* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Nicotinic Acetylcholine Receptor
Pharmaceutical industry wikipedia , lookup
CCR5 receptor antagonist wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug design wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Drug interaction wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
NMDA receptor wikipedia , lookup
Toxicodynamics wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Psychopharmacology wikipedia , lookup
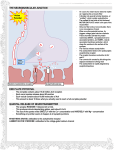
Nicotinic Acetylcholine Receptor The electrostatic isopotential surface--a surface representing constant electric potential--for a model of the nicotinic acetylcholine receptor. Some members of this family of receptors in the brain bind nicotine and are targets for the addictive activity of this drug. The receptor is composed of five subunits with similar amino acid sequences encircling a central channel. Neurotransmitters such as acetylcholine bind at two of the five subunit interfaces, gating, or opening, the channel to allow sodium ions to enter from outside the cell. The red surface corresponds to the isopotential contour -1 kT/e, where k is the Boltzmann constant, T is temperature, and e is electronic charge. The contour shows the electrostatic influence on the binding of acetylcholine. The model was developed by Igor Tsigelny, Naoya Sugiyama, and Palmer Taylor at the Departments of Pharmacology and Chemistry/Biochemistry at the University of California, San Diego, in collaboration with Steven M. Sine at the Mayo Foundation in Rochester, Minnesota. Visualized by Igor Tsigelny at SDSC. MEDICINAL CHEMISTRY Pharmaceutical Sciences 621& Chemistry 569 Professor C. M. Thompson (x4643) mailto:%[email protected] Lecture 8 DRUGS ACTING ON NEUROTRANSMITTERS AND THEIR RECEPTORS - ACETYLCHOLINE AND DOPAMINE (in part) ACETYLCHOLINE A. Acetylcholine and Cholinergic Receptors. The cholinergic system is found in the central nervous system (CNS), in the autonomic nervous system and the skeletomotor system. Acetylcholine (ACh) is the neurotransmitter of interest: CH3C(O)OCH2CH2N+(CH3)3 Cholinergic receptors show duality and have sites of differing binding properties: "nicotinic" and "muscarinic." Acetylcholine bind to both types! Nicotine Receptor: binds nicotine and are found in all autonomic ganglia and at the neuromuscular endplate of striated muscle. Muscarinic Receptor: bind muscarine and occur at post-ganglionic parasympathetic terminals -> control peristalsis, glandular secretion, pupil constriction, vasodilation and heart rate reduction. Amanita muscaria mushroom. Euripedes lost his wife and 3 children to poisoning by this mushroom. Also contains amanatins (octapeptides) which cause death by inhibition of RNA polymerase leading to renal or hepatic failure (nitrogen should bear a positive charge). The degeneration of cholinergic pathways in the CNS results in "neuronal tangles" -> neuron arrangement messed up. This process is hypothesized to be a major contributor to Alzheimer's disease (not the same as senile dementia), a premature and progressive memory loss. Drug treatment with choline replacement, cholinergic agonists have shown marginal success. A.1. Acetylcholine Metabolism As ACh is synthesized, it is stored in the neuron "depot" (a.k.a. vesicles) and is released by neuronal stimulation, which occurs by K+ depolarization (below). Although the cholinesterase is shown "floating" in the synapse (for effect), it is actually a membrane bound protein. Acetylcholine release is inhibited by botulinus toxin (LD50 = 1 ng / Kg; or 7 x 108 g to kill a 70 kg person). Produces muscle paralysis by blocking the active zone of the presynaptic membrane. A protein exists that fuses the vesicle to the membrane, anchoring it to release ACh. Botulism toxin binds this protein and the vesicle can not get to the edge to release the ACh. A.2. Nicotinic Acetylcholine Receptor. The receptor was isolated with the help of the electric eel and electric ray, which have a copious concentration of these receptors; much higher than the human brain. specie ray eel human ACh-R conc. 1000 nmol/kg tissue 50-100 nmol/kg tissue brain 0.1-1.0 nol/kg tissue Electric ray can give a shock of 50-60 volts and an eel up to 600 volts and 1 kilowatt energy. At any rate, these receptor rich