* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Unit II presentation
Genetic engineering wikipedia , lookup
Epigenetics of diabetes Type 2 wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Gene expression programming wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Genome (book) wikipedia , lookup
Oncogenomics wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Point mutation wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
Gene therapy wikipedia , lookup
Designer baby wikipedia , lookup
Microevolution wikipedia , lookup
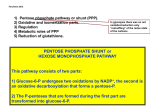
Unit II presentation Glucose -6-phosphate dehydrogenase deficiency Introduction • Most common human enzyme defect • Present in more than 400 million people world wide • Distribution similar to malaria • X linked ,hereditary genetic defect due to mutations in the G6PD gene • More than 140 mutations of the G6PD gene have been identified. • G6PD catalyzes the first reaction in the Pentose phosphate pathway[PPP] • Producing reduced form of nicotinamide adenine dinucleotide phosphate[NADPH] • NADPH enables cells to counterbalance oxidative stress and preserve the reduced form of glutathione • Red blood cells do not contain mitochondria • PPP is only source of NADPH • Defense against oxidative damage is dependant on G6PD Function of G6PD • Through action of G6PD and 6 phosphogluconate dehydrogenase the PPP provides reducing power in form of NADPH • NADPH serves as an electron donor for enzymatic reactions essential in biosynthetic pathways • Its production is crucial to protection of cells from oxidative stress • G6PD is also necessary to regenerate the reduced form of glutathione • Glutathione is essential for the reduction of hydrogen peroxide and oxygen radicals • Also for maintenance of Hg and other RBC proteins in the reduced state. Genetics • The inheritance is typically X linked • Males are hemizygous for the G6PD gene Normal gene expression G6PD deficient • Females ,who have two copies of the G6PD gene on each X chromosome Normal gene expression Heterozygous Homozygous[in populations with high frequency of G6PD] • Heterozygous females are genetic mosaics as a result of X chromosome inactivation. • The abnormal cells of a heterozygous female can be as deficient as for G6PD as those of a G6PD deficient male. • On average heterozygous females have less severe clinical manifestations than G6PD deficient males Epidemiology and malaria selection • Deficient G6PD alleles are world • Its estimated that at least 400 million people carry a mutation in the G6PD causing deficincy • Highest prevelance is in Africa,southern europe,middle east,southeast asia and the central and southern pacific islands • The worldwide distribution of malaria is remarkably similar to that of mutated G6PD alleles. • Ruwende and colleagues noted that G6PD A-allele is associated with a reduction in the risk of severe P falciparum,for female heterozygotes and male hemizygotes [46% and 58% respectively] • Others have shown that parasite growth is slowest in G6PD deficient cells. • Intracellular schizogenesis,rather than invasion is affected in G6PD deficient RBC s Oxidative injury to parasite • Luzzatto and co-workers showed that RBC s with normal G6PD activity taken from G6PD Aheterozygous females Had 2-80 times more parasite growth than G6PD deficient RBC s • G6PD deficient RBCs infected with parasites undergo phagocytosis at an earlier stage Diagnosis of G6PD deficiency • The definitive diagnosis of G6PD deficiency is based on the estimation of enzyme activity,by quantitative spectrophotometric analysis of the rate of NADPH production from NADP • Several screening test are available • False negative may occur when measuring enzyme activity during an episode of acute haemolysis or presence of a high reticulocyte count Level of activity higher in young erythrocytes Clinical manifestation • Fortunately,most individuals are asymptomatic throughout their life • Generally manifests as acute haemolysis after oxidative stress Drugs Infection Ingestion of fava beans • Also presents as neonatal jaundice anaemia Chronic non-spherocytic haemolytic anaemia • The precise mechanism by which increased sensitivity to oxidative damage leads to haemolysis is not fully known. • The sequence of events after an exogenous trigger factor is present is also unknown • Clinically characterised by Fatigue,back pain ,anaemia jaundice Increased unconjugated bilirubin Reticulocytosis,LDH are markers of the disorder Drug induced haemolytic anemia • Clinically detectable haemolysis and jaundice 24-72 hrs of drug dosing. • Dark urine due to haemoglobin is characteristic • Anaemia worsens until days 7-8 • After drug cessation ,Hg begin to recover 8-10 days after • Heinz bodies typical Infection induced haemolytic anaemia • Infection is a typical cause of haemolysis • Hepatitis viruses A and B, cytomegaloviruses,pneumonia and typhoid fever are notable causes • ARF is a potential complication of viral hepatitis and concomitant G6PD deficiency Acute tubular necrosis due to renal failure Tubular obstruction by Hg casts Favism • Clinical sequelae of fava bean ingestion • Originally more common in the mediterranean countries • Presents as acute haemolytic anaemia usually after24 hrs after the beans are ingested. • Haemoglobinuria is more • Anaemia is generally acute and severe leading to ARF Neonatal jaundice • Jaundice 1-4 days of age • Similar to physiological jaundice ,comes later than ABO incompatibility • More typical and severe in premature infants • Mechanism not fully understood • Haemolysis does not contribute as much as impaired bilirubin conjugation and clearance by liver Congenital non-spherocytic haemolytic anaemia • Variant of G6PD deficiency causing chronic haemolysis • Class 1 WHO • Patients typically severe neonatal jaundice, chronic anaemia worsened by oxidative stress requiring BT • Also reticulocytosis, gallstones,splenomegally. management • Most effective is to prevent haemolysis by avoiding oxidative stressors. • Fortunately,Acute haemolysis is usually short lived and does not require specific tx • Rare cases of acute haemolysis leads to severe anaemia requiring transfusion • Neonatal jaundice caused by G6PD deficiency is treated in the same way as other causes of NNJ. • May require phototherapy or blood transfusion • Patients with congenital non-spherocytic anaemia sometimes have a well compensated anaemia not requiring BT • However any exacerbating event can severely worsen the degree of anaemia • Rarely it may be BT dependant • Sometimes develop splenomegally but do not benefit from splenectomy. end