* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 37 - BristolPlymouth21stCenturyHealth
Survey
Document related concepts
Hypothyroidism wikipedia , lookup
Hypothalamus wikipedia , lookup
Metabolic syndrome wikipedia , lookup
Growth hormone therapy wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Graves' disease wikipedia , lookup
Hyperandrogenism wikipedia , lookup
Hypoglycemia wikipedia , lookup
Insulin resistance wikipedia , lookup
Diabetic hypoglycemia wikipedia , lookup
Gestational diabetes wikipedia , lookup
Diabetes management wikipedia , lookup
Complications of diabetes mellitus wikipedia , lookup
Diabetic ketoacidosis wikipedia , lookup
Transcript
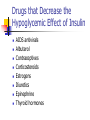
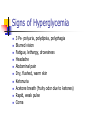
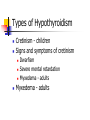
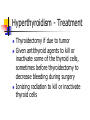
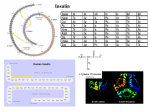
Chapter 43 Antidiabetic Drugs Revised 11/10 Diabetes A complicated, chronic disorder characterized by insufficient insulin production or by cellular resistance to insulin Two Types of Diabetes Type 1—insulindependent diabetes mellitus (IDDM) Insulin produced in insufficient amounts Requires insulin Type 2—non-insulindependent diabetes mellitus (NIDDM) Decreased production of insulin or decreased cell sensitivity to insulin May be treated with oral drug and/or insulin Four Pillars of Management of Diabetes Meal planning referred to as medical nutrition therapy Activity and exercise Medication Self monitoring of blood glucose (SMBG) Insulin A hormone produced by the pancreas that acts to maintain blood glucose levels within normal limits Insulin is a high alert medication Insulin Essential for the use of glucose in cellular metabolism and for proper protein and fat metabolism Insulin A hormone produced by the beta cells of the pancreas Controls the use of glucose, protein, and fat in the body Lowers blood sugar by inhibiting glucose production by the liver FA Davis, FON, onset, peaks, duration. See handout from pharm 1 (corrections made) Insulin Available as purified extracts from beef and pork pancreas (used infrequently) Synthetic insulins, such a human insulin and insulin analogs;derived from strains of Escherichia coli (recombinant DNA), fewer allergies with this than extracts of beef and pork Activates a process that helps glucose molecules enter the cells Stimulates the liver glycogen synthesis Insulin (Con’t) Used to treat diabetes mellitus and control more severe and complicated forms of type 2 diabetes Insulin Injections: Must be injected into the subcutaneous in the legs, arms, stomachs or buttocks. Cannot be taken orally- it’s a protein and the stomach acid would break it down before it could be used. Newer forms include Insulin Pump ADMINISTERING INSULIN BY INJECTION Administered with an insulin syringe ( syringe calibrated in units) Various insulin syringes hold volumes of 0.3, 0.5, and 1 mL The standard dosage strength of insulin is 100 U/mL Low dose insulin syringes are used to deliver insulin in 30-50 U or less A standard insulin syringe can administer up to 100 U of insulin Insulin Syringe Size is ½ inch Insulin Preparations See handout from Introduction to Pharmacology Text, page 411 New insulin Levemir (similar to Lantus, cannot mix with other insulins) Considered a basal insulin like NPH and Lantus (covers the body’s basal metabolic needs in the absence of food) Onset, Peak, and Duration of Action Define onset, peak and duration Refer to Handout from Introduction to Pharmacology Text, page 411, must memorize onset, peak and duration of each type of insulin (review of introduction to pharmacology) Hypoglycemia reactions can occur anytime but most common during peak (treat with OJ, hard candy, glucose tabs, glucagon, Glucose 10% & 50% IV). Make sure patient has swallowing and gag reflexes for po method) Insulin Contraindications Contraindicated if patient has hypersensitivity to any ingredient in the product (older preparations made with beef and pork) and if the patient is hypoglycemic Precautions Used cautiously with renal