* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Endocrine Physiology lecture 3
Survey
Document related concepts
Hormone replacement therapy (female-to-male) wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Hypothalamic–pituitary–adrenal axis wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Hypothyroidism wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Vasopressin wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Graves' disease wikipedia , lookup
Hyperandrogenism wikipedia , lookup
Kallmann syndrome wikipedia , lookup
Growth hormone therapy wikipedia , lookup
Pituitary apoplexy wikipedia , lookup
Transcript
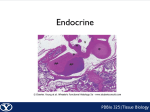
Endocrine Physiology lecture 3 Dale Buchanan Hales, PhD Department of Physiology & Biophysics Anterior pituitary • Anterior pituitary: connected to the hypothalamus by hypothalmoanterior pituitary portal vessels. • The anterior pituitary produces six peptide hormones: – – – – – prolactin, growth hormone (GH), thyroid stimulating hormone (TSH), adrenocorticotropic hormone (ACTH), follicle-stimulating hormone (FSH), luteinizing hormone (LH). Anterior pituitary cells and hormones Cell type Pituitary Product population Target Corticotroph 15-20% Thyrotroph 3-5% Adrenal gland ACTH b-lipotropin Adipocytes Melanocytes TSH Thyroid gland Gonadotroph 10-15% LH, FSH Gonads Somatotroph 40-50% GH Lactotroph 10-15% PRL All tissues, liver Breasts gonads Anterior pituitary hormones Feedback regulation of hypothalmus/pituitary A prominent feature of each of the hormonal sequences initiated by the hypothalamic releasing hormones is negative feedback exerted upon the hypothalamic-pituitary system by the hormones whose production are stimulated in the sequence. Hypothalamus-pituitary axis Feedback control Feedback control of thyroid function Feedback leads to restoration of homeostasis Feedback control of growth hormone Regulation of Growth Hormone Secretion • GH secretion controlled primarily by hypothalamic GHRH stimulation and somatostatin inhibition • Neurotransmitters involved in control of GH secretion– via regulation of GHRH and somatostatin Regulation of Growth Hormone Secretion • Neurotransmitter systems that stimulate GHRH and/or inhibit somatostatin – Catecholamines acting via a2-adrenergic receptors – Dopamine acting via D1 or D2 receptors – Excitatory amino acids acting via both NMDA and non-NMDA receptors Regulation of Growth Hormone Secretion b-adrenergic receptors stimulate somatostatin release and inhibit GH b-adrenergic receptors inhibit hypothalamic release of GHRH Regulation of Growth Hormone Secretion • Additional central mechanisms that control GH secretion include an ultra-short feedback loop exerted by both somatostatin and GHRH on their own secretion Growth hormone vs. metabolic state • When protein and energy intake are adequate, it is appropriate to convert amino acids to protein and stimulate growth. hence GH and insulin promote anabolic reactions during protein intake • During carbohydrate intake, GH antagonizes insulin effects-- blocks glucose uptake to prevent hypoglycemia. (if there is too much insulin, all the glucose would be taken up). • When there is adequate glucose as during absorptive phase, and glucose uptake is required, then GH secretion is inhibited so it won't counter act insulin action. Growth hormone vs. metabolic state • During fasting, GH antagonizes insulin action and helps mediate glucose sparing, ie stimulates gluconeogenesis • In general, during anabolic or absorptive phase, GH facilitates insulin action, to promote growth. • during fasting or post-absorptive phase, GH opposes insulin action, to promote catabolism or glucose sparing Growth hormone and metabolic state Clinical assessment of GH • Random serum samples not useful due to pulsatile pattern of release • Provocative tests necessary – GH measurement after 90 min exercise – GH measurement immediately after onset of sleep • Definitive tests – GH measurement after insulin-induced hypoglycemia – Glucose