* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download B cell development & function PPT
Lymphopoiesis wikipedia , lookup
Adaptive immune system wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Innate immune system wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Molecular mimicry wikipedia , lookup
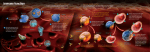
B Cells and B Cell Development © Dr. Colin R.A. Hewitt [email protected] The discovery of B cell immunity 1954 - Bruce Glick, Ohio State University Studies on the function of the bursa of Fabricius, a lymphoid organ in the cloacal region of the chicken Bursectomy – no apparent effect Bursectomised chickens were later used in experiments to raise antibodies to Salmonella antigens None of the bursectomised chickens made anti-Salmonella antibodies Bursa was later found to be the organ in which antibody producing cells developed – antibody producing cells were thereafter called B cells Mammals do not have a bursa of Fabricius Origin of B cells and organ of B cell maturation Transfer marked foetal liver cells Normal bone marrow Mature marked B cells in periphery No Mature B cells Defective bone marrow B cell development starts in the foetal liver After birth, development continues in the bone marrow B cell development in the bone marrow B Regulates construction of an antigen receptor B Ensures each cell has only one specificity B Checks and disposes of self-reactive B cells B Exports useful cells to the periphery B Provides a site for antibody production Bone Marrow provides a MATURATION & DIFFERENTIATION MICROENVIRONMENT for B cell development Bone Marrow S M M E Scheme of B Cell Development in the Bone Marrow Progenitors E n d o o s t e u m Stromal cells Pre-B X X X Macrophage Immature & mature B Central Sinus Bone marrow stromal cells nurture developing B cells 1. Specific cell-cell contacts between stromal cells and developing B cells 2. Secretion of cytokines by stromal cells Cell-cell contact B Secreted Factors - CYTOKINES Stromal cell Types of cytokines and cell-cell contacts needed at each stage of differentiation are different Maturing B cells Bone marrow stromal cell B B Stromal cell Stages of B cell development Stem Cell Early pro-B cell Late pro-B cell Large pre-B cell Peripheral Small pre-B cell Immature B cell Mature B cell Each stage of development is defined by rearrangements of IgH chain genes, IgL chain genes, expression of surface Ig, expression of adhesion molecules and cytokine receptors Cytokines and cell-cell contacts at each stage of differentiation are different VLA-4 Early pro-B Stem (Integrin) Receptor Tyrosine kinase Stem cell factor VCAM-1 (Ig superfamily) Cell adhesion molecules Kit Cell-bound growth factor Stromal cell Cytokines and cell-cell contacts at each stage of differentiation are different Interleukin-7 receptor Interleukin-7 Growth factor Early pro-B Late pro-B Stromal cell Pre-B Stages of differentiation in the bone marrow are defined by Ig gene rearrangement B CELL STAGE Stem cell Early pro-B IgH GENE CONFIGURATION Germline DH to JH Late pro-B Large pre-B VH to DHJH VHDHJH Pre-B cell receptor expressed Ig light chain gene has not yet rearranged Pre- B cell receptor Heavy chain VHDHJH Light chain VLJLCL VpreB CHm l5 Iga & Igb signal transduction molecules Transiently expressed when VHDHJH CHm is productively rearranged VpreB/l5 - the surrogate light chain, is required for surface expression Ligand for the pre-B cell receptor may be galectin 1, heparan sulphate, other pre-BCR or something as yet unknown Ligation of the pre-B cell receptor 1. Suppresses further H chain rearrangement 2. Triggers entry into cell cycle Large Pre-B Unconfirmed ligand of pre-B cell receptor 1. Ensures only one specificty of Ab expressed per cell Stromal cell 