and hepatic impairment and during pregnancy and lactation Interactions See Display 43-1 Drugs that Decrease and Increase the Hypoglycemic Effect of Insulin, page 412 Include as nursing considerations Also review on page 412 signs and symptoms of hypoglycemia and hyperglycemia Drugs that Decrease the Hypoglycemic Effect of Insulin AIDS antivirals Albuterol Contraceptives Corticosteroids Estrogens Diuretics Epinephrine Thyroid hormones Drugs that Increase the Hypoglycemic Effect of Insulin Alcohol Ace inhibitors Oral antidiabetic drugs Calcium Clonidine Lithium MAOIs Salicylate Sulfonimides Tetracycline MIXING INSULINS Insulins tend to bind and become equilibrated Inject within 5 minutes of mixing Regular which is additive free, is combined with intermediate-acting insulin such as Humulin Mixing Insulins Promoting Optimal Response to Insulin Therapy Will be individualized Expect adjustments when under stress and with any illness, particularly illnesses resulting in nausea and vomiting Examples of Insulin Administration using a Sliding Scale Handout from Morton Hospital (use as an example) Double sided (reverse has how to treat hypoglycemia) Follow agency protocol Preparing Insulin for Administration Current insulin bottle at room temperature, except Lantus which is refrigerated Check expiration (dated at time of opening and used for a one month period) Do not shake, rotate gently, invert gently for those insulins in suspension Rotating Injection Sites Rotating sites prevents lipodystrophy (atrophy of subcutaneous fat) Lipodystrophy interferes with absorption of insulin Appears as a slight dimpling or pitting of SC fat Ask patient about particular site rotation schedule Newer philosophy involves using all sites in one area before moving to another body part See text, page 551 Body Diagram of Appropriate Sites Methods of Administering Insulin Parenteral-subcutaneous or intravenous Insulin Pump Inhalation- research continues, Exubria (Pfizer) taken off market, Dec. 2008 due to risks with lungs/complications Insulin Pumps Newer technology. Attempts to mimic the body’s normal pancreatic function. Only regular insulin is used. Needle inserted subcutaneously and left in place for 1-3 days Battery operated. Amount of insulin injected can be adjusted according to blood glucose levels (monitored 4-8 times a day) Inhaled Insulin- Recently taken off market- only FYI Food and Drug Administration approved the first noninjectable insulin in a dry inhalation powder in early 2006 (Exubera) Exubera was a rapid acting insulin and must be taken within 10 minutes of a meal. Peaks 90-120 minutes similar to rapid acting analogs (Humalog, Novolog, Apidra). Duration was 6 hours. Contraindicated in people who smoke or recently stopped within 6 months, or poorly controlled lung disease, and during pregnancy. Dosing- not supplied in international units, rather 1 mg or 3 mg blisters. (1 mg blister equivalent to 3 units; 3 mg blister equivalent to 8 units (physics/ cloud burst) Directions: load, apply pressure, inhale, hold breath for 5 seconds at the end of inhalation. Monitoring and Managing Adverse Reactions Must know signs and symptoms of hypoglycemia and hyperglycemia Signs of Hyperglycemia 3 Ps- polyuria, polydipsia, polyphagia Blurred vision Fatigue, lethargy, drowsiness Headache Abdominal pain Dry, flushed, warm skin Ketonuria Acetone breath (fruity odor due to ketones) Rapid, weak pulse Coma Signs of Hypoglycemia Headache Hunger Fight or flight Neuroglycopenia Shaky Cold sweat (cool, clammy skin, diaphoresis) “Cold and clammy, need some candy” Palpitations Tachycardia Irritability, nervousness, anxiety Confusion Blurred vision General weakness Drowsiness Seizures, coma CAUTION Autonomic neuropathy: No symptoms Educating the Patient and Family Review principles of teaching the adult patient Noncompliance may be a problem with some patients (may be related to lack of understanding of disease process or medications or management) Establish a thorough teaching plan for patients newly diagnosed, for patients with changes in treatment