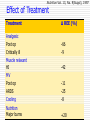
Determine Requirement for the Patients Pranithi Hongsprabhas MD. Division of Clinical Nutrition, Department of Medicine, Faculty of Medicine, KKU Objectives • Energy metabolism, normal protein, • carbohydrate and lipid metabolism Mechanisms that regulate substrate utilization and energy production • • • Metabolic responses to starvation and metabolic stress Effect of stress on metabolic rate and substrate utilization Determine calorie and protein requirements during metabolic stress • Methods for calculating nutritional requirements Energy Expenditure Basal energy expenditure~0.8-1.2 kcal/min Age Sex Body size (roughly with BSA): LBM Thermic effect of activity Thermic effect of food Metabolic stress BMR: shortly after awakening, fast 8-12 hr, thermoneutrally) RMR: Resting energy expenditure (fast 2 hr, rest 30 min, thermoneutrally) ~ 110%BEE Nutrients • • • • Protein Carbohydrates •enteral •parenteral Lipids Vitamins • • Water Minerals 4 kcal / g 4 kcal / g 3.4 kcal / g 9 kcal / g – Water soluble – Fat soluble – Electrolytes – Trace elements and ultra trace minerals Glucose Metabolism Glucose Glucose CYTOPLASM Cori Cycle MITOCHONDRIA Pyruvate Pyruvate Krebs Cycle ATP AcetylCoA Lactate Lactate Lieberman MA, Vester JW. Carbohydrates. In: Nutrition and Metabolism in the Surgical Patient. Boston, MA: Little, Brown and Company;1996:203-236. Fatty Acid Metabolism CAPILLARY Triglycerides CYTOPLASM Fatty Acids Carnitine MITOCHONDRIA Fatty Acids Fatty Acids + Glycerol ß Oxidation ATP Triglycerides Fischer JE, ed. Nutrition and metabolism in the surgical patient. Boston, MA: Little, Brown and Company; 1996. Amino Acids • Essential Leucine Lysine Valine Threonine Isoleucine Phenylalanine Methionine Histidine Tryptophan • Conditionally essential • Non-essential Glutamine Arginine Alanine Tyrosine Aspartic Acid Glutamic Acid Cysteine Glycine Serine Proline Fischer JE, ed. In: Nutrition and Metabolism in the Surgical Patient. 1st ed. Lippincott Williams and Wilkins Publishers; 1996. Nutrient Utilization • Regulation – Nutrient availability – Hormonal environment – Inflammatory state Metabolic Response to Fasting GLUCOSE UTILIZED (g/hora) I II III IV 40 V Exogenous Glycogen Gluconeogenesis 30 20 10 LEGEND I II III FUEL FOR BRAIN GLUCOSE GLUCOSE GLUCOSE IV GLUCOSE, KETONES V GLUCOSE, KETONES Ruderman NB. Annu Rev Med 1975;26:248 Body Response to Starvation: Early Stage Alanine / Pyruvate Glucose Glycerol Gluconeogenesis FAT Ketogenesis Glutamine Ketones AGL Ureagenesis Ketones Urea NH3 Body Response to Starvation: Late Stage Alanine / Pyruvate Glucose Glycerol Gluconeogenesis FAT Ketogenesis Glutamine Ketones AGL Ureagenesis Ketones Urea NH3 Metabolic Response to Starvation Hormonal Response Starvation Energy Expenditure in to Starvation Nitrogen Excretion (g/day) Hormone 12 Source Change in Secretion Norepinephrine Sympathetic Nervous System Norepinephrine8 Adrenal Gland Epinephrine Adrenal Gland Normal Range Thyroid Hormone Thyroid Gland (changes to T3 Partial Starvation 4 T4 peripherally) Total Starvation 0 10 20 Days 30 40 Long CL et al. JPEN 1979;3:452-456 Landberg L, et al. N Engl J Med 1978;298:1295. Metabolic Response to Trauma Flow Phase Energy Expenditure Ebb Phase Time Cutherbertson DP, et al. Adv Clin Chem 1969;12:1-55 Metabolic Response to Trauma Endocrine Response Fatty Deposits Fatty Acids Liver & Muscle (glycogen) Glucose Muscle (amino acids) Amino Acids Metabolic Response to Surgical Trauma Alanine / Pyruvate Glucose Glycerol Gluconeogenesis FAT Ketogenesis Glutamine Ketones AGL Ureagenesis Ketones Urea NH3 Metabolic Response to Trauma Nitrogen Excretion (g/day) 28 24 20 16 12 8 4 0 10 20 30 Days Long CL, et al. JPEN 1979;3:452-456 40 Glucose Metabolism During Starvation and Critical Illness Starvation Stress reaction Gluconeogenesis + +++ Glycolysis - +++ Glucose oxidation Glucose cycling - - - +++ Glucose oxidation decrease to 2-2.5 mg/kg/min (3-4 g/kg/d) Lipid Metabolism During Starvation and Critical Illness Starvation Stress reaction Peripheral lipolysis +++ ++ Lipid oxidation +++ + Fatty acid cycling - ++ Protein Metabolism During Starvation and Critical Illness Starvation Stress reaction Proteolysis - +++ Protein synthesis Amino acid oxidation - + - +++ AA should be increased up to 1.5-2 g/kg/d Calorie Distribution Shift in Catabolism NORMAL CATABOLIC 15% 30% Protein 25% 25% Fat Fat CHO Protein CHO 45% 60% REE in Critically Ill Patient 70 62 Hypermetabolic 60 Normal Metabolic 50 Inappropriate Hypometabolic 40 30 23 20 15 10 0 Hypermetabolic Normal Metabolic Crit Care Med 1990;18:1320 Inappropriate Hypometabolic Effect of Illness REE in Sepsis 200 161+22 REE (%) 175 155+14 Sepsis Sepsis syndrome Septic shock Recovery from septic 124+12 150 102+24 125 100 Sepsis Sepsis syndrome Septic shock Recovery from septic shock Chioléro Rมet al. Energy metabolism in sepsis and injury. Nutrition 1997; 13 (suppl): 45S-51S Stress Stratified According to Metabolic Criteria Stress level Urine N Plasma (g/d) lactate Plasma glucose (mM) (mg/dl) Insulin resistance VO2 2 (ml/min·m ) Low <10 <1.5 <150 No <140 Moderate 10-20 1.5-3 150-250 Some 140-180 high >20 >3 >250 yes >180 Cerra FB. Multiple organ failure syndrome. In: Bihari DJ, Cerra FB, eds.Multiple organ failure syndrome. Fullerton, California: Society of Critical Care Medicine, 1989:1-24 Effect of Treatment Treatment Catecholamine E NE DA DB Nutrition Vol. 13, No. 9(Suppl), 1997 ∆ REE (%) (septic shock) +15 +25 +4 +6 blocker burn Head injury -7 -6 Sedative Post op MV Barbiturate: head trauma -25-55 -32 Nutrition Vol. 13, No. 9(Suppl), 1997 Effect of Treatment Treatment ∆ REE (%) Analgesic Post op Critically ill -66 -9 Muscle relaxant HI MV Post op ARDS Cooling Nutrition Major burns -42 -11 -25 -8 +20 Measure Energy Expenditure 2500 Expected Measured 2000 1500 1000 Bakker JP et al. Gastroenterology 1984: 87: 53-9 Roulet M et al. Clin Nutr 1983; 2:97-105 McCall M et al. JPEN 2003;27: 27-35 HI nonparalysed Trauma HI paralysed Septic Ventilated 0 Sepsis Ventilated 500 Energy Expenditure in ICU Kcal/d Kcal/kg/d 1927 3257 25 47 Trauma wk1 2380 Trauma wk2 4123 31 59 Sepsis wk1 Sepsis wk2 Uehara M. et al CCM1999; 27:P1295-2 Stage of Diseases: Metabolism and Chronic Critical Illness EBB EBB FLOW FLOW SIRS/MODS SIRS/MODS TIME Chronic critical illness The development of chronic critical illness: decreased TIME burnout metabolism and endocrine Prolonged hypermetabolism: SIRS and MODS Determining Calorie Requirements • Indirect calorimetry • Harris-Benedict x stress factor x activity factor • 25-30 kcal/kg body weight/day Calculating Basal Energy Expenditure Harris-Benedict Equation – Variables: gender, weight (kg), height (cm), age(yr) Men: 66.47 + (13.75 x weight) + (5 x height) – (6.76 x age) Women: 655.1 + (9.56 x weight) + (1.85 x height) – (4.67 x age) Calorie requirement = BEE x activity factor x stress factor Metabolic Response to Starvation and Trauma: Nutritional Requirements Injury Minor surgery Long bone fracture Cancer Peritonitis/sepsis Severe infection/multiple trauma Multi-organ failure syndrome Burns Activity Confined to bed Out of bed Stress Factor 1.00 – 1.10 1.15 – 1.30 1.10 – 1.30 1.10 – 1.30 1.20 – 1.40 1.20 – 1.40 1.20 Factor – 2.00 Activity 1.2 1.3 Example: Energy requirements for patient with cancer in bed = BEE x 1.10 x 1.2 ADA: Manual Of Clinical Dietetics. 