2. Expands only the pre-B cells with in frame VHDHJH joins ALLELIC EXCLUSION Expression of a gene on one chromosome prevents expression of the allele on the second chromosome Evidence for allelic exclusion ALLOTYPE- polymorphism in the C region of Ig – one allotype inherited from each parent Allotypes can be identified by staining B cell surface Ig with antibodies B a (Refer back to Dreyer & Bennet hypothesis in Molecular Genetics of Immunoglobulins lecture topic) B AND b b B B Y Suppression of H chain rearrangement by pre-B cell receptor prevents expression of two specificities of antibody per cell Y b Y B Y a a/b b/b Y Y a/a a Allelic exclusion prevents unwanted responses One Ag receptor per cell IF there were two Ag receptors per cell Y YY S. aureus Y Y Y Y Anti S. aureus Antibodies B S. aureus Anti brain Abs Y Y Y Y Self antigen expressed by e.g. brain cells YY B Anti S. aureus Antibodies Suppression of H chain gene rearrangement ensures only one specificity of Ab expressed per cell. Prevents induction of unwanted responses by pathogens Allelic exclusion is needed for efficient clonal selection Antibody S. typhi S. typhi All daughter cells must express the same Ig specificity otherwise the efficiency of the response would be compromised Suppression of H chain gene rearrangement helps prevent the emergence of new daughter specificities during proliferation after clonal selection Allelic exclusion is needed to prevent holes in the repertoire One specificity of Ag receptor per cell IF there were two specificities of Ag receptor per cell Anti-brain Ig Anti-brain Ig AND anti-S. aureus Ig B B Exclusion of anti-brain B cells i.e. self tolerance B Deletion OR B BUT anti S.aureus B cells will be excluded leaving a “hole in the repertoire” Anergy B S. aureus Ligation of the pre-B cell receptor 1. Suppresses further H chain rearrangement 2. Triggers entry into cell cycle Large Pre-B Unconfirmed ligand of pre-B cell receptor 1. Ensures only one specificity of Ab expressed per cell Stromal cell 2. Expands only the pre-B cells with in frame VHDHJH joins Large pre-B cells need in frame VHDHJH joins to mature Human IgG3 Heavy Chain nucleotide sequence Translation in frame 1 ATGAAACANCTGTGGTTCTTCCTTCTCCTGG TGGCAGCTCCCAGATGGGTCCTGTCCCAGG TGCACCTGCAGGAGTCGGGCCCAGGACTGG GGAAGCCTCCAGAGCTCAAAACCCCACTTGG TGACACAACTCACACATGCCCACGGTGCCCA GAGCCCAAATCTTGTGACACACCTCCCCCGT GCCCACGGTGCCCAGAGCCCAAATCTTGTG ACACACCTCCCCCATGCCCACGGTGCCCAG AGCCCAAATCTTGTGACACACCTCCCCCGTG CCCNNNGTGCCCAGCACCTGAACTCTTGGG AGGACCGTCAGTCTTCCTCTTCCCCCCAAAA CCCAAGGATACCCTTATGATTTCCCGGACCC CTGAGGTCACGTGCGTGGTGGTGGACGTGA GCCACGAAGACCCNNNNGTCCAGTTCAAGT GGTACGTGGACGGCGTGGAGGTGCATAATG CCAAGACAAAGCTGCGGGAGGAGCAGTACA ACAGCACGTTCCGTGTGGTCAGCGTCCTCAC CGTCCTGCACCAGGACTGGCTGAACGGCAA GGAGTACAAGTGCAAGGTCTCCAACAAAGCC CTCCCAGCCCCCATCGAGAAAACCATCTCCA AAGCCAAAGGACAGCCCGAGGAGATGACCA AGAACCAAGTCAGCCTGACCTGCCTGGTCAA AGGCTTCTACCCCAGCGACATCGCCGTGGA GTGGGAGAGCAATGGGCAGCCGGAGAACAA CTACAACACCACGCCTCCCATGCTGGACTCC GACGGCTCCTTCTTCCTCTACAGCAAGCTCA CCGTGGACAAGAGCAGGTGGCAGCAGGGGA ACATCTTCTCATGCTCCGTGATGCATGAGGC TCTGCACAACCGCTACACGCAGAAGAGCCTC TCCCTGTCTCCGGGTAAATGA MKXLWFFLLLVAAPRWVLSQV HLQESGPGLGKPPELKTPLGD TTHTCPRCPEPKSCDTPPPCP RCPEPKSCDTPPPCPRCPEPK SCDTPPPCXXCPAPELLGGPS VFLFPPKPKDTLMISRTPEVTC VVVDVSHEDXXVQFKWYVDG VEVHNAKTKLREEQYNSTFRV VSVLTVLHQDWLNGKEYKCKV SNKALPAPIEKTISKAKGQPEE MTKNQVSLTCLVKGFYPSDIAV EWESNGQPENNYNTTPPMLD SDGSFFLYSKLTVDKSRWQQG NIFSCSVMHEALHNRYTQKSLS LSPGK* Translation in frame 2 (no protein) Development continues Large pre-B Pre-B cell receptor can be activated Development arrests * Translation in frame 3 ETXVVLPSPGGSSQMGPVPGA PAGVGPRTGEASRAQNPTW* Development arrests Ligation of the pre-B cell receptor triggers entry into the cell cycle Proliferation Large Pre-B Large Large Pre-B Large Pre-B