plan Include teaching on diet, glucose monitoring, medications, adverse reactions, hygiene, exercise, sick day protocols, medic alert bracelets Nursing Diagnoses Anxiety and Fear Impaired Adjustment, Coping, and Altered Health Maintenance Acute confusion related to hypoglycemic reaction Glucose, risk for instable blood glucose Oral Drugs Sulfonylureas Biguanides Alpha-glucosidase inhibitors Meglitinides Thiazolidinediones Hormone Mimetic Agents –many different actions to help lower blood sugar levels, see page 424; Januvia, Byetta, Symlin See Summary of Drugs- pages 556-557 Sometimes oral antidiabetic drugs are used in combinations Sulfonylureas Examples—tolbutamide (Orinase), glipizide (Glucotrol), glyburide (Diabeta, Micronase), glimepiride (Amaryl) Act to lower blood glucose by stimulating the beta cell to release insulin Adverse Reactions—hypoglycemia, anorexia, nausea, vomiting, epigastric discomfort, weight gain, heartburn, weakness and numbness of extremities Nursing considerations:Glucotrol given 30 minutes before a meal, glyburide is given with breakfast. Avoid alcohol (has a disulfiram-like reaction(Antabuse)-flushing, throbbing in head and neck, respiratory difficulty, vomiting, sweating, chest pain and hypotension, arrhythmias, and unconsciousness Secondary failure may occur (may lose effectiveness,; may prescribe another sulfonylureas or add another oral antidiabetic drug such as metformin Biguanides Example—metformin (Glucophage) Action—reduces hepatic glucose production and increases insulin sensitivity to muscle and fat cells. May cause weight loss, favorable SE includes lowering of triglycerides and LDL cholesterol Adverse Reactions—gastrointestinal (GI) upset (abdominal bloating, nausea, cramping, diarrhea, etc), metallic taste, hypoglycemia (rare) Rare SE: lactic acidosis with kidney failure Nursing implications; give with meals. Glucophage XR given once daily with evening meal. Glucophage must be stopped 48 hours before and after radiology studies that use iodine. Monitor renal function. Alpha-Glucosidase Inhibitors Examples—acarbose, miglitol Action—lower blood sugar by delaying carbohydrate digestion and absorption Adverse Reactions—bloating and flatulence, abdominal pain, diarrhea Nursing considerations: given with first bite of the meal because food increases absorption. Monitor liver function Meglitinides Examples—nateglinide (Starlix), repaglinide (Prandin) Action—stimulate insulin release from the pancreas in response to a glucose load. Has short duration of action, thus reduces the potential for hypogylcemic reactions. Adverse Reactions – upper respiratory infection (URI), headache, rhinitis, bronchitis, headache, back pain, hypoglycemia Nursing considerations: give 15-30 minutes before meal. Disadvantage- need to take up to 4 doses a day Thiazolidinediones Examples—rosiglitazone (Avandia-December 2008, FDA announced safety issues and increase of cardiac related deaths, off market), pioglitazone (Actos) Action—decrease insulin resistance and increase insulin sensitivity by modifying several processes. . Increases sensitivity of muscle and fat tissue to insulin Adverse Reactions—aggravated diabetes mellitus, URI, sinusitis, headache, pharyngitis, myalgia, diarrhea, back pain Nursing considerations: delay of a meal for as little as 30 minutes can cause hypoglycemia. Monitor liver function. Reduces the blood level of some oral contraceptives Combination Agents Metaglip- glipizide and metformin Glucovance-glyburide and metformin Actoplus Met- pioglitazone and metformin Avandamet- rosiglitazone and metformin Duetact- Pioglitazone and glimepiride Avandaryl- rosiglitzone and glimepride Pharmacologic Algorithm for Treating Type 2 Diabetes See text, page 558 Emergency Medications to ELEVATE Glucose Glucagon IM (glucagon is a hormone produced by the alpha cells of the pancreasstimulates the conversion of glycogen to glucose in the liver. . return to consciousness within 5-20 minutes, if no response, suggests a lack of available hepatic glycogen and will need to administer IV dextrose) IV