* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download This page should automatically redirect. If nothing is
Survey
Document related concepts
Transcript
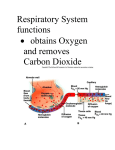
Respiration If you can’t breathe, nothing else matters! ® American Lung Association COPD Chronic Obstructive Pulmonary Disease (COPD), is the fourth leading cause of death in the United States, a major cause of death throughout the world, and the third leading cause for disability in the United States. No wonder that when the doctor utters those initials, "COPD" or "Emphysema," for the first time, the individual goes into a state of shock and depression. 1. Lateral cartilage 2. Inferior concha 3. Middle concha 4. Superior concha 5. Sphenoid sinus 6. Nasal septum Functions of the internal nose! The interior structures of the nose are specialized for three functions: (1) incoming air is warmed, moistened, and filtered; (2) olfactory stimuli are received; and (3) large hollow resonating chambers are provided for speech sounds. In addition, mucous membranes trap dust particles and, with the help of cilia, move unwanted particles to the throat for elimination. 1.Nasal cavity 2.Hard palate 3.Tongue 4.Soft palate 5.Larynx 6.Spinal column 7.Spinal cord 8.Trachea Larynx This diagram shows the view of the larnyx as seen from above. Note the position of the epiglottis and the vocal cords. Check out the model! Review Identify each of the numbered structures: 1. 2. 3. 4. 5. 6. 7. What is the identity of the U shaped structure at the bottom of the above photograph? What is(are) its function. 1. Hyoid bone 2. Thyroid cartilage 3. Cricoid cartilage 4. Tracheal cartilages The Chest Cavity Thorax This is a view of the thorax showing the mediastinum and heart separating the two lungs. Each lung is within a separate pleural cavity with the Visceral pleura tightly associated with the surface of the lungs and the Somatic Pleura associated with the inside of the thoracic wall. The somatic pleura also covers the diaphragm which forms the floor of the thoracic cavity Organs of thorax This photograph shows the larynx, trachea, primary bronchi and the great vessels of the heart all of which are found in the mediastinum. The nerves serving the diaphragm and the heart can also be identified. The two lungs are seen with a Cardiac notch present in the left lung. What is found in this notch. The Trachea and the Lungs Trachea The Trachea consists of smooth muscle, elastic connective tissue, and incomplete rings of cartilage shaped like a series of letter C's. The open ends of the C's are held together by the trachealis muscle. The cartilage provides a rigid support so that the tracheal wall does not collapse inward and obstruct the air passageway, and, because the open parts of the C's face the esophagus, the latter can expand into the trachea during swallowing. If the trachea should become obstructed, a tracheostomy may be performed. Another method of opening the air passageway is called intubation, in which a tube is passed into the mouth and down through the larynx and the trachea. Primary Bronchii and Trachea The Primary Bronchi and Trachea are seen in the center of this image. What is the major blood vessel seen as red located just to the left side of the trachea? At the bifurcation of the trachea, on the midline, is a sensitive area called the Carina which represents a receptor for the cough reflex. Particles falling on this ridge of tissue initiates a forceful explusion as part of a cough. The Trachea and The Bronchi Bronchial Tree The Trachea terminates by dividing into a Right Primary Bronchus, going to the Right Lung, and a Left Primary Bronchus, to the Left Lung. They continue dividing in the lungs into smaller bronchi, the secondary (lobar) bronchi, one for each lobe of the lung. These bronchi, in turn, continue dividing into still smaller bronchi called Tertiary (Segmental) Bronchi, which divide into Bronchioles. The next division is into even smaller tubes called Terminal Bronchioles. This entire branching structure of the trachea is commonly referred to as the Bronchial Tree. What are the lungs? The lungs are multi-lobed, bilateral, spongy organs involved in the process of respiration and which lie enclosed within the chest cavity. The right lung has three sections, called lobes; it is a little larger than the left lung, which has two lobes. When we breathe in, the lungs take in oxygen, which our cells need to live and carry out their normal functions. When we breathe out, the lungs get rid of carbon dioxide, which is a waste product of the body's cells. Major surface features of the Broad inferior portion lungs include: 1. Base resting on diaphragm. 2. Apex Narrow superior portion just above clavicles. 3. Costal surface Surface lying against ribs. 4. Mediastinal surface Medial surface. 5 . Hilus Region in mediastinal surface through which bronchial tubes, blood vessels, lymphatics, and nerves enter and exit the lung. 6. Cardiac notch Medial concavity in left lung in which heart lies. Squamous pulmonary The alveolar wall:1) epithelial cells Large cells that form a continuous lining of the alveolar wall, except for occasional septal cells. 2) Septal cells Cuboidal cells dispersed among squamous pulmonary epithelial cells that secrete a phospholipid substance called Surfactant, a surface tension lowering agent. 3) Alveolar macrophages (dust cells)Phagocytic cells that remove dust particles and other debris from the alveolar spaces. Alveolar-capillary membrane The exchange of respiratory gases between the lungs and blood takes place by diffusion across the alveolar and capillary walls. This membrane, through which the respiratory gases move, is collectively known as the alveolar-capillary membrane. 1. A layer of squamous pulmonary epithelial cells with septal cells and free alveolar macrophages (dust cells) that constitute the alveolar (epithelial) wall. 2. An epithelial basement membrane underneath the alveolar wall. 3. A capillary basement membrane that is often fused to the epithelial basement membrane. 4. The endothelial cells of the capillary. Measurement of Respiratory Volumes The word respiration refers to one complete respiratory cycle, including one inspiration and one expiration. A normal adult has 14 to 18 respirations in a minute, during which the lungs exchange specific volumes of air with the atmosphere. Tidal Volume As the following respiratory volumes and capacities are discussed, keep in mind that the values given vary with age, height, sex, and physiological state. The volume of air expired under normal, quiet inspiration is approximately 500 ml. The volume of air expired under normal, quiet breathing conditions is equal to that of inspiration, and this volume of air is called Tidal Volume. Dead Spaces Only approximately 350 ml of this tidal volume reaches the alveoli. The other 150 ml of air is called Dead Air volume because it remains in the spaces not designed for air exchange (Anatomical dead space ) (nose, pharynx, larynx, trachea, and bronchi) as well as those areas designed for air exchange but not currently being utilized by the lungs (Physiological dead space). Total Air Volume Inspiratory reserve volume ~ take in a breath, without exhaling, take in as much air as you can. Expiratory reserve volume ~ Exhale normally and without inhaling exhale as much as you can. (TV + ERV = ERC) Residual volume ~ Even with forceful expiration there is still air remaining in the lungs. Vital capacity ~ is equal to the volume of air that can be forcibly exhaled following maximal inspiratory effort (IRV + TV +ERC) Spirogram Diaphragm and pericardial sac This a view of the base of the thoracic cavity showing the muscular diaphragm crowning medially. Attached to the medial portion of the diaphragm is the fibrous membrane which forms the Percardial sac.