Large Pre-B Pre-B Small Large pre-B Proliferation stops Pre-receptor not displayed Many large pre-B cells with identical pre-B receptors IgM Intracellular VDJCH chain VL-JL rearranges Y Large pre-B Large Pre-B Large Large Pre-B Large Pre-B Large Pre-B Pre-B Immature B cell Light chain expressed IgM displayed on surface Heavy and light chain rearrangement is potentially wasteful V D J C Germline V D D J C DH-JH joining C VH-DHJH joining V V D J Large pre-B With two “random” joins to generate a heavy chain there is a 1:9 chance of a rearrangement of being in frame V J C Germline V V J C VL-JL joining With one “random” join to generate a light chain there is a 1:3 chance of a rearrangement being of frame Small pre-B There is, therefore, only a 1:27 chance of an in frame rearrangement Out of frame rearrangements arrest further B cell maturation B cells have several chances to successfully rearrange Ig genes Early Pro B DH-JH On first chromosome NO DH-JH On second chromosome Late Pro B YES YES VH-DJH On first chromosome NO VH-DJH On second chromosome Pre B YES k on first YES chromosome Y B YES l on first chromosome IgMl k on second chromosome NO NO NO NO B IgMk YES NO YES Immature B l on second chromosome NO YES Y B Acquisition of antigen specificity creates a need to check for recognition of self antigens Y Small pre-B cell B Y B Y Y Immature B cell No antigen receptor at cell surface Cell surface Ig expressed Unable to sense Ag environment Able to sense Ag environment !!May be self-reactive!! Can now be checked for self-reactivity 1. Physical removal from the repertoire 2. Paralysis of function 3. Alteration of specificity DELETION ANERGY RECEPTOR EDITING B cell self tolerance: clonal deletion Small pre-B B B Immature B B YY Small pre-B cell assembles Ig Immature B cell recognises MULTIVALENT self Ag Clonal deletion by apoptosis B cell self tolerance: anergy IgD normal IgM low Small pre-B B YY Immature B B IgM IgD B IgD IgD B Small pre-B cell assembles Ig Immature B cell recognises soluble self Ag No cross-linking Anergic B cell Receptor editing A rearrangement encoding a self specific receptor can be replaced V V V B V D J C !!Receptor recognises self antigen!! Arrest development And reactivate RAG-1 and RAG-2 V B V V B D J Apoptosis or anergy C Edited receptor now recognises a different antigen and can be rechecked for specificity B cell self tolerance: export of self tolerant B cells Small pre-B B YY Immature B B IgD and IgM normal IgD IgM IgM IgD B IgD IgM IgM IgD Small pre-B cell assembles Ig Immature B cell doesn’t recognise any self Ag Mature B cell exported to the periphery How can B cells express IgM and IgD simultaneously? Cm Cd Cg3 Cg1 Ca1 Cg2 Cg4 Cd Ce Cd Ca2 Sg3 Cg3 Cg3 Cm Sg1 Cm Cg1 VDJ Cg3 VDJ Ca1 VDJ Ca1 VDJ Cg3 VDJ Ca1 VDJ Ca1 IgG3 produced. Switch from IgM IgA1 produced. Switch from IgG3 IgA1 produced. Switch from IgM N.B. Remember Molecular Genetics of Immunoglobulins lecture – No Cd switch region Consider similarities with mechanism allowing secreted and membrane Ig by the same cell Splicing of IgM and IgD RNA VD J VD J Cm1 Cm2 Cm Cm3 Cd Cg3 Cd1 Cm4 Cg1 Cd2 DNA Cd3 pA2 pA1 Two types of mRNA can be made simultaneously in the cell by differential usage of alternative polyadenylation sites and splicing of the RNA VD J Cm1 Cm2 Cm3 Cm4 AAA Cd1 V D J Cm Cd2 Cd3 RNA cleaved and polyadenylated at pA1 IgM mRNA RNA cleaved and polyadenylated at pA2 VD J Cm1 Cm2 Cm3 Cm4 Cd1 Cd2 Cd3 pA1 V D J Cd IgD mRNA AAA Summary • B cells develop in the foetal liver and adult bone marrow • Stages of B cell differentiation are defined by Ig gene rearrangement • Pre-B cell receptor ligation is essential for B cell development • Allelic exclusion is essential to the clonal nature of immunity • B cells have several opportunities to