D50 Key Concepts for Insulin Know which insulins can or cannot be mixed (Lantus cannot be mixed) Concentration of U100 most commonly used Check expiration date, name, concentration each time Rotate cloudy suspensions Check orders/verify with 2nd nurse per agency protocol No air bubbles Rotate sites Familiarize self with needle size, pens, dials, pumps Hypoglycemic reactions can occur anytime, but most common during insulin peak time Proper storage-room temperature if used within one month, refrigerate up to 3 months Prefilled syringes are stable for one week Insulin needs change if stressed or ill Travel with supplies and snacks Know signs and symptoms of hyper and hypoglycemia Case Study Timothy Jones is admitted to your unit with a diagnosis of new onset type 1 diabetes mellitus. His blood sugars have stabilized and he is beginning to ask questions. How would you answer the following questions? What is diabetes? Why can’t I be on pills instead of insulin? Why do I have to test my blood sugars? What should I do if it is too high or too low? Does insulin have any side effects? What should I watch for? Develop a Care Plan for Mr. Jones, a 22 year old newly diagnosed with Type 1 diabetes MD orders include: Test blood sugars ac and hs Regular insulin sc coverage ac and hs Sliding scale: < 200 no coverage 201-250---2 u 251-300---4 u 301-350---6 u 351-400---8 u > 400 Call MD Humulin N 20 units sc 7:30 am 1800 ADA diet Videos or Workbook Activities Insulin Injections Novo Pen 3 Workbook, chapter 43 Review of Introduction NCLEX and Pharmacology Generic names for medications, may use brand name if only one brand name available May give clues such as drug classification May ask question(s) by drug classification Core Concepts in Pharmacology Second Edition Norman Holland and Michael Patrick Adams Chapter 29 Drugs for Endrocrine Disorders The Endocrine System Consists of glands that secrete hormones Hormones are released as changes in the body occur Hormones are transported by the blood through the body One hormone may control the secretion of another hormone Hormone action is controlled by a negative feedback mechanism Utilization of Hormones Replacement therapy for patients who are unable to secrete sufficient quantities of endogenous hormones Thyroid hormone - following a thyroidectomy Insulin - when the pancreas is not functioning Given in the same low-level amounts as if secreted by the gland Utilization of Hormones (cont’d) Cancer chemotherapy Testosterone for breast cancer Estrogen for testicular cancer Given in doses much larger than normally secreted by the gland Used to produce an exaggerated response Hydrocortisone - suppress inflammation Estrogen or progesterone - prevent ovulation and pregnancy The Hypothalamus and the Pituitary Gland Hypothalamus secretes releasing factors (hormones) that travel by way of the blood to the anterior pituitary Releasing factors tell pituitary which hormone to release Pituitary gland releases the appropriate hormone into the blood, which travels to its target organ to cause its effect Thyrotropin-releasing hormone (hypothalamus) Thyroid-stimulating hormone (pituitary gland) Thyroid hormone (thyroid gland-target organ) Pancreas Essential to both the digestive and endocrine systems Exocrine function - secretes several enzymes into the duodenum via the pancreatic duct Assist in chemical digestion Endocrine function - islets of Langerhans secrete glucagon and insulin directly into the blood Insulin Secretion Regulated by a number of chemicals, hormonal and nervous factors Glucose in the blood stimulates islets of Langerhans in the pancreas to secrete insulin Insulin affects carbohydrate, lipid, and protein metabolism Without insulin glucose can’t enter the cells to be used for fuel Glucagon Secreted by the islets of Langerhans in the pancreas Secreted when levels of glucose in the blood are low Maintains adequate levels of glucose in the blood between meals Moves glucose from liver to the blood Type 1 Diabetes Mellitus Aka juvenile-onset diabetes Lack of insulin secretion