tissues were isolated with the help of the Siamese cobra. The venom of certain snakes contain peptides called bungarotoxin (peptide of about 61-75 amino acids containing lots of arginines and lysines cationic amine residues). They block cholinergic neurotransmission by direct binding to the receptor. Can you now think of how they used the snake to trap the eel [receptor]? Sure you can? A.3. Muscarinic Acetylcholine Receptor. Far more stereospecific and structure specific than the nicotinic receptor. In fact, only as recently as 1980 have scientists studied the differences between nicotine and muscarinic receptors. As a result, the structure, biochemistry, and operation of the muscarinic receptor is still vague; especially since there are no organs "rich" in this particular receptor. Two subtypes of receptor, M1 and M2 have been identified: M1: closes K+ channels M2: located in heart muscle, cerebellum and hindbrain and is regulated by GTP. That is, a second messenger is usually interactive with the M2. The breakthrough came when an agonist called pirenazepine, was found that selectively binds, or rather has a high affinity for the M1. A.4. Cholinergic Agonists. You can generally increase stimulation of the ACh-receptor two ways: 1. by direct binding of an agonist to the receptor - direct acting. 2. by inhibition of acetylcholinesterase (AChE), prolonging the agonist action because the protein responsible for its breakdown is rendered inactive. It is called - indirect acting. A.4.a. Design of Modification of Acetylcholine. Cholinergic Agonists: Structural 1. Ammonium Group. The replacement of the ammonium moiety with either a sulfonium or phosphonium results in a complete loss of activity. Increasing one methyl group to a larger alkyl (e.g., ethyl) results in 25% activity. Increase two methyl groups in size -> lose all activity. Replacement of ammonium group with tert-butyl retains 0.003% of activity. Implies that the charge distribution and size are important factors to ACh-R action. 2. Ethylene bridge. Acts as a "perfect spacer" or ruler between the carbonyl and the quaternary ammonium moiety and ensures the proper distance for receptor binding. Rule of Five: Should be no more than four atoms between the ammonium and the terminal methyl group, otherwise a loss of activity. Branching on the ethylene bridge tolerates methyl only. 3. Ester Group. Not very amenable to modification and a change from a methyl to a phenyl makes a good antagonist! Some activity can be maintained by replacement with a ketone/ether and carbamate (carbachol). 4. Cyclic analogs. Many have good activity including muscarine itself. The acetoxy cyclopropyls were used to probe the receptor. Trans isomer had same effect as muscarine. A.5. Mode of Cholinergic Binding. ACh is very flexible. Two major conformations. Eclipsed not considered but could be a possible contributor once inside the receptor. Gauche conformer = muscarinic Anti conformer = nicotinic It is generally accepted that the ammonium group binds a carboxylate (glutamate or aspartate) aided by van der Waals interactions of a hydrophobic pocket. Approximately 5.9 Å away a hydrogen donor forms a H-bond with the carbonyl. Some speculation over the acetoxy-methyl binding a smaller pocket also has been forwarded. Requirements for nicotinic and muscarinic receptors are similar except the muscarinic has a methyl group to complement a pocket and the nicotinic a carbonyl group. Recheck the two structures. A.5.a. Cholinergic Blocking Agents. Drugs that inhibit the interaction of ACh with its receptor are called "cholinergic blocking agents." [Note: peripheral cholinergic synapses are muscarinic.] Anticholinergic agents decrease the secretion of saliva (dry-mouth) and gastric juice, decrease G.I and urinary peristalsis and pupil dilation. Some are used in the treatment of peptic ulcer, ophthalmology and Parkinson's disease. Some of the oldest anti-cholinergics are the "belladonna alkaloids" also known as deadly nightshade, which has excitatory and hallucinogenic effects. Story time: Belladonna was used by the ancient Hindu's, Roman Empire and the Middle Ages to induce prolonged poisoning. Much of the poison uses were quite fun to the poisoner, watching the victim fall to memory loss, disorientation, destruction of mental faculties prior to