* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download AminoAcidMetabolismFIN2011
Western blot wikipedia , lookup
Two-hybrid screening wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Catalytic triad wikipedia , lookup
Nitrogen cycle wikipedia , lookup
Butyric acid wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Ribosomally synthesized and post-translationally modified peptides wikipedia , lookup
Nucleic acid analogue wikipedia , lookup
Point mutation wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Peptide synthesis wikipedia , lookup
Metalloprotein wikipedia , lookup
Protein structure prediction wikipedia , lookup
Proteolysis wikipedia , lookup
Citric acid cycle wikipedia , lookup
Genetic code wikipedia , lookup
Biochemistry wikipedia , lookup
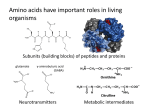
December 7-8, 2011 AMINO ACID METABOLISM I,II,III Lecturer: Eileen M. Lafer Reading: Stryer Edition 6: Chapters 23 and 24 OBJECTIVES: 1. Understand the fates and sources of the amino acids in general terms. 2. Understand the general features of lysosomal protein degradation, including what types of proteins are degraded in lysosomes. 3. Understand how "controlled proteolysis" is effected in cells. This includes an understanding of the mechanism of selection and attachment of ubiquitin to target proteins, as well as where and how ubiquitinated proteins are degraded. 4. Understand the common pathways for the removal of the a-amino group from an a-amino acid during amino acid catabolism. 5. Understand how the fate of the ammonium ions generated during amino acid degradation differs in the liver versus the peripheral tissues. 6. Understand the fundamentals of the urea cycle and how it is regulated. Understand how defective urea cycle enzymes can lead to disease, and how those diseases are treated. 7. Understand which a-amino acid carbon skeletons feed into which major metabolic intermediates during amino acid catabolism. 8. Know which amino acids are solely ketogenic, solely glucogenic, and both ketogenic and glucogenic. 9. Know which steps in amino acid degradation lead to the following diseases: methyl-malonic acedemia, homocystinuria, maple syrup disease, phenylketonuria, tyrosinemia I, II and III, and alkaptonuria. For each disease, you should know the name of the defective enzyme, the reaction catalyzed by the enzyme, and the pathway in which the enzyme functions. 10. Know which amino acids are essential and which are non-essential in humans. 11. Know in humans, which major metabolic intermediates are able to serve as carbon skeletons for the biosynthesis of which amino acids. 12. Know which amino acids can act as neurotransmitters. 13. Know which amino acids can be used for the synthesis of which neurotransmitters. 14. Understand in general terms the biosynthesis of spermine, spermidine, creatine and phosphocreatine. Reminder: to download movies used in my lectures go to my web page: http://www.biochem.uthscsa.edu/~lafer/ (aleternativly go to uthscsa biochem dept., click on faculty, etc. to find above link) Click on links, for a mirror of the ppt files on blackboard, as well as the movie files that are not permitted on blackboard due to size limitations. SOURCES AND FATES OF AMINO ACIDS IN THE BODY PROTEIN CATABOLISM Proteolysis of dietary proteins in the stomach and lumen of the small intestine releases free amino acids into the bloodstream. Proteolysis of proteins that move through the endocytic pathway takes place in the lysosomes of all cells. Controlled proteolysis of ubiquitin-tagged intracellular proteins takes place in the proteasomes of all cells. AMINO ACID POOL LYSOSOMAL DEGRADATION 1. Lysosomes degrade proteins taken up by endocytosis, or proteins that traffic within the endocytic pathway. 2. Lysosomes contain ~50 hydrolytic enzymes (proteases). Their pH optima is acidic. 3. The pH of the lysosome is ~5. 