by the pancreas Genetic component Signs and symptoms Hyperglycemia Polyuria Polyphagia Polydipsia Glucosuria Weight loss Fatigue Type 2 Diabetes Mellitus Aka adult-onset diabetes Pancreas secretes insulin in small amounts but insulin receptors in target cells insensitive or resistant to insulin Common in overweight clients and those having low HDL-cholesterol and high triglyceride levels Untreated Both Type 1 and Type 2 Can Produce Serious Long-Term Damage To blood vessels in heart, brain, kidneys, eyes, legs, and feet To peripheral nerves in hands and feet Type 1 Diabetes - Treatment Type 1 diabetes is treated with a combination of diet, exercise, and insulin Meals regularly, every 4–5 hours, to regulate blood glucose levels Regular, moderate exercise to help cells respond to insulin Insulin therapy to keep blood glucose levels within normal limits Type 2 Diabetes - Treatment Controlled through lifestyle changes and oral hypoglycemic agents Proper diet and exercise can sometimes increase sensitivity of insulin receptors Type 2 Diabetes - Treatment (cont’d) Oral hypoglycemic drugs When diet and exercise have failed to decrease the blood glucose Five classes of oral hypoglycemics Classifications based on chemical structure and mechanism of action Therapy initiated with a single agent Oral hypoglycemics are effective when taken on a regular basis Drug Profile - Oral Hypoglycemic Glipizide (Glucotrol), second generation sulfonylurea Actions and uses Adverse effects and interactions Mechanism in action Insulin Therapy Five types of insulin available, differing in onset of action and duration of action Table 29.2 Insulin Preparations Table 29.2 (continued) Insulin Preparations Insulin Therapy (cont’d) Most insulin today obtained through recombinant technology Routes of administration: Most common route is subcutaneous Only regular insulin can be given IV Insulin pumps are being used Research to discover new routes - nasal spray Doses of insulin highly individualized Self-monitoring of blood glucose is important Drug Profile - Insulin Regular insulin (Humulin R, Novolin R) Actions and uses Adverse effects and interactions Mechanism in action Hypoglycemia Can Result From: Insulin overdose Improper timing of insulin dose Skipping a meal Signs and Symptoms of Hypoglycemia Tachycardia Confusion Sweating Drowsiness Without quick treatment you will see convulsions, coma, and death Hyperglycemia Can Result From: Underdose of insulin or hypoglycemic agent Signs and symptoms of hyperglycemia Fasting blood glucose greater than 126 mg/dl Polyuria Polyphagia Polydipsia Glucosuria Weight loss/gain Fatigue Thyroid Follicular cells secrete thyroid hormones Thyroxine (tetraiodothyronine or T4) Triiodothyronine (T3) Iodine is necessary for the production of these hormones Found in iodized salt Parafollicular cells secrete calcitonin Involved with calcium homeostasis Thyroid Function Multiple levels of hormonal control TRH stimulates the pituitary gland to produce and secrete TSH TSH stimulates the thyroid gland to produce and secrete thyroid hormones into the blood Thyroid Function (cont’d) When thyroid hormones reach a certain level in the blood, the secretions of TRH and TSH are slowed down This slowing down is known as a negative feedback loop If thyroid hormone levels in the blood drop then more TRH and TSH will be secreted Thyroid Hormone Affects Every Cell in the Body Regulates basal metabolic rate Critical to growth of the nervous system Hypothyroidism Causes of insufficient secretion of TSH or thyroid hormone Consequences of autoimmune disease Surgical removal of thyroid gland Aggressive treatment with antithyroid drugs Types of Hypothyroidism Cretinism - children Signs and symptoms of cretinism Dwarfism Severe mental retardation Myxedema - adults Myxedema - adults Types of Hypothyroidism (cont’d) Signs and symptoms of myxedema Slowed body metabolism Slurred speech Bradycardia, weight gain Low body temperature Intolerance to cold Treatment for Both Types Is Natural or Synthetic Thyroid Hormone Hyperthyroidism - Too