* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Mucosal immune system
Inflammation wikipedia , lookup
Monoclonal antibody wikipedia , lookup
DNA vaccination wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Molecular mimicry wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Adaptive immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Innate immune system wikipedia , lookup
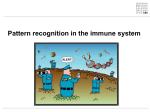
Immunosuppressive drug wikipedia , lookup
Immune system The main functions of the immune system Immune system belongs to the basic homeostatic mechanisms Defense - identification and protection against pathogenic microorganisms and their toxins Autotolerance – recognition of own tissues and keeping tolerance to them Immune surveillance - identifying and removing the old , damaged and otherwise changed cells Antigen (immunogen) * substance that the immune system recognizes and responds to it * usually proteins or polysaccharides (lipids and nucleic acids only in the combination with proteins or polysaccharides) * Molecules <5 kDa can´t trigger an immune response, the optimal size of the antigen molecules to initiate immune response is about 40 kDa * autoantigen - antigen derived from his own body * exoantigen - alien substance from the external environment allergen - exoantigen that in susceptible individuals may cause pathological (allergic) immune response Haptens * small molecules, that are able to induce specific immune response only after the establishment to the macromolecular carrier (separate haptens are not immunogenic) * typically drugs (eg penicillin antibiotics, hydralazin) Interaction antigen – antibody * Binding site of antibody (paratop) form non-covalent complexes with the corresponding part on antigen molecule (epitope) * participation: the hydrogen bonds, electrostatic and hydrophobic interactions, van der Waals forces * antigen-antibody complex is reversible Types of antigens according to antigen presentation 1) thymus dependent antigens * more frequently, mostly protein Ag * for specific humoral immune response to antigen is necessary to cooperate with TH lymphocytes (or response isn´t enough effective) * assistance implemented in the form of cytokines produced by TH lymphocytes Types of antigens according to antigen presentation 2) thymus independent antigens * in a small number of antigens can be induced antibodies production directly without the participation of T lymphocytes * this are mainly a bacterial polysaccharides, lipopolysaccharides and polymer forms of proteins (e.g. Haemophilus, Str.pneumoniae) Superantigens * proteins (microbial products) which have 2 binding sites, one interacts with the epitope presented on all MHCgpII, second interacts with other structures presented in many different TCR molecules (connection of T lymphocyte with APC) * stimulate polyclonaly and massively * massive activation of T lymphocytes can cause shock * e.g. bacterial toxins (Staph.aureus, Str.pyogenes, Pseud.aeruginosa) Differcence between antigen and superantigen binding Sequestered antigens * autoantigens that are normally hidden to the immune system and therefore unknow (e.g. the lens of the eye , testes) * if they are "uncovered" by demage, may take the immune system to respond (one of the theories of autoimmune processes) Components of the immune system Components of the immune system * Lymphoid tissues and organs * Cells of the immune systém * Molecules of the immune system Lymphoid tissues and organs * are linked with the other organs and tissues by network of lymphatic and blood vessels Primary lymphoid tissues and organs * bone marrow, thymus * place of maturation and differentiation of immunocompetent cells * immature lymphocytes acquire here their antigenic specificity Secondary lymphoid tissues and organs * meeting place of immunocompetent cells with Ag spleen - in contrast to the lymph nodes filter the blood and captures presented antigens lymph nodes and their organized clusters (tonsils, appendix, Peyer patches in the intestine) - filter lymph and capture present antigens MALT (mucous associated lymphoid tissue) - diffuse lymphatic tissue, the main role is capture of antigens that penetrate through the mucous membrane Cells of the immune system * evolution of red and white blood cells begin at yolk sack, then haematopoiesis travels to fetal liver and spleen (3 to 7 month gestation), the main hematopoietic function has bone marrow * all blood cells arise from a pluripotent stem cell (CD 34) * stem cells are modified and maintained throughout life * haematopoiesis is regulated by cytokines that are secreted by bone marrow stromal cells, activated TH cells and macrophages Surface molecules of leukocytes * antigen-specific receptors (TCR, BCR) * adhesion molecules (integrin, selectin, adhesion molecules Ig family) * Fc receptors * complement receptors * cytokine and chemokine receptors * MHC gp * receptors for components of microbial surfaces CD nomenclature * leukocyte surface molecules are called by CD-names (cluster of differentiation) * newly described molecules get the serial number * many of them have alternative