4. In well-nourished cells, lysosomal protein degradation is non-selective. 5. In starving cells, there is a selective pathway that preferentially degrades cytosolic proteins containing the pentapeptide KFERQ (Lys-Phe-Glu-Arg-Gln). CONTROLLED PROTEOLYSIS 1. Ubiquitin tags proteins for destruction. 2. The proteasome digests the ubiquitin tagged proteins. 3. Protein degradation can be used to regulate biological function. UBIQUITIN The Mark of Death 76 aa polypeptide. C-terminal gly attaches to the e-amino groups of several lys on a protein destined for degradation. Additional ubiquitin molecules can be added to Lys48. UBIQUITIN CONJUGATION E1=Ubiquitin-Activating Enzyme E2=Ubiquitin-Conjugating Enzyme E3=Ubiquitin-Protein Ligase UBIQUITIN IS ATTACHED TO THE e-AMINO GROUP OF LYSINE RESIDUES ON TARGET PROTEINS CLINICAL CORRELATION: Human papilloma virus (HPV) encodes a protein that activates a specific E3 enzyme. The enzyme ubiquitinates the tumor suppressor p53 and other proteins that control DNA repair, which are then destroyed. The activation of this E3 enzyme is observed in more than 90% of all cervical carcinomas. A SINGLE UBIQUITIN MOLECULE IS A POOR SIGNAL FOR DEGRADATION. CHAINS OF 4 OR MORE UBIQUITIN MOLECULES ARE VERY STRONG SIGNALS FOR DEGRADATION. WHAT DETERMINES WHETHER A PROTEIN IS UBIQUITINATED? The substrate specificity of each E3. 1. The N-terminal rule: the chemical nature of the amino-terminal amino acid. For example, a protein with methionine at it s N terminus has a half life of 20 hours, while a protein with an arginine at its N-terminus has a half life of 2 minutes. 2. Cyclin destructive boxes: specific amino acid sequences that mark cell-cycle proteins for destruction. 3. PEST sequences: proteins rich in proline, glutamic acid, serine and threonine. THE 26S PROTEASOME DIGESTS THE UBIQUITIN TAGGED PROTEINS 19S regulatory subunit 20S proteasome (catalytic activity) 19S regulatory subunit The Executioner THE 20S PROTEASOME 1. 700kD, 28 homologous subunits: 14 of type a and 14 of type b. 2. Subunits are arranged in 4 rings of 7 subunits each to form a sealed barrel. 7 7 7 7 PROTEOLYTIC ACTIVITY RESIDES IN THE N-TERMINALTHREONINE RESIDUES OF THE BETA SUBUNITS 7 7 7 7 ACCESS TO THE 20S PROTEASOME IS CONTROLLED BY THE 19S CAPS The 19S regulatory subunits bind to polyubiquitin chains. SOURCES AND FATES OF AMINO ACIDS IN THE BODY PROTEIN DEGRADATION CAN REGULATE BIOLOGICAL PROCESSES Dynamically alter the stablity of regulatory proteins. SOURCES AND FATES OF AMINO ACIDS IN THE BODY AMINO ACID DEGRADATION 1. Any amino acids generated by protein catabolism that are not needed as building blocks for new biomolecular synthetic reactions are degraded to carbon skeletons in the liver. 2. The first step in amino acid degradation is the removal of nitrogen. a-AMINO GROUPS ARE CONVERTED INTO AMMONIUM IONS BY OXIDATIVE DEAMINATION OF GLUTAMATE The a-amino group of the a-amino acid is transferred to a-ketoglutarate to form glutamate, which is oxidatively deaminated to yield ammonium ion. 1. THE TRANSAMINATION REACTION: Aminotransferases (also called transaminases) catalyze the transfer of an a-amino group from an a-amino acid to an a-keto acid. These enzymes generally utilize a-ketoglutarate as the acceptor. The enzymes are named after their amino acid substrates, i.e. aspartate transaminase catalyzes the transfer of the a-amino group of aspartate to aketoglutarate, yielding oxaloacetate plus glutamate. 