Much Thyroid Hormone Secreted Graves’ disease - severe form of hyperthyroidism Signs and symptoms Increased body metabolism Tachycardia, weight loss High body temperature Anxiety Hyperthyroidism - Treatment Thyroidectomy if due to tumor Given antithyroid agents to kill or inactivate some of the thyroid cells, sometimes before thyroidectomy to decrease bleeding during surgery Ionizing radiation to kill or inactivate thyroid cells Adrenal Gland Cortex Medulla Adrenal Cortex Secrete several classes of steroid hormones Glucocorticoids Mineralocorticoids Androgens The three hormones are referred to as corticosteroids or adrenocortical hormones Mineralocorticoid Aldosterone Increases the renal absorption of sodium in exchange for potassium Glucocorticoid CRF secreted from the hypothalamus Causes release of ACTH from the pituitary gland Glucocorticoids are released from the adrenal cortex As the glucocorticoid level rises, hormones are shut off Glucocorticoids Affect Metabolism of Nearly Every Cell During long-term stress, mobilize the formation of glucose Increase the breakdown and utilization of proteins and lipids Potent anti-inflammatory effect Promote homeostasis of the cardiovascular, nervous, and musculoskeletal systems Adrenocortical Insufficiency Decrease production of corticosteroid Causes Hyposecretion by adrenal cortex Inadequate secretion of ACTH from pituitary Signs and symptoms Hypoglycemia Fatigue Hypotension GI disturbances Primary adrenocortical insufficiency - Addison’s Disease Quite rare Deficiency of both glucocorticoids and mineralocorticoids Treated with glucocorticoid replacement therapy Secondary Adrenocortical Insufficiency Relatively common Long-term therapy with glucocorticoids that is abruptly discontinued Treated with glucocorticoid replacement therapy Insulin Table 29.2 Insulin Preparations Table 29.2 (continued) Insulin Preparations Oral Hypoglycemics Table 29.3 Oral Hypoglycemics Table 29.3 (continued) Oral Hypoglycemics Table 29.3 (continued) Oral Hypoglycemics Thyroid and Antithyroid Agents The correct dose is highly individualized Requires periodic adjustments Table 29.4 Thyroid and Antithyroid Medications Hypothyroidism Slows the Body’s Metabolism Administration of thyroid hormone reverses that effect Drug Profile - Thyroid Agent Levothyroxine (Synthroid) Actions and uses Adverse effects and interactions Mechanism in action Hyperthyroidism Speeds the Body’s Metabolism Administer drugs that kill or inactivate thyroid cells Drug Profile - Antithyroid Agent Propylthiouracil (Propacil) Actions and uses Adverse effects and interactions Mechanism in action Glucocorticoids Are Used to Treat: Inflammatory and immune responses Disorders that may be treated with corticosteroids Allergies, seasonal rhinitis, asthma Contact dermatitis and rashes Hodgkin’s disease, leukemias, lymphomas Shock Rheumatoid arthritis, ankylosing spondylitis, bursitis Ulcerative colitis, Crohn’s disease Hepatic, neurological, renal disorders with edema Following transplant surgery Significant Adverse Effects Can Occur During Long-Term Therapy Known as Cushing’s Syndrome Adrenal atrophy Osteoporosis Increased risk of infections Delayed wound healing Peptic ulcer Accumulation of fat around shoulders and neck Mood and personality changes Drug Profile - Glucocorticoid Hydrocortisone (Cortef) Actions and uses Adverse effects and interactions Mechanism in action Growth Hormone - Aka Somatotropin Secreted by pituitary gland Stimulates growth of cell Deficiency in children Dwarfism with no mental impairment Growth Hormone Medications for Dwarfism in Children Somatrem (Protopin) Somatropin (Humantrope) Not approved to stimulate growth in short children Antidiuretic Hormone Produced by the hypothalamus Secreted from the posterior pituitary gland Increases water absorption by kidneys Raises blood pressure if secreted in large amounts Diabetes insipidus - deficiency of ADH Treatment of Diabetes Insipidus Vasopressin (Pitressin) Desmopressin (DDAVP, Stimate) Lopressin (Diapid) Desmopressin used for enuresis - nasal spray