names (CD14 - LPS receptor; CD16 - FcgRIII ...) * TCR, BCR and MHC gp have no CD title Molecules of the immune system * antigen-specific receptors (TCR, BCR) * antibodies * MHCgp I and II class (HLA) * Fc receptors * adhesion and costimulating molecules * cytokines and their receptors * non-specific receptors for components of microbial surfaces * complement system Immune mechanisms Immune mechanisms Nonspecific and specific immune mechanisms cooperate with each other. The first in defense usually apply nonspecific mechanisms that recognize the chemical structures present on the surface of many microorganisms (and absent in their own cells). Some types of phagocytes are essential for the initiation of antigen-specific mechanisms, because they work as APC (antigen presenting cells) for T lymphocytes. Tolerance Redundancy Nonspecific immune mechanisms * non-adaptive, innate * evolutionarily older * no immunological memory * in the presence of pathogens react quickly, in minutes (based on molecules and cells which are in the body prepared in advance) * component cellular - phagocytes (some are APC), NK cells humoral - complement, interferons, lectins and other serum proteins Natural non-immune protective mechanisms In protection the body against infection are important intact mucous membranes and skin and nonimmune protective mechanisms. mechanical – movement of cilia, air flow in the airways, or fluid flow in the urinary tract chemicals – fatty acids on skin; lysozyme in saliva, tears and sweat; antibacterial defensins, acid pH in stomach and urine microbial - non-pathogenic microflora Specific immune mechanisms * adaptive, antigen-specific * evolutionarily younger * have immunological memory * development of a full-specific immune response takes several days even weeks * component cellular - T lymphocytes (TCR) humoral - antibodies Specific immune mechanisms Clonal, anticipatory principle - the immune system is able to predict (anticipate) meeting with any Ag, so that it is prepared to advance a large number of T and B lymphocytes, which differ in their antigen-binding sites of specific receptors (TCR and BCR) and after contact with certain Ag multiply relevant cells and create clones of cells with the same specificity Principle of the second signal - for the full activation of lymphocytes is necessary costimulating signal, when it is not present, and lymphocyte reaches only the first signal (via the TCR, BCR), it leads to anergy or apoptosis Mucosal and skin immune system Function and structure of the mucosal and skin immune system Mucous membranes and skin are in constant contact with the outside environment, there is concentrated about 80% of immunocompetent cells. Skin - barrier against mechanical, physical and chemical damage, and against the penetration of microorganisms, humans surface of about 1,5 m2 Mucosal immune system - prevents the penetration of pathogenic microorganisms, preventing the development of self-harm inflammatory immune responses against pathogens and harmless antigens from the external environment, mucosa with an area of about 400 m2 Mucosal immune system Mucosa of mouth and nose, respiratory, gastrointestinal and urogenital system, mucous membrane of eye and inner ear, ducts of exocrine glands Natural non-immune defense mechanisms Movement of cilia, the flow of air and fluids, secrets of exocrine glands with bactericidal effects (fatty acids , lysozyme, pepsin, defensins, acidic pH of the stomach and urine) Structure of mucosal immune system MALT (mucous associated lymphoid tissue) BALT (bronchus associated lymphoid tissue) GALT (gut associated lymphoid tissue) o-MALT (organized) – consists from lymphoid follicles in the mucous membrane, tonsil and adenoids, appendix, Peyer patches d-MALT (diffuse) - is made up of leukocytes diffusely distributed in the lamina propria (T and B lymphocytes, macrophages, neutrophils, eosinophils and mast cells) Intraepithelial T lymphocytes * located predominantly in the villi of the small intestine * mostly have TCRgd a coreceptor CD8 * produce TGFb (mucosal healing) * suppression of adverse reactions to food allergens Humoral immune mechanisms of the mucous system sIgA *(secretory immunoglobulin A) * * * most significant mucosal immunoglobulin, in breast milk transcytosis - IgA is transported across the epithelium using transport Fc receptor (poly-Ig receptor), on luminal side is IgA split off with the part of the receptor called secretory component, which protects Ig against intestinal proteases neutralizing antigens on mucosal surfaces, don´t activate complement, binds to Fc receptors on phagocytes, in Peyerś patches may be immune complexes with IgA captured and can induce immune response sIgM * secretory immunoglobulin M * applied in newborns and in selective IgA deficiency * more prone to intestinal protease degradation * neutralizing antigens on mucosal surfaces IgG * get on the mucous membrane by diffusion * applies particularly in the lower airways Induction of mucosal immune response Oral tolerance * majority of antigens given orally causes suppression of specific immunity (critical is also the size of the