death. Thus, they could be viewed as possessed by demons! Hippocrates indicated its use in the treatment of gastric disturbances. Belladonna gets its name (Atropa belladonna) from Carolus Linnaeus, the founder of modern botanical nomenclature, who named it after Atropos, the oldest of the Three Fates, who was said to cut the thread of life after her sisters had spun and measured it. Belladonna (translation anyone?) contains atropine and scopolamine, the major active ingredients found in the "witches brew." They are esters of tertiary amines with a bulky ester component and are mixed M1 and M2 antagonists. [NOTE: the amine group is protonated at physiological pH.] Fit to the receptor is good and the phenyl moiety "bends out" to possibly block incoming ACh to displace it. Atropine. 10 mg can kill a child. The diagnosis: widespread paralysis, convulsions, circulatory collapse, blood pressure drop, inadequate respiration and coma. Scopolamine: truth serum and sleep inducer Cocaine: note only the similarity in structure to these other two alkaloids. We are all pretty familiar with the effects of cocaine - note that atropine and scopalamine are down regulating drugs (sleep, blood pressure lowering, etc.) whereas cocaine is an up regulating stimulant. What is the basic difference in the structures - STEREOCHEMISTRY! A.5.b. Ganglionic Blocking Agents. interfere with nicotinic ACh receptors. Usually simple ammonium groups. Used in the control of hypertension by decreasing vasoconstriction. Et4N+ Me3N+ + (CH2)6 NMe3 Because they have no "second" binding interaction, they are non-specific and have many side effects. They also fit so "loosely" that they are in/out of the receptor rapidly. Basically abandoned. A.5.b.2. Neuromuscular Blocking Agents. Widely used in surgery because they can help relax abdominal muscles without the use of deep (and risky) anesthesia. Two classes of these agents exist. 1. Competitive Agents. Curare (tubocurarine: active ingredient): known as the arrow poison of South American Indian. Competitive agents are usually bulky rigid molecules with an optimum distance of 10 +/- 0.1 Å. Tubocurarine: intra-ammonium distance 10.3 Å by x-ray. Story Time Again!Curare has a long and romantic history. Used primarily for killing wild animals, it is a generic term for arrow poisons, the most widely used is tubocurarine. Studied as early as 1805, it was brought to the attention of medical practitioners between 1932-1940 in Europe, when it was used to treat specific disorders and tetanus (lockjaw: can't move muscle) to relax muscles at a very low concentration. Biomechanistically, curare combines with the cholinergic receptor sites at the post-junctional membrane (surface) and thereby, competitively blocks the transmitter action of ACh. The receptor becomes "insensitive" to ACh and thus, the motor nerve impulse and the endplate potential (K+ flux) falls dramatically. However, and this is a big "however," the end-plate region of the remainder of the muscle fiber retains their normal sensitivity to K+ and the muscle fiber still responds to direct electrical stimulation. In summary, you are unable to move your muscles but you still very much feel the pain. 2. Depolarizing Agents. flexible structures with free bond rotation. They were devised (not natural products) through mimicry of the N+ - N+ distance, but they act by a different mechanism. Me3N+ (CH2)10+NMe3 decamethonium Me3N+ CH2CH2-OC(O)CH2CH2C(O)OCH2CH2+NMe3 succinylcholine These molecules bind normally to the ACh-receptor and triggers the same response as ACh - a brief contraction of the muscle - however, it is followed by a prolonged period of transmission blockage leading to muscular paralysis. Succinylcholine is far shorter lived than decamethonium because it is a substrate for acetylcholinesterase (AChE), the enzyme responsible for hydrolyzing esters in the neural synapse. For medical use, an anesthetic is coadministered. NOREPINEPHRINE AND THE ADRENERGIC RECEPTOR A. Adrenergic System: Also known as the sympathetic nervous system and is involved in homeostatic regulation, increased heart rate, cardiac contraction, blood pressure, bronchial airway tone, carbohydrate and fatty acid metabolism. Stimulation of the sympathetic nervous system normally occurs in response to physical activity, stress, allergic reactions, and