* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Renal-CPC-17-y-old
Immune system wikipedia , lookup
Duffy antigen system wikipedia , lookup
Anti-nuclear antibody wikipedia , lookup
DNA vaccination wikipedia , lookup
Complement system wikipedia , lookup
Adaptive immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
Innate immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
X-linked severe combined immunodeficiency wikipedia , lookup
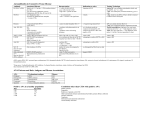
Renal CPC February 2009 ‘A 17 year old girl with chest pain and haemoptysis….’ Patient history • 17 y old girl admitted to hospital with a history of chest pain and haemoptysis • Previous history of mild asthma • Developed bi-pedal oedema 4 months previously • 3+ proteinuria in her urine, haematuria and hyperlipidaemia Patient history • Past and family history: – Mild intermittent asthma – Mother had MS and asthma and sickle cell trait – Siblings: sickle cell trait – Father had hypertension – Cousins had ?connective tissue disorder – One cousin on dialysis ?cause Patient history • Renal biopsy at that time [4 months previously] indicated membranous GN • Negative for antibodies to: – – – – – – – Hep B Hep C Anti-ribonuclear protein Anti-topoisomerase I, Anti-Ro [SS-A] Anti-double stranded DNA Anti-nuclear antibody Patient history • Levels of serum C3 and C4 complement were normal • Commenced on enalapril, atorvastatin and fluid restriction begun • Developed muscle cramps and pain and atorvastatin stopped • Persistent abdominal and back pain • US of the kidney: small peri-nephric haematoma Patient history • Over the next 2 months, continuing back pain with evidence of reduction of the peri-nephric haematoma • Treated with routine analgesics • Condition continued to deteriorate until she was unable to walk • Bilateral lower limb oedema occurred intermittently • 2 weeks before admission to hospital, the severity of the abdominal and back pain increased significantly, and also developed chest pain [radiating to the neck and shoulder area, made worse by coughing and deep inspiration] Patient history • 6 days before admission, a diagnosis on intercostal nerve ‘neuralgia’ was made • The chest pain continued to get more severe and cough and haemoptysis developed • She experienced one episode of significant dyspnoea which was relieved by the use of an albuterol inhaler • The day before admission to this hospital she attended the A&E room in another facility: – 390C, 115/69mmHg, HR 156, RR 50, O2 sats –98% [on room air], looked de-hyrdrated – Breathing shallow, lungs clear, other observations and clinical examination normal Patient history • She was given 2L of normal saline by the attending physician and pain relief • What investigations would you order on this patient? Patient history • O2 saturation dipped intermittently to 92-93% on room air • Urinalysis: – protein +3, blood +2, SG 1.041 • CXR: – Patchy density in the left costo-phrenic angle • ECG: – Tachycardia • Cardiac echcocardiography: – Right ventricular dilatation, pulmonary arterial pressure of 60mmHg and a small pericardial effusion. No clots were visible Patient history • Spiral CT scan and CT angiography of the chest were performed: – Emboli in both pulmonary arteries – Multiple bilateral pulmonary infracts – Bilateral pleural effusions • Renal ultrasound: – Haematoma around the left kidney • Doppler studies: – No clot in the deep veins of the leg, or the inferior vena cava • Heparin treatment commenced Patient history • Transferred to ICU • On admission to ICU: – – – – – – – – – 38.30C, HR 148, RR 34, O2 sat 92% Blood pressure increased Increased respiratory effort Prominent second heart sound JVP: increased to 7cm [at 30degree recline] Systolic murmur [grade 2/6], lower sternal border Right ventricular heave Tender abdomen 1+ oedema of both legs extending to above the knee Patient history • ECG: – S wave in lead I and Q and T waves in lead III Laboratory investigations Haemaglobin – normal HcT –normal WBCs – normal Diff – normal Platelets 497,000 [increased] MCV – normal PTT 70.3 [on heparin] PT 1.1 [normal] D-dimers –5,656 [increased] Glucose – normal Na+ – normal K+ – normal Cl- – normal Laboratory investigations BUN – normal Bilirubin –normal Protein: total – normal albumin – low Ca++ – normal CK – normal CK-MB – normal Alk phos – normal AST – normal ALT – normal C-reactive protein –22.6 [increased] Cardiac troponin – elevated Amylase – normal NT-pro-BNP 2571 [increased] Lipoprotein [increased] Laboratory investigations Lipase – normal Activated protein C screen – normal Functional protein S – normal Anticardiolipin IgG phospholipid units [GPL] – normal Anticardiolipin IgM phospholipid units [MPL] – normal Antithrombin III – normal Lupus anticoagulant – negative PT gene G201210A – not detected Antinuclear antibody 1:40 speckled Anti-double stranded DNA Ab titre – negative Anti-Ro [SS-A] antibody – negative Anti-smooth muscle antibody – negative Goodpasture’s antigen – negative ABGs: pH 7.51 pCO2 increased paO2 normal Urine total protein [mg/24 hrs] – 2690 (increased) Urine creatinine [g/24 hrs] 0.25 Cardiac echo: - panel A: flattening of the interventricular septum - pericardial effusion [black arrows] - panel B: enlarged right ventricle and a pericardial effusion [white arrow] Magnetic Resonance Venogram Small area of hypointense thrombus extending from the right renal vein into the inferior vena cava What is your differential diagnosis? • What would you do next? • What about anti-coagulation? • Will the low albumin level effect the use of heparin? • Should we use a direct thrombin inhibitor? • Should we transition to warfarin and what INR would you attempt to achieve? Summary of abnormalities • Proteinuria, haematuria, hyperlipdaemia [the nephrotic syndrome] • Pulmonary embolism [haemoptysis, chest pain and ECG changes] • Elevated cardiac troponins • Elevated pro-BNP • Elevated d-dimers on admission • Elevated platelet count • Variable hypertension • Anti-nuclear antibody • Membranous GN Causes of the nephrotic syndrome Proteinuria> 3.5 g of urinary protein:hypoalbuminaemia <3g/dl: oedema, hyperlipidaemia and lipiduria Differential diagnosis • Pulmonary embolism • Pulmonary embolism and features of the nephrotic syndrome • Pulmonary embolism and features of the nephrotic syndrome plus something else???? What test would you order now or would review any previous test? Renal biopsy appearances • Glomeruli: – normal or showed mild mesangial hyeprcellularity – granular staining of the BM with IgG • EM: – sub-epithelial deposits with effacement of the podocyte foot processes – mesangial and sub-endothelial deposits Diagnosis • Membranous GN – Primary – Secondary • Drugs, cancer, infection, autoimmune disease [most commonly SLE] Features suggestive of SLE in this case Treatment approaches • Improve proteinuria and treat hyperlipidaemia: – ACE inhibitors, statins • Add in immunosuppressive therapy: – If proteinuria persists A – minimal change B – membranous GN Features of SLE Immune response to self or foreign antigen Genetic deficiency in components of the innate immune system, such as complement component 1q (C1q), C4, serum amyloid protein, natural IgM or complement receptor 2 (CR2) leads to increased susceptibility to systemic lupus erythematosus (SLE). Two general hypotheses have been proposed to explain the genetic association with disease. a | The clearance hypothesis states that failure to clear apoptotic bodies — a principal source of SLE antigens — leads to inappropriate activation of mature, self-reactive B and T cells. Accordingly, apoptotic bodies are usually sequestered from the adaptive immune system by efficient recognition, binding and uptake by components of the innate immune system. So, SLE antigens are effectively 'hidden' from self-reactive lymphocytes. Defects in clearance of apoptotic bodies, such as those that occur in the absence of C1q or C4, would lead to the exposure of self-antigens to autoreactive lymphocytes and the development of SLE. b | The tolerance hypothesis states that innate immunity is important in the negative selection of selfreactive lymphocytes, especially B cells that are specific for SLE antigens. The innate immune pathway functions to recognize, degrade and bind SLE antigens to stromal cells present in the bone marrow and spleen. Immature B cells that encounter concentrations of cognate antigen above a certain threshold are negatively selected; that is, they undergo receptor editing, clonal deletion or anergy. C1q and C4 function to enhance 'presentation' of SLE antigens to specific immature B cells in the bone marrow. Alternatively, coupling of C4b to self-antigen could result in co-receptor stimulation of immature B cells displaying the CR1–CD19–CD81 co-receptor. The co-receptor is expressed at the surface of immature B cells during transitional stages in the spleen, in which co-ligation with the B-cell receptor could result in enhanced negative selection and 'escape' of self-reactive B cells into the peripheral mature compartment, where they encounter SLE antigens and become activated. Summary of the multiple factors that are known to contribute to abnormal lipid profiles in SLE Sandborg C et al. (2008) Therapy Insight: cardiovascular disease in pediatric /early adult systemic lupus erythematosus Nat Clin Pract Rheumatol doi:10.1038/ncprheum0789 Topics for revision • Pulmonary embolism – Risk factors – Investigation • The nephrotic syndrome – Causes of.. – Investigation of.. • Membranous GN