rearrange their antigen receptors • IgM and IgD can be expressed simultaneously due to differential RNA splicing • So far, mostly about B cells in the bone marrow - what about mature peripheral B cells? What are the external signals that activate B cells? Fab anti-mIg mIg (Fab)2 anti-mIg Anti-(Fab)2 Although Fab fragments bind to membrane Ig (mIg), no signal is transduced through the B cell membrane Bridging (or ‘Cross-linking’) of different mIg allows the B cell receptor to transduce a weak signal through the B cell membrane Extensive cross linking of (Fab)2 bound to mIg using an anti-(Fab)2 antibody enhances the signal through the B cell membrane Ring staining Patching Ig is evenly distributed around the cell surface Ig is aggregated in uneven ‘clumps’ as a result of mild cross-linking of Ig Capping Ig is collected at a pole of the cell in a ‘cap’ as a result of extensive cross-linking of Ig Transduction of signals by the B cell receptor Extracellular antigen recognition domains Igb Iga The cytoplasmic domains of the Iga and Igb contain Immunoreceptor Tyrosine based Activation Motifs (ITAMS) - 2 tyrosine residues separated by 9-12 amino acids - YXX[L/V]X6-9YXX[L/V] Intracytoplasmic signalling domains Phosphorylation by Src kinases Kinase domain Enzyme domain phosphorylates tyrosines (to give phosphotyrosine) SH2 domain SH3 domain Unique region Phosphotyrosine receptor domain Adaptor protein recruitment domain ITAM binding domain • Phosphorylation changes the properties of a protein by changing its conformation • Changes in conformation may activate or inhibit a biochemical activity or create a binding site for other proteins • Phosphorylation is rapid, requires no protein synthesis or degradation to change the biochemical activity of a target protein • It is reversible via the action of phosphatases that remove phosphate Regulation of Src kinases Kinase domain Inhibitory tyrosine residue SH2 domain SH3 domain Unique region Activating tyrosine residue Phosphorylation of ‘Activating Tyrosine’ stimulates kinase activity Kinase domain SH2 domain SH3 domain Unique region Phosphorylation of ‘Inhibitory Tyrosine’ inhibits kinase activity by blocking access to the Activating Tyrosine Residue Regulation of Src kinases by Csk and CD45 C terminus Kinase domain SH2 domain SH3 domain Unique region Activated cells: a phosphatase associated with the Leukocyte Common Antigen - CD45, removes the C terminus phosphate allowing the activating tyrosine to be phosphorylated Resting cells: Src kinase is inactivated by a constitutively expressed C terminal Src kinase (Csk) Kinase domain Kinase domain SH2 domain SH3 domain Unique region The balance between Csk and CD45 phosphatase activity sets the threshold for initiating receptor signalling Phosphorylation of ITAMs by Src kinases ITAM ITAM ITAM P ITAM P ITAM P P P 1. Csk inactived Src interacts with low affinity with the ITAMs of ‘resting’ receptors 2. Antigen clusters B cell receptors with CD45 phosphatases. Src kinases are phosphorylated and are activated to phosphorylate ITAMS 3. Src kinases bind to phosphorylated ITAMS and are activated to phosphorylate adjacent ITAMS Syk protein Tyrosine kinases • CD45 phosphatase allows activation of Src family kinases Blk, Fyn & Lyn • Receptor cross-linking activates Src kinases that phosphorylate ITAMs in the Iga and Igb ITAM P P Syk - 2 x SH2 domains spaced to bind to two phosphotyrosines on an ITAM ITAM P P P P P ITAM P One Syk binds to Iga, one to Igb - each Syk transphosphorylates the other The B cell co-receptor CD21 (C3d receptor) CD45 CD19 Igb Iga CD81 (TAPA-1) The B cell co-receptor Co-receptor phosphorylation C3d opsonised bacterium C3d binds to CD21, the complement receptor 2 (CR2) Antigen recognition P P P P Src family kinases then bind the