provocation. In many cases the "adrenergic reaction" is opposite to cholinergic effects. There are two sub-systems: 1. Noradrenergic: controls behavior, mood and sleep 2. Adrenergic: uses epinephrine (a.k.a. adrenaline) as neurotransmitter. B. Biosynthesis of Catecholamine Neurotransmitters: Why the name catecholamines All come from tyrosine, an essential amino acid! A biosynthesis of catecholamines is presented: C. Adrenergic Drugs: Drugs acting at these neuron centers are called adrenergic drugs and may be separated into two types; presynaptic and post-synaptic effects. Pre-synaptic effects may be separated into the five following distinct categories, although we shall only discuss two types: 1. 2. 3. 4. 5. Drugs Drugs Drugs Drugs Drugs acting acting acting acting acting on on on on on catecholamine synthesis... catecholamine metabolism... catecholamine storage... catecholamine reuptake... presynaptic receptors... 1. Drugs acting on catecholamine synthesis... These are mostly enzyme inhibitors that interact/interfere with the steps shown on the previous page. One example is -methyldopa, which is a competitive inhibitor of dopa decarboxylase. 2. Drugs acting on catecholamine metabolism... Not discussed 3. Drugs acting on catecholamine storage... Probably the most important and most widely studied of these drugs is (+)-amphetamine. Understanding the mechanism of action of this drug allows for interpretation of an array of analogs. AMPHETAMINE: Amphetamine is used as a mood elevator, psychomotor stimulant and appetite suppressant. It has a multiple neuronal effect, inhibiting neurotransmitter uptake while increasing neurotransmitter (dopamine) release. It is a direct receptor agonist-the receptor in this case being a vesicle. If amphetamine is used continually to release dopamine, paranoid schizophrenia may occur (due to neurochemical imbalances and sleep disorders). So, how does amphetamine act on the norepinephrine neurons and [dopamine] receptors? It is worthy to note that both amphetamine and cocaine share this neurochemical system as their primary site of action, although different mechanisms account for their physiologic effects. First, compare the structure of amphetamine ("speed" "crank" "uppers") and methamphetamine ("meth" "crystal") to the actual neurotransmitters: Dopamine and norepinephrine are two major transmitters contained in the neurons that regulate emotional behavior. Thus, stimulants may act on this dopamine pathway by enhancing neuronal function by release of dopamine/norepinephrine from "storage vesicles" (similar to ACh). Due to the structural similarity, the illicit stimulants displace neurotransmitters from their storage sites. The neurotransmitters are therefore "pushed out" into the synaptic cleft where they stimulate receptors until the stimulant is metabolized or removed from the storage site. How much amphetamine can your neurons take? Unknown. Since this is a displacement reaction rather than an equilibrium, there is no precise dose - effect curve. Dangerous. A cartoon (loosely constructed) representing the effect is shown below. 4. Drugs acting on catecholamine reuptake... The principal mechanism for the deactivation of released catecholamines is not enzymic destruction (like the ACh - AChE system). Rather, "reuptake" of catecholamine into the nerve ending occurs. The presynaptic membrane contains an "amine pump" - an active transport system that moves the catecholamines from the membrane to the vesicles. Therefore, drugs may interact with the reuptake at several points in the process. For example; a. The drug can be taken up by the pump (mistaken for neurotransmitter) and transported to the storage site where it displaces the neurotransmitter. b. The drug can block the pump by binding to the membrane site where the pump is "attached." That is, the drug acts to prevent reuptake by clogging the holes. One drug that acts by mechanism b is cocaine. Cocaine acts by preventing dopamine from being reabsorbed. Thus, the neurotransmitter remains in the synaptic cleft where it continues to enervate the receptor long after the normal activation time has lapsed. Although this process is concentration dependent (dose-effect curve possible), this is only one site of action for cocaine, and ill effects come from a combination of processes.