2. THE OXIDATIVE DEAMINATION REACTION: The nitrogen atom that is transferred to a-ketoglutarate in the transamination reaction is converted into free ammonium ion by oxidative deamination. This reaction is catalyzed by glutamate dehydrogenase. This reaction takes place in the mitochondria, and is driven by the consumption of ammonia. Dehydrogenation Hydrolysis The sum of the aminotransferase and glutamate dehydrogenase reactions yield ammonium ion: aminotransferase AMINO ACID 1 ALPHA KETOACID 1 dehydrogenase urea cycle ALPHA KETOACID 2 AMINO ACID 2 excreted ALL AMINOTRANSFERASES CONTAIN THE PROSTHETIC GROUP PYRIDOXAL PHOSPHATE (PLP) PLP is derived from Pyridoxine (Vitamin B6) PLP TAUTOMERS: The phenolic hydroxyl group is slightly acidic, favoring deprotonation. The pyridine ring is slightly basic, which favors protonation of the pyrimidine N. PHENOLATE PLP FORMS SCHIFF BASE INTERMEDIATES IN AMINOTRANSFERASES AMINO ACID 1 (schiff-base linkage with the enzyme) (schiff-base linkage with the substrate) The positively charged schiff-base linkages are stabilized by the negatively charged phenolate group. TRANSAMINATION MECHANISM 1. The schiff base loses a proton from the a-carbon of the amino acid to become a quinonoid intermediate. 2. Reprontonation of the quinonoid at the aldehyde carbon yields a ketimine intermediate. 3. The ketimine is then hydrolyzed to an a-ketoacid and PMP. ALPHA KETOACID 1 1 2 3 ONCE THE AMINO GROUP HAS BEEN TRANSFERRED TO PMP, PMP TRANSFERS THE AMINO GROUP TO ANOTHER ALPHA-KETOACID BY REVERSING THE REACTION SCHEME WE JUST DISCUSSED (FOLLOW THE RED ARROWS): ALPHA KETOACID 2 (ALPHA KETOGLUTARATE) 3 2 4 AMINO ACID 2 (GLUTAMATE) 1 The sum of the aminotransferase and glutamate dehydrogenase reactions yield ammonium ion: aminotransferase AMINO ACID 1 ALPHA KETOACID 1 dehydrogenase urea cycle ALPHA KETOACID 2 AMINO ACID 2 excreted ASPARTATE AMINOTRANSFERASE Active site Arg386 helps orient substrates by binding to their a-carboxylate groups. PLP is bound to active site Lys268 by a Schiff-base linkage. MECHANISM OF THE AMINOTRANSFERASE REACTION: MOVIE: Movie file 18-01.avi The sum of the aminotransferase and glutamate dehydrogenase reactions yield ammonium ion: aminotransferase AMINO ACID 1 ALPHA KETOACID 1 dehydrogenase urea cycle ALPHA KETOACID 2 AMINO ACID 2 excreted • End of First Lecture SERINE AND THREONINE CAN BE DIRECTLY DEAMINATED 1. The nitrogen atoms of MOST amino acids are transferred to aketoglutarate. 2. The a-amino groups of serine and threonine can be directly converted into ammonium ion by the action of dehydratases. Threonine a-ketobutyrate + NH4+ PERIPHERAL TISSUES TRANSPORT NITROGEN TO THE LIVER BY THE ALANINE CYCLE OR AS GLUTAMINE If amino acids are produced in tissues that lack the urea cycle, they need a mechanism to release nitrogen in a form that can be absorbed by the liver and converted into urea. EXAMPLE: Muscle uses amino acids as fuel during prolonged exercise and fasting. THE ALANINE CYCLE 1. In peripheral tissues,the a-amino groups of the amino acids are transferred to glutamate by a transamination reaction, as in the liver. 2. However, rather than oxidatively deaminating glutamate to form ammonium ion, the a-amino group is transferred to pyruvate to form alanine. 3. The liver takes up the alanine, and converts it back to pyruvate by another transamination reaction. 4. The pyruvate can be used for gluconeogenesis, and the amino group eventually ends up as urea by the usual pathway. a-ketoglutarate pyruvate a-ketoglutarate glutamate NITROGEN CAN ALSO BE TRANSPORTED AS GLUTAMINE Glutamine Synthetase: NH4+ + glutamate + ATP glutamine + ADP + Pi Once glutamine is in the liver, it can be metabolized like any other amino acid and the nitrogen can end up in the urea cycle. SOURCES AND FATES OF AMINO ACIDS IN THE BODY IN LIVER THE AMMONIUM IONS GENERATED DURING AMINO ACID DEGRADATION FEED INTO THE UREA CYCLE Urea cycle: importance • NH4+ is a product of the breakdown of amino acids. • NH4+ is required by cells for synthesis of nitrogencontaining compounds. • Excess NH4+ is very toxic. Normal levels in human blood are: [NH4+] < 70 M. • Excess NH4+ is converted to urea via the urea cycle and excreted. The urea cycle accounts of ~80% of the excreted nitrogen. Urea cycle: location and source