* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Genetics 3 – Aneuploidies and Other Chromosome
Site-specific recombinase technology wikipedia , lookup
Birth defect wikipedia , lookup
Genomic library wikipedia , lookup
DNA supercoil wikipedia , lookup
Biology and sexual orientation wikipedia , lookup
Medical genetics wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Comparative genomic hybridization wikipedia , lookup
Segmental Duplication on the Human Y Chromosome wikipedia , lookup
Point mutation wikipedia , lookup
Hybrid (biology) wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
DiGeorge syndrome wikipedia , lookup
Designer baby wikipedia , lookup
Epigenetics of human development wikipedia , lookup
Cell-free fetal DNA wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Gene expression programming wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Genomic imprinting wikipedia , lookup
Microevolution wikipedia , lookup
Down syndrome wikipedia , lookup
Genome (book) wikipedia , lookup
Skewed X-inactivation wikipedia , lookup
Y chromosome wikipedia , lookup
X-inactivation wikipedia , lookup
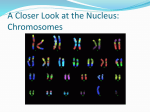
MCD - Genetics 3 - Aneuploidies and Other Chromosome Alterations Anil Chopra 1. Describe the normal karyotype, chromosome banding and nomenclature. In a normal karyotype, there will be 22 pairs of autosomal chromosomes and one pair of sex chromosomes (XX or XY) which makes up 46 chromosomes altogether (DIPLOID). In sex cells there are 23 chromosomes (HAPLOID). In order to identify chromosomes and genes on chromosomes, G (Giemsa) banding is used. Bands are labelled according to the chromosome number, then the arm (the p arm is the shorter one and the q arm is the longer one), and then the distance from the centromere: There are 3 main types of chromosome aberrations: • Structural – translocations, deletions, insertions, inversions, rings • Numerical – aneuploidy, loss or gain • Mosaicism – different cell lines Aberrations cause: - 60% of all early spontaneous miscarriages. - 4.5% of all still births (dead when born) - 7.5% of all conceptions, 0.6% of live births. 2. Draw a diagram of a balanced translocation and explain why these generally not deleterious? A balanced translocation occurs when two pieces of DNA from the chromosomes become exchanged. These do not normally cause any negative effect if any, because all the DNA of both chromosomes is present. They can however be associated with cancer if they occur in haploid cells. 3. Draw a diagram showing possible meiotic products from someone with a balanced translocation. or or or r normal balanced • • unbalanced d a balanced translocation may have an unbalanced set of Offspring from chromosomes (50%). Affected conceptions may miscarry, or be mentally retarded/multiple malformations if live-born. 4. Describe how 3 different chromosome aberrations lead to Down syndrome Aneuploidy • Monosomy - loss of a single chromosome is almost always lethal • Trisomy - gain of one chromosome can be tolerated • Tetrasomy - gain of two chromosomes can be tolerated Downs Syndrome • Overall incidence at birth is approx 1 in 650 to 1 in 700 • Strong association between incidence and advancing maternal age:20 years, 1 in 1500; 30 years, 1 in 900 40 years, 1 in 100; 45 years, 1 in 30 There are 3 possible causes for Down’s syndrome: 1) Trisomy 21: this is where there are 3 chromosome 21s. 95% of all Down’s cases 90% maternal origin of extra chromosome Non-disjunction (the failure of the chromosomes to properly segregate during meiotic or mitotic anaphase, resulting in daughter cells with abnormal numbers of chromosomes) in maternal meiosis I. The non-disjunction is most probably an ageing effect on the primary oocyte. This is caused by age-related reduction in immunological competence which allows survival of trisomic embryos Radiation Delayed fertilisation after ovulation 2) Translocation: this is where genetic material is moved around. 