suppresses GH levels 30-90 min after administration– patients with GH excess do not suppress – Measurement of IGF-1 to assess GH excess Acromegaly and Gigantism • Caused by eosinophilic adenomas of somatotrophs • Excess GH leads to development of gigantism if hypersecretion is present during early life– a rare condition – Symmetrical enlargement of body resulting in true giant with overgrowth of long bones, connective tissue and visceral organs. • Excess GH leads to acromegaly if hypersecretion occurs after body growth has stopped. – Elongation of long bones not possible so there is over growth of cancellous bones– protruding jaw, thickening of phalanges, and over growth of visceral organs Acromegaly Acromegaly A) before presentation; B) at admission Harvey Cushing’s first reported case Gigantism Identical twins, 22 years old, excess GH secretion ACTH: adrenocorticotropic hormone: synthesis and regulation of secretion • Produced in corticotrophs • ACTH is produced in the anterior pituitary by proteolytic processing of Prepro-opiomelanocortin (POMC). • Other neuropeptide products include b and g lipotropin, b-endorphin, and a-melanocytestimulating hormone (a-MSH). • ACTH is a key regulator of the stress response ACTH synthesis ACTH Processing and cleavage of pro-opiomelanocortin (POMC) ACTH ACTH is made up of 39 amino acids Regulates adrenal cortex and synthesis of adrenocorticosteroids a-MSH resides in first 13 AA of ACTH a-MSH stimulates melanocytes and can darken skin Overproduction of ACTH may accompany increased pigmentation due to a-MSH. Addison’s Disease • Disease in which patients lack cortisol from zona fasiculata, and thus lacks negative feedback that suppresses ACTH production • Result: overproduction of ACTH • Skin color will darken • JFK had Addison’s disease and was treated with cortisol injections b-endorphin • • • • Produced as a result of ACTH synthesis Binds to opiate receptors Results in “runner’s high” Role in anterior pituitary not completely understood • One of many endogenous opioids such as enkephalins Melanocyte-stimulating hormone (MSH) • MSH peptides derived by proteolytic cleavage of POMC a-MSH has antipyretic and anti-inflammatory effects – Also inhibits CRH and LHRH secretion • • • • Four MSH receptors identified May inhibit feeding behavior ACTH has MSH-like activity However– MSH has NO ACTH like activity Regulation of ACTH secretion Regulation of ACTH secretion • Stimulation of release – CRH and ADH – Stress – Hypoglycemia • CRH and ADH both synthesized in hypothalamus – ADH (a.k.a. vasopressin) is released by posterior pituitary and reaches anterior pituitary via inferior hypophyseal artery. Regulation of ACTH secretion • Deficiency of vasopressin (ADH) in hereditary diabetes insipidus is accompanied by decreased ACTH release. • Vasopressin potentiates CRH at both hypothalamic and pituitary levels. • Many vasopressinergic neurons also contain CRH resulting in co-release of two peptides into portal blood. ACTH • Circadian pattern of release – Highest levels of cortisol are in early AM following ACTH release – Depends on sleep-wake cycle, jet-lag can result in alteration of pattern • Opposes the circadian pattern of growth hormone secretion Regulation of ACTH ACTH • Acts on adrenal cortex – stimulates growth of cortex (trophic action) – Stimulates steroid hormone synthesis • Lack of negative feedback from cortisol results in aberrantly high ACTH, elevated levels of other adrenal corticosteroids– adrenal androgens • Adrenogenital syndrome: masculization of female fetus Glycoprotein hormones LH, FSH, TSH and hCG a and b subunits Each subunit encoded by different gene a subunit is identical for all hormones b subunit are unique and provide biological specificity Glycoprotein hormones Glycoprotein hormones contain two subunits, a common a subunit and a distinct b subunit: TSH, LH, FSH and hCG. Gonadotrophs • Cells in anterior pituitary that produce LH and FSH • Synthesis and secretion stimulated by GnRH– major effect on LH • FSH secretion