of atoms • Urea synthesis takes place mostly in the liver. • One N atom of urea comes from Asp (blue). • One N atom comes from NH4+ (green). • One C atom comes from CO2 (red). • Ornithine acts as a carrier of various atoms in the process of synthesizing urea. Urea cycle reactions: carbamoyl phosphate synthetase • Catalyzes formation of carbamoyl phosphate from H2O, 2 ATPs, CO2 and NH3. • The positive heterotropic activator, Nacetylglutamate, is required for activity. • Brings one C atom and one N atom into the urea cycle as a carbamoyl group. • Catalyzes the critical step in removing NH4+ from the blood. Urea cycle reactions: carbamoyl phosphate synthetase • The reaction is made irreversible by cleaving two ATP molecules to two ADP. • One molecule of phosphate is released while the second phosphate ends up as part of carbamoyl phosphate. Urea cycle reactions: carbamoyl phosphate synthetase • Carbamoyl phosphate synthetase is present at very high concentration in the mitochondrial matrix (~1 mM). • The high enzyme concentration allows the enzyme to work well below the Km ~ 250 M for NH4+. • By operating well below Km, a small increase in NH4+ leads to a large increase in the rate of removal of NH4+ insuring that NH4+ remains low. Urea cycle reactions: ornithine transcarbamoylase • Catalyzes the formation of citrulline and Pi from ornithine and carbamoyl phosphate. • Transfer of a carbamoyl group to ornithine is facilitated by rupture of a high energy phosphoanhydride bond. • Catalyzes introduction of one C atom and one N atom into the urea cycle from carbamoyl phosphate. Urea cycle reactions: argininosuccinate synthetase • Catalyzes condensation of citrulline and aspartate to form argininosuccinate. • Catalyzes the introduction of one N atom into the urea cycle from aspartate. Urea cycle reactions: argininosuccinase • Cleaves argininosuccinate to arginine and fumarate. • Completes the transfer of the amino group from aspartate to make arginine. • Retains the carbon skeleton of aspartate (as a fumarate molecule). Urea cycle reactions: arginase • Catalyzes hydrolysis of arginine to ornithine and urea. • Ornithine “cycles” back to the first step and picks up another carbamoyl group from carbamoyl phosphate. Urea cycle: overall reaction • PPi 2 Pi quickly in a reaction catalyzed by pyrophosphotase. • Overall, four high energy phosphate bonds are broken to synthesize each molecule of urea. Urea cycle and the citric acid cycle General amino acid catabolism • Fumarate production connects the urea cycle and the citric acid cycle (fumarate malate oxaloacetate). • In the citric acid cycle fumarate is converted to oxaloacetate. • Oxaloacetate is transaminated to aspartate. • Aspartate carries the amino groups of other amino acids into the urea cycle. Compartmentalization of the urea cycle • Takes place in the liver. • Two intracellular locations. • Mitochondrial matrix: carbamoyl phosphate formation and citrulline synthesis. • Cytosol: argininosuccinate formation; cleavage of argininosuccinate to arginine and fumarate; hydrolysis of arginine to ornithine and urea. Regulation of the urea cycle • The urea cycle removes excess NH4+ which comes from the breakdown of amino acids. • Overall control of the urea cycle is by enzyme levels, which change by as much as ten-fold depending on the diet. • The flow of compounds through the urea cycle also depends on the concentrations of cycle intermediates. • Several reactions convert amino acids into urea cycle intermediates. • Arginine from the diet can be converted to ornithine. • Glutamate can be converted to ornithine by intestinal enzymes. Regulation of the urea cycle • Fine control of the urea cycle is through regulation of carbamoyl phosphate synthetase. • N-acetylglutamate is a heterotropic allosteric activator of carbamoyl phosphate synthetase. (Heterotropic means an effector