5th ed. Chicago: American Dietetic Association; 1996 Long CL, et al. JPEN 1979;3:452-456 Calorie Calculation “Rule of Thumb” Calorie requirement = 25 to 30 kcal/kg/day Macronutrients during Stress Carbohydrate • At least 100 g/day needed to prevent ketosis • Carbohydrate intake during stress should be between 30%-40% of total calories • Glucose intake should not exceed 5 mg/kg/min Barton RG. Nutr Clin Pract 1994;9:127-139 ASPEN Board of Directors. JPEN 2002; 26 Suppl 1:22SA Macronutrientes during Stress Fat • Provide 20%-35% of total calories • Maximum recommendation for intravenous lipid infusion: 1.0 -1.5 g/kg/day • Monitor triglyceride level to ensure adequate lipid clearance Barton RG. Nutr Clin Pract 1994;9:127-139 ASPEN Board of Directors. JPEN 2002;26 Suppl 1:22SA Determining Protein Requirements • • • • Body weight Age Type of protein Daily requirements: Healthy 0.8 to 1.0 g/kg/day Stressed state 1.0 to 2.0 g/kg/day depending on condition TUN Vs UUN In Critically Ill Patients Receiving NS TUN = UUN+2 (UUN<10) TUN = 1.1UUN+2 (UUN>10) TUN = UUN 0.85 Dickerson RN, et al JPEN 2004;28:S24 Vitamins Fat Soluble Vitamins Vitamin A Vitamin D Water Soluble Vitamins Folic Acid Pantothenic Acid Biotin Niacin Riboflavin – Vitamin E – Vitamin K – Thiamin – Vitamin B6 – Vitamin B12 – Vitamin C Key Vitamins and Minerals Vitamin A Vitamin C B Vitamins Pyridoxine Zinc Vitamin E Folic Acid, Iron, B12 Wound healing and tissue repair Collagen synthesis, wound healing Metabolism, carbohydrate utilization Essential for protein synthesis Wound healing, immune function, protein synthesis Antioxidant Required for synthesis and replacement of red blood cells Minerals Sodium Potassium Chloride Calcium Phosphorus Magnesium Zinc Copper Chromium Manganese Selenium Iodine Iron Summary • Metabolic response to starvation is an adaptive • • mechanism Nutritional requirements increase during metabolic stress Energy Substrate Utilization • Fasting state: • Depends on nutrient availability • In stress: • Depends on hormonal environment and inflammatory response Adverse Effect of Overfeeding Hepatic steatosis Excess VCO2 Hyperglycemia Hypo K, Mg, P Hypertriglyceridemia RES suppression Worsening gas exchannge Intensive Insulin Therapy in Critically Ill Patients Von den Bergh et al. NEJM 2001,345(19):1359 A study on all patients during 1 year in ICU and need of ventilation (n= 1548) Randomized to conventional treatment (n=783) or Intensive insulin treatment (n=765) conventional (Intensive: Blood glucose <110mg/dl; Conventional: Insulin if >215 mg/dl) Fed according to needs, EN, PN or combined Intensive Insulin Treatment… Van Den Berghe Et Al, NEJM 2001 In hospital survival % 100 96 Intensive treatment 92 P = 0.01 88 Conventional treatment 84 0 50 100 150 200 Days after admission 250 Effect of Caloric loading CHO Loading What should We feed the critically ill High energy intake Not required Not prevent catabolism Increased risk of complication Intolerance to feeding, PN If intolerance: Permissive underfeeding Adequate protein intake!!!! Jeejeebhoy KN. Nutrition in Clinical Practice 2004; 19: 477-480