controlled by inhibin • Pulsitile secretion of GnRH and inhibin cause distinct patterns of LH and FSH secretion LH/FSH • Pulsatile pattern of secretion – LH pulses are biphasic (every 1 minute, then large pulse at 1 hour) – FSH pulses are uniphasic • Diurnal– LH/FSH more pronounced during puberty • Cyclic in females– ovarian cycle with LH surge at time of ovulation • Males are not cyclic, but constant pulses of LH cause pulses of testosterone to be produced Pulsitile secretion of GnRH and LH Regulation of LH/FSH • Negative feed-back – Inhibin produced by testes and ovaries Decreases FSH b-subunit expression – Testosterone from Leydig cells– synthesis stimulated by LH, feedsback to inhibit GnRH production from hypothalamus and down-regulates GnRH receptors – Progesterone– suppresses ovulation, basis for oral contraceptives. Works at both the level of pituitary and hypothalamus. Regulation of LH/FSH • Dopamine, endorphin, and prolactin inhibit GnRH release. – Prolactin inhibition affords post-partum contraceptive effect • Overproduction of prolactin via pituitary tumor can cause amenorrhea– shuts off GnRH – Treated with bromocryptine (dopamine agonist) – Surgical removal of pituitary tumor Regulation of LH/FSH • Positive feedback – Estradiol at high plasma concentrations in late follicular phase of ovarian cycle stimulates GnRH and LH surge– triggers ovulation Regulation of gonadotropin secretion Thyrotrophs • • • • Site of TSH synthesis Pattern of secretion is relatively steady TSH secretion stimulated by TRH Feedback control by T3 (thyroid hormone) Feedback control of thyroid function Grave’s disease • Hyperthyroidism caused by circulating antibodies to the TSH receptor. • Associated with diffuse goiter. • Autoantibodies bind to TSH receptor and mimic the action of TSH itself leads to persistent stimulation of thyroid and elevated levels of thyroid hormones. Lacotrophs • Site of production of prolactin • Lactogenesis (milk synthesis) requires prolactin • Tonically inhibited – Of the anterior pituitary hormones, the only one – Multifactoral control, balance favors inhibition • Dopamine inhibits prolactin • Prolactin releasing hormone is TRH – Ocytocin also stimulates prolactin release – Estradiol enhances prolactin synthesis Prolactin • Stimulates breast development and lactogenesis • May be involved in development of Leydig cells in pre-pubertal males • Immunomodulatory effects– stimulates T cell functions – Prolactin receptors in thymus Clinical assessment of PRL • Single basal serum PRL measurement sufficient to determine excess – PRL deficiency not a usual clinical concern • PRL is only anterior pituitary with predominant negative control by hypothalamus– often elevated by lesions that interfere with portal blood flow. • Elevated by primary PRL adenomas of pituitary Posterior pituitary hormones: ADH (AVP) and Oxytocin (hypothalamic hormones) Both are synthesized in the cell bodies of hypothalamic neurons ADH: supraoptic nucleus Oxytocin: paraventricular nucleus Both are synthesized as preprohormones and processed into nonapeptides (nine amino acids). They are released from the termini in response to an action potential which travels from the axon body in the hypothalamus Hypothalamus and posterior pituitary Structures of ADH and oxytocin Oxytocin: stimulates myoepithelial contractions In uterus during parturition In mammary gland during lactation Oxytocin: milk ejection from lactating mammary gland suckling is major stimulus for release. sensory receptors in nipple connect with nerve fibers to the spine, then impulses are relayed through brain to PVN where cholinergic synapses fire on oxytocin neurons and stimulate release. Oxytocin: uterine contractions • Reflexes originating in the cervical, vaginal and uterus stimulate oxytocin synthesis and release via neural input to hypothalamus • Increases in plasma at time of ovulation, parturition, and coitus • Estrogen increases synthesis and lowers threshold for release Oxytocin secretion is stimulated by nursing