molecule that is different from the substrate.) Regulation of the urea cycle • N-acetylglutamate acts as a signal for high amino acid concentrations. • N-acetylglutamate is synthesized in the liver from acetylCoA and glutamate in a reaction catalyzed by Nacetylglutamate synthetase. Regulation of the urea cycle • The steady state concentration of N-acetylglutamate is determined by two factors. • Concentrations of substrates: acetyl CoA and glutamate. • Concentration of arginine, which activates Nacetylglutamate synthetase. Defective urea cycle enzymes and inherited disease • High NH4+ is toxic and a complete lack of any urea cycle enzyme is fatal. • Some diseases are believed to be due to partially active defective enzymes. • Defective enzymes cause high levels of NH4+ in the blood. • Sometimes a low protein diet can help. The diet decreases the amount of NH4+ that needs to be eliminated through the urea cycle. Defective enzymes and treatment • Problem: argininosuccinase deficiency. • Treatment: a low protein diet high in arginine. NOTE THIS IS THE PRODUCT OF THE DEFECTIVE ENZYME • Result: argininosuccinate is secreted in place of urea to remove ammonium ions that are generated during amino acid catabolism. X Defective enzymes and treatment • Problem: carbamoyl phosphate synthetase or ornithine transcarbamoylase deficiency. • Result: glycine and glutamine build up (pyruvate and glutamate accept amino groups from ammonium ions). Defective enzymes and treatment • Treatment: feed benzoate to remove Gly as hippurate. • Treatment: feed phenylacetate to remove Gln as phenylacetylglutamine. + NH4 toxicity and excess glutamine • NH4+ toxicity may be due to formation of excess glutamine. • High glutamine levels are found in the cerebrospinal fluid of those with high NH4+. • High glutamine and glutamate may lead to brain damage, possibly by producing osmotic effects that cause brain swelling. Urea cycle: overall reaction • PPi 2 Pi quickly in a reaction catalyzed by pyrophosphotase. • Overall, four high energy phosphate bonds are broken to synthesize each molecule of urea. END OF LECTURE 2 SOURCES AND FATES OF AMINO ACIDS IN THE BODY FATES OF THE CARBON SKELETONS OF THE AMINO ACIDS All 20 amino acids funnel into only 7 major metabolic intermediates. 1. The strategy of amino acid degradation is to transform the carbon skeletons into major metabolic intermediates that can be converted into glucose, or oxidized by the citric acid cycle. 2. The carbon skeletons of a diverse set of 20 amino acids are funneled into only 7 molecules: pyruvate, acetyl CoA, acetoacetyl CoA, a-ketoglutarate, succinyl CoA, fumarate and oxaloacetate. PYRUVATE AS AN ENTRY POINT INTO METABOLISM 3-carbon amino acids ala, ser, cys enter via pyruvate. OXALOACETATE AS AN ENTRY POINT INTO METABOLISM The skeletons of 4-carbon amino acids enter at oxaloacetate. a-KETOGLUTARATE AS AN ENTRY POINT INTO METABOLISM The skeletons of several 5-carbon amino acids enter the TCA cycle at a-ketoglutarate. All first transfer their amino groups to glutamate, which is then oxidatively deaminated by glutamate dehydrogenase to yield a-ketoglutarate. SUCCINYL COENZYME A AS AN ENTRY POINT INTO METABOLISM FOR SEVERAL NON-POLAR AMINO ACIDS Threonine (in humans) CLINICAL CORRELATION: methyl-malonic acedemia methylmalonylCoA mutase is defective CLINICAL CORRELATION: homocystinuria Scoliosis, muscle weakness, mental retardation, thin blond hair cystathione b-synthase is defective Glucogenic Amino Acids: amino acids (aa) that are converted to metabolites that can be converted to glucose. TCA cycle intermediates and pyruvate can be converted to phosphoenolpyruvate and then glucose. Ketogenic Amino Acids: aa that give rise to ketone bodies or fatty acids. Only leucine and lysine are solely ketogenic. Isoleucine,phenylalanine, tryptophan and tyrosine are both ketogenic and glucogenic. Remaining 