antigenic particles) * Tr lymphocytes (regulatory) - production of IL-10 Induction of mucosal immune response * M cells - specialized enterocytes that provide transport of Ag (endocyte Ag from the surroundings) - are in close contact with lymphocytes and APC * mucosal immunization leads to stimulation of TH2 and TH3 lymphocytes and IgA production Immunological importance of the breastfeeding Breast milk contains: * sIgA, IgG (neutralization of infectious microorganisms, their products and potential allergens - before the full development of the newborn mucosal immune system) * CD 59 (protektin) - protect cells from the effects of complement * lysozyme, lactoferin, complement components, cytokines, including interferons * immunocompetent cells Skin immune system Epidermis * keratinocytes - secretion of cytokines (IL-1,6,TNF,IL-10,TGFb) - expression of MHCgpII → can serve as APC * Langerhans cells - skin dendritic cells (APC) * scattered intraepithelial lymphocytes * melanocytes Dermis * fibroblasts - collagen production - removal of apoptotic cells * mast cells * T lymphocytes (small amount) * vessels, hair follicles, sweat and sebaceous glands Immune mechanisms of inflammation (Local and systemic reactions) Inflammation * Is a summary of physiological responses to breach the integrity of the organism, leading to protection against infection of damaged sites, localization of damage and healing. * The first signals to the development of inflammatory responses come from mast cells, phagocytes, and the substances released from damaged cells and extracellular components of matter. Inflammation - acute (physiological defensive reactions, usually subside without consequences, damaged tissue heals completely) - chronic (usually already pathological reactions, occurs partial destruction of tissue and compensation with fibrous tissue) Response of the organism - local - system Local body's response to inflammation Manifestations - pain (dolor), heat (calor), redness (rubor), swelling (tumor) and loss of function (funkcio laesa) - increased permeability of blood vessels (vasoactive amines, complement components C3a, C5a, leukotrienes ..., swelling at site of inflammation) - increased expression of adhesion molecules on endothelia - activation of coagulation, fibrinolytic, kinin and complement system - influence of local nerve endings (prostaglandins, pain) - changes in temperature (IL-1, IL-6, TNF, prostaglandins) Systemic response to inflammation - depends on the extent of damage and duration of local inflammation - fever (proinflammatory cytokines TNF, IL-1, IFN g; stimulate hypothalamic center of thermoregulation) - mobilization of tissue metabolism - induction of expression of Hsp (heat-shock-proteins; function as chaperones) - production of acute phase proteins(CRP, SAP, C4, C5; opsonization and complement activation) - increased hepatic synthesis of certain serum transport proteins (ceruloplasmin, transferrin) - increased synthesis of protease inhibitors ( macroglobulin) - leukocytosis Septic shock - the massive penetration of microorganisms into the bloodstream ( TNF) Anaphylactic shock - basophil degranulation and complement activation with allergen Repair of damaged tissue - elimination of damaged cells with phagocytes - activation of fibroplastic mechanisms - activation of angiogenesis - regeneration and tissue remodeling Phagocytosis Phagocytosis = ability to absorb particles from the surroundings Professional phagocytes * cells, which provide defenses by mechanism of phagocytosis * neutrophilic and eosinophilic granulocytes, monocytes and macrophages granulocytes - a defense against extracellular pathogens - able to perform effector functions immediately - neutrophils don´t express MHCgpII (not APC) macrophages - the removal of own apoptotic cells, defense against certain intracellular parasites - fully functional after activating by cytokines (IFNg, TNF) The intersection of phagocytes in damaged and infected tissues 7% of peripheral neutrophils and phagocytes 93% neutrophils and phagocytes in the bone marrow * this ratio changes due to inflammatory cytokines and bacterial products * in place of damage are captured phagocytes to endothelium (due to inflammatory cytokine expression of adhesion molecules is higher) * the first is interaction between selectins (adhesion proteins of endothelial cells) and carbohydrate structures on the surface of neutrophils - called roling, which slows the movement of neutrophils * then there is a stronger link between ICAM-1 (endothelial cells) and leukocyte integrins (neutrophils) or VCAM-1 (endothelial cells) and b1-integrins (monocytes, eosinophils) and subsequent penetration between endothelial cells to the tissue - diapedesis , extravasation * phagocytes are directed to the site of inflammation by chemotactic active substances (IL-8, MIP-1 and b, MCP-1, RANTES, C3a, C5a, bacterial products ...), for which phagocytes have receptors * in tissue phagocytes move so that they secret the hydrolytic enzymes witch cleave components of intercellular substance Receptors of phagocytes PAMPs - "pathogen associated molecular patterns„ - structures