phosphorylated CD19 • mIg and CD21 are cross-linked by antigen that has activated complement • CD21 is phosphorylated and receptor-associated kinases phosphorylate CD19 • Phosphorylated CD19 activates more Src family kinases • Ligation of the co-receptor increases B cell receptor signalling 1000 -10,000 fold Activation of signals that affect gene transcription BLNK P P P P Tec Tec Tec Tec Cell membrane-associated B cell Linker protein - BLNK contains many Tyrosine residues BLNK binds Tec kinases ITAM P P P P P ITAM P Activated Syk phosphorylates BLNK Activated Syk phosphorylates Guanine-nucleotide exchange factors (GEFS) that in turn activate small GTP binding proteins Ras and Rac Tec kinases activate phospholipase C- g (PLC-g) PLC-g cleaves phosphotidylinositol bisphosphate (PIP2) to yield diacylglycerol (DAG) and inositol trisphosphate (IP3) Ras and Rac activate the MAP kinase cascade Transmission of signals from the cell surface to the nucleus • B cell-specific parts of the signalling cascade are associated with receptors unique to B cells - mIg, CD19 etc. • Subsequent signals that transmit signals to the nucleus are common to many different types of cell. • The ultimate goal is to activate the transcription of genes, the products of which mediate host defence, proliferation, differentiation etc. Once the B cell-specific parts of the cascade are complete, signalling to the nucleus continues via three common signalling pathways via: 1.The mitogen-activated protein kinase (MAP kinase) pathway 2. Increased in intracellular Ca2+ mediated by IP3 3.The activation of Protein Kinase C mediated by DAG Simplified scheme linking antigen recognition with transcription of B cell-specific genes • MAP Kinase cascade Small G-protein-activated MAP kinases found in all multicellular animals activation of MAP kinases ultimately leads to phosphorylation of transcription factors from the AP-1 family such as Fos and Jun. • Increases in intracellular calcium via IP3 IP3, produced by PLC-g, binds to calcium channels in the ER and releases intracellular stores of Ca++ into the cytosol. Increased intracellular [Ca++] activate a phospatase, calcineurin, which in turn activates the transcription factor NFAT. • Activation of Protein Kinase C family members via DAG DAG stays associated with the membrane and recruits protein kinase C family members. The PKC, serine/threonine protein kinases, ultimately activate the transcription factor NFkB The activated transcription factors AP-1, NFAT and NFkB induce B cell proliferation, differentiation and effector mechanisms Differentiation in the periphery B B YY YY Mature peripheral B cell B cell recognises non-self antigen in periphery Y Y Y Y YY B Ig-secreting plasma cell Plasma cells Surface Surface High rate Growth Somatic Isotype Ig MHC II Ig secretion hypermut’n switch B High Yes No Yes Yes Yes Low No Yes No No No Mature B cell B Plasma cell Summary You should know: •Where B cells come from •What happens to B cells in the bone marrow •How B cell differentiation is linked with Ig gene rearrangement •The B cell developmental ‘check points’ that ensure each cell produces a single specificity of antibody that does not react with self •How B cells transmit information from the shape and charge of an antigen through the cell membrane to allow the expression of genes in the nucleus What do mature B cells do once activated by an antigen in the periphery? Recirculating B cells normally pass through lymphoid organs T cell area B cells in blood B cell area Efferent lymph Recirculating B cells are trapped by foreign antigens in lymphoid organs Antigen enters node in afferent lymphatic YY Y B cells proliferate rapidly B cells leave blood & enter lymph node via high endothelial venules Y YY Y Y Y GERMINAL CENTRE Transient