14 amino acids are solely glucogenic. WHEN THE BRANCHED CHAIN AMINO ACIDS VALINE, ISOLEUCINE, AND LEUCINE ARE DEGRADED IN EXTRA-HEPATIC TISSUES THEY SHARE TWO COMMON ENZYMES: branched-chain aminotransferase branched-chain a-ketoacid dehydrogenase complex While much of the catabolism of amino acids takes place in the liver, the branched chain amino acids are oxidized as primary fuels in muscle, adipose, kidney, and brain tissues. CLINICAL CORRELATION: maple syrup disease; Defective branched-chain a-keto acid dehydrogenase complex; urine has odor of maple syrup, mental and physical retardation UNLESS patients are placed on a diet low in valine, isoleucine and leucine early in life. OXYGENASES ARE REQUIRED FOR THE DEGRADATION OF AROMATIC AMINO ACIDS Monooxygenase- one atom of O2 appears in the product and one in H20. CLINICAL CORRELATION: MUTATIONS IN THE GENE ENCODING PHENYLALANINE HYDROXYLASE CAUSE PHENYLKETONURIA More than 200 mutations have been identified. Mutations effecting the active site, the biopterin binding site, and other regions of the protein are indicated as colored spheres. AROMATIC AMINO ACID METABOLISM Clinical Correlation: Phenylketonuria-phenylalanine accumulates in body fluids, if untreated, severe mental retardation. Treatment-low phenylalanine diet. Tyrosinemias-if untreated, weakness, self-mutilation, liver damage, mental retardation. Treatment? Alkaptonuriahomogentisate accumulates in the urine, and is excreted, which turns dark on standing due to the oxidation of homogentisate. Harmless. TRYPTOPHAN DEGRADATION Nearly all cleavages of aromatic rings in biological systems are catalyzed by dioxygenases. SUMMARY OF DEFECTS IN AMINO ACID CATABOLISM THAT CONTRIBUTE TO HUMAN DISEASE FATES OF THE CARBON SKELETONS OF THE AMINO ACIDS SOURCES AND FATES OF AMINO ACIDS IN THE BODY AMINO ACID BIOSYNTHESIS 1. The nitrogen in amino acids, purines, pyrimidines and other biomolecules ultimately comes from atmospheric N2. 2. This process begins with the reduction of N2 to NH3. This process is called NITROGEN FIXATION, and is carried out by some bacteria. 3. Since nitrogen fixation does not take place in higher organisms, the source of nitrogen for amino acid biosynthesis in humans are the metabolites of dietary nitrogen. AMINO ACIDS ARE MADE FROM METABOLITES OF THE MAJOR METABOLIC PATHWAYS MOST MICROORGANISMS CAN SYNTHESIZE ALL 20 AMINO ACIDS HUMANS CAN ONLY SYNTHESIZE 11 AMINO ACIDS The essential amino acids cannot be made by humans and must be obtained in the diet. 1. The synthesis of many of the amino acids is a simple reversal of their degradation, utilizing a transamination reaction. 2. Amino acids skeletons end up as major metabolic intermediates during degradation. Likewise, amino acids are also biosynthesized from major metabolic intermediates. SOURCES AND FATES OF AMINO ACIDS IN THE BODY BIOSYNTHETIC FATES OF THE AMINO ACIDS: 1. Protein synthesis (Dr. Lee) 2. Nucleic acid synthesis (Dr. Lee) 3. Heme synthesis (Dr. Luduena) 4. Thyroid hormone synthesis (Dr. Adamo) 5. Neurotransmitter synthesis 6. Spermine and spermidine 7. Creatine and phosphocreatine Several amino acids can function as neurotransmitters without any chemical modification: Glutamate Glycine Aspartate MOST OF THE SMALL-MOLECULE NEUROTRANSMITTERS ARE AMINO ACIDS OR THEIR DERIVATIVES * Tyrosine Tyrosine Tyrosine Glutamate Tryptophan Histidine * (not directly from an amino acid, from acetyl CoA + choline) CATHECHOLAMINE BIOSYNTHESIS GABA BIOSYNTHESIS HISTAMINE BIOSYNTHESIS SEROTONIN BIOSYNTHESIS BIOSYNTHESIS OF SPERMINE AND SPERMIDINE BIOSYNTHESIS OF CREATINE AND PHOSPHOCREATINE BIOSYNTHETIC FATES OF THE AMINO ACIDS: 1. Protein synthesis 2. Nucleic acid synthesis 3. Heme synthesis 4. Thyroid hormone synthesis 5. Neurotransmitter synthesis 6. Spermine and spermidine 7. Creatine and phosphocreatine SOURCES AND FATES OF AMINO ACIDS IN THE BODY