* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download chapter17
Common cold wikipedia , lookup
Immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Innate immune system wikipedia , lookup
Adaptive immune system wikipedia , lookup
Anti-nuclear antibody wikipedia , lookup
Infection control wikipedia , lookup
Globalization and disease wikipedia , lookup
Molecular mimicry wikipedia , lookup
Herd immunity wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
DNA vaccination wikipedia , lookup
Vaccination policy wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Hepatitis B wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Smallpox vaccine wikipedia , lookup
Whooping cough wikipedia , lookup
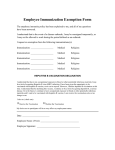
Applications of Immune Responses Chapter 17 Smallpox virus (or plague bacteria Smallpox [Yersina pestis]) has killed more people than any other infectious disease In the first half of the 1900s, smallpox was killing 4 million people worldwide each year In 1958, the Soviet Union proposed the global eradication of smallpox by using a concerted vaccination program Smallpox infects only humans, thus it could be eradicated The program was started in the late 1960s Representation of the Effects of Smallpox Vaccination 17.1 Principles of Immunizations Vaccines safely elicit an adaptive (T cell and B cell) immune response to pathogenic microbes In the process, they stimulate: High-affinity antibodies Class switching of antibodies (e.g., IgG, IgA) Memory T cells and B cells There are two types of vaccines Inactivated (all bacteria and some viruses) Attenuated-live (some viruses) 17.1 Principles of Immunizations 17.1 Principles of Immunizations 17.2 Vaccine and Immunization Procedures Attenuation Use of a similar virus that is non-pathogenic Vaccinia virus for smallpox Relies upon cross-reactive immunity Serial passage of pathogenic virus in cell culture or embyronated eggs Since cells and eggs have no immune system, mutant viruses arise that lose virulence These viruses often retain their antigenic determinants and thus elicit strong immunity 17.2 Vaccine and Immunization Procedures Inactivation Formalin (37% formaldehyde) Cross-links proteins and nucleic acids Used for toxoid (inactivated toxin) vaccines, such as tetanus β-propiolactone (BPL) Nucleic acid mutagen Breaks down rapidly After 24 hours, virtually none exists in a vaccine preparation 17.2 Vaccine and Immunization Procedures Inactivated vaccines Whole-agent: entire microbe is in the vaccine (inactivated poliovirus) Toxoid: No cells, just their toxin(s) (tetanus) Protein subunit vaccine: Only antigenic subunits (acellular pertussis, hepatitis B) Polysaccharide conjugate vaccines By conjugating (covalently-linking) polysaccharide antigens to proteins, the antigen becomes T-dependent Haemophilus influenzae type b (Hib) and Streptococcus pneumonia Requires an adjuvant (e.g aluminum hydroxide) to stimulate the innate immune response 17.2 Vaccine and Immunization Procedures Advantages/Disadvantages of Attenuation Advantages Disadvantages Stronger antibody response More expensive Requires fewer boosters Perishable (live viruses); requires refrigeration Longer memory Pathogenic revertants (rare) Stimulates MHC I processing (cytotoxic T cells) Possible contamination with other viruses More closely resembles natural infection 17.2 Vaccine and Immunization Procedures Advantages/Disadvantages of Inactivation Advantages Disadvantages Less Expensive Weaker antibody response Stable (room temp storage) Requires mre boosters No chance of infection Shorter memory Contaminating viruses will also be inactivated Does not stimulate MHC I processing (no Tc cells) Does not resemble natural infection 17.2 Vaccine and Immunization Procedures The importance of routine immunization in children Prior to the use of routine immunization, thousands of children died or were disabled by infectious diseases in the U. S. Globally, measles still kills 700,000 people, mostly children, per year By immunizing, the incidence of the disease, and consequently the microbe, decrease substantially For each infectious disease, a target vaccine coverage rate is needed to reduce the incidence of disease to nearly zero For measles, this rate is 95% 17.2 Vaccine and Immunization Procedures Vaccine side effects Risk The risk of vaccination is not zero But the risk of not vaccinating is far greater Those who do not immunize their children take advantage of those who do assume the risks Vaccines and autism spectrum disorders Large-scale population studies have shown that the incidence of autism spectrum disorders in vaccinated and unvaccinated populations is virtually the same 17.2 Vaccine and Immunization Procedures Japan’s experience with pertussis (whooping cough) 1972: Mandatory vaccination at 3 months reduces the incidence of pertussis to fewer than 300 cases per year 1973-74: Two children die shortly after vaccination 1974: Politicians change the first vaccination age to 2 years (instead of 3 months) 1979: Japan reports more than 13,000 cases of pertussis with 41 deaths. Some surviving have permanent neurological damage (which is what pertussis toxins do) 1980: Japan returns to their previous vaccine schedule and within a few years the incidence of pertussis returns to 1972 levels Vaccines are often victims of their own success 17.3 Principles of Immunologic Testing Antibodies are generated in response to infection The presence of antibodies in the blood (serum) to a pathogen are highly suggestive of infection Detection of IgM indicates recent infection Detection of IgG indicates recent or distant infection The study of blood antibodies is serology 17.3 Principles of Immunologic Testing Blood collection Collect blood without anticoagulants Allow to stand at room temp 30 min for clot formation, then at 4° C for 1 hour for contraction Centrifuge the blood to separate clot from serum Aspirate the serum into a new tube Dilute for testing (usually 1:20 for IgM or 1:100 for IgG testing) 17.3 Principles of Immunologic Testing Serological tests Agglutination (e.g. influenza typing) Precipitation Immunofluorescence Enzyme-linked immunosorbant assay (ELISA) Western blot 17.5 Using Labeled Antibodies to Detect Antigen-Antibody Interactions ELISA Antigen: Coat known protein antigen to a solid-surface Polyvinyl chloride (PVC) is commonly used because it has a high affinity for proteins Serum sample: Add patient’s serum and incubate 1 hour If antibodies to the antigen are present, they will bind to the antigen coated on the plate Detection antibody: Wash with saline, then add an enzymeconjugated anti-human IgG antibody If the patient has antibodies, they will be bound by the detection antibody Substrate: Wash with saline, then add substrate that turns color in the presence of the enzyme