structure of Intense proliferation YY Y Germinal centre releases B cells that differentiate into plasma cells B cells (stained brown) in the Germinal Centre P = Paracortex, Mn = Mantle zone SC = Subcapsular zone Follicular Dendritic cells (stained blue)in the Germinal Centre Retention of Antigens on Follicular Dendritic Cells Radiolabelled antigen localises on the surface of Follicular Dendritic cells and persists there, without internalisation, for very long periods Maturation of Follicular Dendritic cells Club-shaped tips of developing dendrites Filiform dendrites Bead formation on dendrites Bead formation on dendrites Association of antigen with FDC Antigen enters the germinal centre in the form of an immune complex with C3b and antibodies attached The Immune complexes bind to Fc and complement receptors on the FDC dendrites Ig Fc receptor Complement receptor 3 FDC surface The filiform dendrites of FDC develop beads coated with a thin layer of immune complexes Iccosome formation and release DC veils The veils of antigen-bearing dendritic cell surround the beads and the layer of immune complexes is thickened by transfer from the dendritic cell. These beads are then released and are then called ICCOSOMES Iccosomes (black coated particles) bind to and are taken up by B cell surface immunoglobulin Uptake of Iccosomes/Antigen by B cells Anti- Y Iccosomes bearing different antigens Surface Ig captures antigen Cross-linking of antigen receptor activates B cell Activated B cell expresses CD40 B cell B CD40 Fate of Antigens Internalised by B cells B 1. Capture by antigen specific Ig maximises uptake of a single antigen 2. Binding and internalisation via Ig induces expression of CD40 3. Antigen enters exogenous antigen processing pathway 4. Peptide fragments of antigen are loaded onto MHC molecules intracellularly. MHC/peptide complexes are expressed at the cell surface B T cell help to B cells Signal 2 - T cell help B Y Signal 1 antigen & antigen receptor Th Th 1. T cell antigen receptor 2. Co-receptor (CD4) 3.CD40 Ligand T cell help - Signal 2 Signal 2 Cytokines Th B IL-4 IL-5 IL-6 IFN-g TGF-b Y Cytokines Signal 1 B cells are inherently prone to die by apoptosis Signal 1 & 2 upregulate Bcl-XL in the B cell and Bcl-XL prevents apoptosis Signal 1 & 2 thus allow the B cell to survive T cells regulate the survival of B cells and thus control the clonal selection of B cells T cell help - Signal 2 activates hypermutation Signal 2 Receipt of signal 2 by the B cell also activates hypermutation in the CDR - encoding parts of the Ig genes Th B Signal 1 Y Day 6 Day 8 Day 12 Day 18 Clone 1 Clone 2 Clone 3 Clone 4 Clone 5 Clone 6 Clone 7 Clone 8 Clone 9 Clone 10 Signal 2, and thus T cells, regulate which B cells are clonally selected. Low affinity Ig takes up and presents Ag to T cells inefficiently. Inefficient presentation to T cells does not induce CD40. Deleterious mutation Beneficial mutation Neutral mutation CDR3 CDR1 CDR2 CDR3 CDR1 CDR2 CDR3 CDR1 CDR2 CDR3 CDR1 CDR2 With no signal 2 delivered by CD40, low affinity B cells die. Lower affinity - Not clonally selected Higher affinity - Clonally selected Identical affinity - No influence on clonal selection Only B cells with high affinity Ig survive - This is affinity maturation Control of Affinity & Affinity Maturation Five B cell antigen receptors all specific for , but with different affinities due to somatic hypermutation of Ig genes in the germinal centre B B B B B Only this cell, that has a high affinity for antigen can express CD40. Only this cell can receive signal 2 Only this cell is rescued from apoptosis i.e. clonally selected The cells with lower affinity receptors die of apoptosis by neglect Germinal Centre Macrophages (stained brown) Clean Up Apoptotic Cells GC = Germinal Centre, TBM = Tingible Body Macrophages Role of T cell cytokines in T cell help Signal 2 Cytokines IL-4 IL-5 IL-6 IFN-g TGF-b Th B Y Signal 1 B B B B B B B PC B B B B B B B Proliferation & Differentiation IgM IgG3 IgG1 IgG2b IgG2a IgE IgA IL4 inhibits inhibits induces inhibits induces IL-5 augments IFN-g inhibits induces inhibits induces inhibits TGF-b inhibits inhibits induces induces Regulation of specificity - Cognate recognition 1. T cells can only help the B cells that present antigen to them 2. B cells are best at presenting antigens that they take up most efficiently 3. B cells are most efficient at taking up antigens that their B cell antigen receptors bind to 4. T and B cells help each other to amplify immunity specific for the same antigen i.e. Regulates the Characteristics of Adaptive Immunity Sharply focuses specificity - Pathogen specificity Improves specificity & affinity - Better on 2nd exposure Is specific antigen dependent - Learnt by experience Seeds memory in T and B cell pools Synaptic tethering of a B cell (red) to a T cell (green) T cell (in centre) surrounded by B cells with cytoskeleton stained green Recirculating B cells are trapped by foreign antigens in lymphoid organs Antigen enters node in afferent lymphatic YY Y B cells Rapidly proliferate in follicles B cells leave blood & enter lymph node via high endothelial venules Y YY Y Y Y GERMINAL CENTRE Transient structure of Intense proliferation YY Y Germinal centre releases B cells that differentiate into plasma cells B cells (90%) and T cells (10%) migrate to form a primary follicle B B B T B B B 1. Antigen loaded dendritic cells migrate from subcapsular sinus to paracortical area of the lymph node Primary follicle formation 3. T cells proliferate T DC B B B T T B T T T B B 4. B cells migrate through HEV - most pass through the B paracortex and primary follicle. Some interact with T cells and proliferate to form a primary focus T T HEV 2. T cells migrate through HEV and are trapped by antigen on DC T cell motility in the lymph node Germinal Centre Microanatomy 2. B cells (centrocytes) upregulate surface Ig, stop dividing and receive costimulatory signals from T cells and FDC Light zone 4. Selected cells leave lymph node as memory cells or plasma cells Primary Follicles become secondary follicles B Dark zone when germinal centres develop T Follicular dendritic cells select useful B cells 3. Apoptosis of self-reactive & unselected cells 1. B cells (centroblasts) downregulate surface Ig, proliferate, somatically hypermutate their Ig genes. AFFINITY MATURATION Two B cell lineages B cell precursor Mature B cell B B Plasma cell PC B2 B cells CD5 ? B Distinct B cell precursor B Y Y Y Y Y YY Y Y Y ? IgG B1 B cells ‘Primitive’ B cells found in pleura and peritoneum IgM - no other isotypes B-1 B Cells IgM uses a distinctive & restricted range of V regions CD5 B Y Y Few non-template encoded (N) regions in the IgM Y Y IgM Recognises repeating epitope Ag such as phospholipid phosphotidyl choline & polysaccharides NATURAL ANTIBODY NOT part of adaptive immune response: No memory induced Not more efficient on 2nd challenge Present from birth Can make Ig without T cell help Comparison of B-1 and B-2 B cell properties Property N regions V region repertoire Location Renewal Spontaneous Ig production Isotypes Carbohydrate specificity Carbohydrate specificity Proteinspecificity specificity Protein Need T cell cellhelp help Somatic hypermutation of Ig Memory development B-1 cells Few Restricted Peritoneum/pleura Self renewal in situ High IgM Yes Yes Rarely Rarely No No No No B-2 cells Extensive Diverse Everywhere Bone marrow Low IgM/G/A/D/E Rarely Yes Yes Yes Yes High Yes Specificity & requirement for T cell help suggests strikingly different types of antigens are seen by B-1 