3% of all Down’s cases. Robertsonian – where the acrocentric chromosomes (13,14,15,21,22) break and their long arms fuse. (1:1000 incidence) 2/3 de novo translocation in child – i.e. random mutation in the children 1/3 of parents are carriers of translocation – i.e. mutations in the somatic cells (gametes) of the parents. If this is the case, the parents have a high risk of further Down’s babies. 13q21q (the q chains from chromosomes 14 and 21 have fused) and 14q21q - 10% risk of Down’s 21q21q - all offspring will have Down’s. 3) Mosaicism: this is where the actual fertilised egg cell, when it undergoes its first/second mitotic divisions, undergoes non-disjunction. 2% of all Down’s cases Children less severely affected Clinical Features of Down’s Syndrome • Newborn period - severe hypotonia (low muscle tone), sleepy, excess nuchal skin • Craniofacial - protruding tongue, small ears, epicanthic folds (also a feature of oriental and south Asians), upward sloping palpebral fissures, brushfield spots • Limbs - palmar crease, little finger extra short (short pinky), wide gap between 1st and 2nd toes • Cardiac - A and V septal defects • Other - short stature, duodenal atresia • IQ scores ranging from 25-75 • Most children are happy and affectionate • Relatively advanced social skills • Adult height around 150 cm • Cardiac anomaly causes early death in 20% • Usually develop Alzheimer’s in later life 5. Describe 2 common autosomal and 2 common sex chromosome aneuploidies. Trisomy 13 and 18 Trisomy 13 - Patau’s syndrome Trisomy 18 - Edward’s syndrome Usually causes death in 1st few weeks of life 1:5000-10,000 incidence Clinical features include bilateral cleft lip and palate. 90% cardiac abnormalities Cyclopia in some cases mental retardation if longer term survival 10% cases due to translocations/mosaicism Turner’s Syndrome • Has karyotype 45X. (one X chromosome missing) • 80% due to loss of X or Y chromosome in paternal meiosis. • Can also be due to ring chromosome, 1 arm deletion, mosaicism, isochromosome. • • • • • • • • 1 in 3000 live female births Patients have generalised oedema and swelling in neck region can be detected in 2nd trimester They can look normal at birth or have puffy extremities and intra-uterine oedema. Have low posterior hairline, short 4th metacarpals, webbed neck, aorta defect in 15% of cases Patients have normal intelligence. Will have short stature - 145 cm without growth hormone treatment. Have ovarian failure - primary amenorrhoea (never having periods) and infertility. Treated by oestrogen replacement for secondary sexual characteristics and prevention of osteoporosis XXX Females • 1:1000 have 47,XXX karyotype • 95% have extra maternal X arising in meiosis I • 10-20 point decrease in IQ • No physical abnormalities • Normal fertility • Offspring have normal karyotype • 48,XXXX and 49,XXXXX karyotypes show mental retardation Kleinfelter’s Syndrome – 47 XXY • 1 in 1000 male live births • X chromosome from either Male or Female • Clumsiness, mild verbal learning disability (verbal IQ reduced by 10-20 points) • Taller than average (long lower limbs) • 30% - moderately severe gynaecomastia (development of breasts) • All infertile • Increased risk of leg ulcers, osteoporosis and breast carcinoma in adult life • 48,XXXY and 49,XXXXY are rare XYY Males • 1 in 1000 in newborn males • Extra Y chromosome arises from non-disjunction in paternal meiosis II or as a post-zygotic event (mitotic error) • 2-3% institutionalised males who have mental retardation or antisocial criminal behaviour • Express emotional immaturity, impulsive behaviour • 10-20 point decrease in IQ, language delay. 6. Describe why sex determination is not solely based on sex chromosome karyotype The SRY Gene The gene that codes for phenotypically being male is the SRY gene which is situated at the end of the Y chromosome (hence anyone with a Y chromosome is male). It is activated at 6 weeks post conception and codes for the production of male testis. • XX males - Translocation of the SRY gene from Y chromosome to an X chromosome. Phenotypically male, testes develop, but sterile because some genes on Y chromosome need for spermatogenesis. • XY females - Mutations or deletions of SRY gene leads to female who is infertile