that are located on the surface of microorganisms, but not on their own intact cells * mannose receptor * galactose receptor * CD14 (binds bacterial LPS) * receptors of TLR Group (binds bacterial lipoproteins, lipopolysaccharides, bacterial DNA) * scavenger receptors (bind phospholipids on the surface of apoptotic cells) Opsonization - process, which increases the efficiency of foreign particles phagocytosis - the establishment of opsonins (IgG, IgA, C3b, MBL, fibronectin, fibrinogen, CRP, SAP) on the surface of foreign particles * Fc receptors on phagocytes (recognize antibodies linked to surface of micro-organism) * complement receptors (for binding C3b) Liquidation of absorbed organism * fusion of fagosome with lysosomes lysosomes contains - bactericidal substances (defensins) - hydrolytic enzymes (cathepsin, lysozyme) - liquid with a pH of 4-5 * activation of membrane NADPH oxidase after activation of Fc receptors and complement receptors, which leads to respiratory (oxidative) flash, when arise reactive oxygen intermediates (superoxid radical O2-, singlet oxygen, hydrogen peroxide, hydroxyl radical), which damage the structure of biopolymers, enzymes and DNA of microorganisms; enzyme myeloperoxidase catalyses the reaction of H2O2 with Clto form chlornan anions (ClO-) * creation of nitric oxide (NO), which produces NO synthase of macrophages after activation with cytokines (IFNg, TNF) that are produced by TH1 lymphocytes, NO liquidate intracellular parasites of macrophages Secretory products of phagocytes * IL-1, 6, TNF (systemic response to inflammation) * IL-8 (chemokine) * IL-3, GM-CSF (control haematopoiesis) * TGF, TGFb (helping healing of tissues) * metabolic products of arachidonic acid (prostaglandins, prostacyclin, leukotrienes and thromboxanes Complement Complement * system of about 30 serum and membrane proteins (humoral component of nonspecific immunity) * complement components in serum are present in inactive form * complement activation has cascade character * complement proteins are synthesized in the liver, less by tissue macrophages and fibroblasts * the main complement components: C1-C9 (C3 is the central component) * other complement components: factor B, factor D, factor P * regulatory proteins: C1 - inhibitor, factor I, factor H, DAF, MCP, CR1, CD59 (protektin) inactivator of anafylatoxin Function of complement * Opsonization (C3b) * Chemotactic (C3a, C5a) * Osmotic lysis (MAC C5b-C9) * Anafylatoxins (C3a, C4a, C5a) Complement activation * Alternative pathway * Clasial pathway * Lektin pathway An alternative pathway * C3 component of complement rarely spontaneously break into C3b and C3a * C3b can covalently bind on the surface of a particle (own cell, microorganism) or reacts with water and inactivate * to bound C3b join a factor B, which is cleaved by factor D to Ba and Bb, resulting complex C3bBb is stabilized by factor P and functions as an alternative C3 convertase * C3 convertase cleaves C3 to C3a (chemotactic for phagocytes) and C3b, which binds to the surface of the particles (opsonization), or gives rise to other C3 convertases * from some C3 convertases form C3bBbC3b that act as an alternative C5 convertase, which cleaves C5 to C5a (chemotaxis) and C5b (starts terminal lytic phase) Classical pathway * Can be initiated by antibodies (IgG, not by IgG4; IgM) or so-called pentraxins (CRP, SAP - acute phase proteins) * after binding of antibodies to the bacteria surface, there is a change in its conformation and C1 protein can bind * C1 have to bind to the 2 molecules of antibodies, change their conformation and get proteolytic activity - will cleave proteins C4 and C2 * fragments C4b and C2a bind to the surface of organism and create the classic C3 convertase (C4bC2a), which cleaves C3 to C3a and C3b * then creates a classic C5 convertase (C4bC2aC3b) that cleaves C5 to C5a and C5b Lektin pathway * is initiated by serum mannose binding lectin (MBL) * MBL binds to carbohydrate structures on the surface of some microbes, after the bindins starts cleave C4 and C2 * this way is similar to the classical way Terminal (lytic) phase of the complement cascade C5b fragments creates a complex with C6, C7 and C8, the complex dive into the lipid membrane of the cell and attached to it into a circle 13-18 molecules of C9, thus create in the membrane pores and cell can lysis (G-bacteria, protozoans, some viruses). Most microorganisms is to this lytic effect of complement resistant (protection by cell wall). Regulation of complement and protection of own cells Activation of complement cascade is controlled by the plasma and membrane inhibitors. * C1 inhibitor * DAF (decay-accelerating protein)-degradation of C3 convertase * factor I, MCP (membrane cofactor protein), CR1, factor H – C3b cleavage * CD 59 (protectin) - prevents the polymerization of C9 * inactivator of anafylatoxin - inactivates anafylatoxins (C3a, C4a, C5a) Complement receptors * Bind fragments of complement components CR1 - on various cells - removing of immunecomplexes CR2 - on B lymphocytes and FDC - activation of B cells CR3, CR4 - on phagocytes - participation in opsonization, adhesion