and B-2 B cells T Independent Antigens (TI-2) TI-2 Antigen Immature B-2 Cell YY Mature B-1 Y Immature B cells that bind to multivalent self Ag undergo apoptosis B-2 cell repertoire is purged of cells recognising multivalent antigens during development in the bone marrow Y Y Y IgM Non-bone marrow derived B-1 cells are directly stimulated by antigens containing multivalent epitopes. No T cells are necessary Induces the expression of natural antibodies specific for TI-2 antigens T Independent Antigens (TI-1) LPS binding protein Bacterial Lipopolysaccharides, (TI-1 antigens), bind to host LPS binding protein in plasma LPS TLR 4 LPS/LPSBP is captured by CD14 on the B cell surface Toll - like receptor 4 (TLR4) interacts with the CD14/LPS/LPSBP complex CD14 B Cell Activation of B cell T Independent Antigens (TI-1 e.g. LPS) LPS complexes with CD14, LPSBP & TLR4 B B B B B B Y Y Y Y Y Y Six different B cells will require 6 different antigens to activate them At high dose TI-1 antigens (like LPS) will POLYCLONALLY ACTIVATE all of the B cells irrespective fo their specificity. TI-1 antigens are called MITOGENS Y YY YY YY YY YY Y YY YY YY YY YY YY YY YY YY YY YY YY T Dependent & Independent Antigens Induce responses in babies Induce responses in athymics Prime T cells Polyclonally activate B cells Require repeating epitopes T Dependent Antigens TI-1 Antigens TI-2 Antigens Yes No Yes No No Yes Yes No Yes No No Yes No No Yes Why are babies unresponsive to TI-2 antigens? In adults: TI-2 Antigen Immature B-2 Cell YY Mature B-1 Y Adult immature B cells that bind to multivalent self Ag undergo apoptosis Y Y Y IgM Adult non-bone marrow derived B-1 cells are directly stimulated by antigens containing multivalent epitopes produce IgM WITHOUT T cell help. Why are babies unresponsive to TI-2 antigens? In babies: All B cells, B-1 & B-2, are immature TI-2 Antigen Immature B-1 Cell Immature B cells that bind to multivalent self Ag undergo apoptosis YY As with adult B cells, immature B cells that bind multivalent self Ag undergo apoptosis Hence babies do not respond to TI-2 antigens. Babies are, therefore susceptible to pathogens with multivalent antigens such as those on pneumococcus T Dependent & Independent Antigens Induces response in babies Induces response in athymia Primes T cells Polyclonally activates B cells Requires repeating epitopes T Dependent Antigens TI-1 Antigens TI-2 Antigens Yes No Yes No No Yes Yes No Yes No No Yes No No Yes TD: Activate B-1 and B-2 B cells TI-1: Activate B-1 and B-2 B cells TI-2: Activate only B-1 B cells Examples TD: Diptheria toxin, influenza heamagglutinin, Mycobacterium tuberculosis TI-1: Bacterial lipopolysaccharides, Brucella abortis TI-2: Pneumococcal polysaccharides, Salmonella polymerised flagellin Immune effector mechanisms against extracellular pathogens & toxins NEUTRALISATION Toxin Bacterium ` Adhesion to host cells blocked Toxin release blocked Prevents invasion Prevents toxicity NEUTRALISING ANTIBODIES ` Y Effector mechanisms against extracellular pathogens OPSONISATION Bacteria in extracellular space + Ab OPSONISATION Fc receptor binding Phagocytosis Effector mechanisms against extracellular pathogens COMPLEMENT Activation Bacteria in plasma Lysis + Ab & COMPLEMENT Opsonisation Complement & Fc receptor binding Phagocytosis Summary • B cell tolerance of self is by clonal deletion or anergy of self-reactive cells • Receptor editing increases the efficiency of B cell development • Follicular dendritic cells acquire antigen and transfer it to B cells • T cell help to B cells is via CD40L and cytokines • CD40 expression indirectly leads to Ig affinity maturation • Germinal centre microanatomy & function • There are two lineages of B cells - B1 and B2 B cells • The dependency of B cells upon T cells varies