* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download The complement system
Drosophila melanogaster wikipedia , lookup
Monoclonal antibody wikipedia , lookup
DNA vaccination wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Immune system wikipedia , lookup
Adaptive immune system wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Molecular mimicry wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Biochemical cascade wikipedia , lookup
Innate immune system wikipedia , lookup
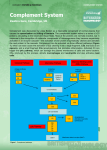
Polyclonal B cell response wikipedia , lookup
The complement system, antigens Martin Liška The complement system • A complex consisting of at least 20 serum proteins, which, once activated, acts like a part of the innate immune defense • The complement components are present in serum in inactive form • The complement is activated in a cascading manner (= each protein activates that following) and it has widespread physiologic and pathophysiologic effects • Complement proteins are synthesized mainly in the liver, but tissue macrophages and fibroblasts can synthesize some complement proteins as well The complement system nomenclature • • • • C1q, C1r, C1s, C2-9 Factor B, Factor D Properdin Regulatory proteins (C1-inhibitor, Factor I, C4bBP, Factor H, S protein, anaphylatoxin inactivator) The classical pathway of complement activation • The pathway is activated through antigenantibody complexes: initially, C1 component binds to a site on the Fc fragment of Ig (IgG (but not IgG4) or IgM); however, native Ig molecules do not interact with C1 • C1 component – contains three polypeptides (C1q, C1r, C1s); C1q attaches first to Ig (for initiation of complement activation, C1q has to interact with two or more Ig monomers) → C1q activates proenzyme C1r → C1r cleaves proenzyme C1s → C1s is able to cleave C4 component The classical pathway of complement activation • Activated C1s cleaves C4 to C4a (an anaphylatoxin) + C4b → C4b binds to cell membranes → the next component becomes susceptible to enzymatic attack by activated C1 • C4b + C2 + C1s → removal of C2a → enzymatically active molecular complex C4b2b (= C3 convertase of the classical pathway) • Formation of C3 convertase represents the nodal point for all pathways of complement system activation The alternative pathway of complement activation • The alternative pathway is considered to be a primitive „bypass“ mechanism, that does not require C1, C2 and C4 • The pathway is activated through reaction of the complement system and some substances of microbial origin (polysaccharides – e.g. lipopolysaccharides of G negative bacteria, teichoic acid of G positive bacteria, zymosan from yeast cell walls, surface components of some animal parasites) or other foreign materials The alternative pathway of complement activation • C3 cleaves into C3a + C3b spontaneously; however, these are inactive under standard conditions • In this case, C3b binds to microbial surface → it reacts with factor B → removal of Ba (it is chemotactic for neutrophils) → C3bBb (= C3 convertase of the alternative pathway) – it is stabilized by properdin (P) The lectin pathway of complement activation • The pathway is activated through binding of MBL (mannose-binding lectin) to microbial surface → C4 → C4a is released + C4b → C4b reacts with C2 → C2b is released → C4b2a complex (= C3 convertase) Further events of complement activation process C3 convertase causes generation of: a/ C3a, C4a, C5a fragments - they act as peptide mediators of inflammation - they are chemotactic for phagocytes b/ C3b - it binds to complement receptors and causes opsonization of microbes and immunocomplexes Further events of complement activation process c/ MAC (membrane attack complex) - formed from terminal complement components (C5b, C6, C7, C8, C9); it attacks membrane of cells (e.g.microbes), causing their osmolysis Complement receptors • Fragments of complement components can bind to complement receptors, which are expressed on the surface of different cells. • CR1 – erythrocytes, granulocytes, monocytes and B cells - important for IC clearance • CR2 – B cells and follicular dendritic cells - immunoregulation • CR3, CR4 – phagocytes - opsonization Regulatory mechanisms of the complement system • Some serum proteins enzymatically attack complement components, thereby inactivating them (factor I inactivates C3b; anaphylatoxin inactivator inactivates anaphylatoxins (C3a, C4a, C5a)) • Some serum proteins bind to, and thus inhibit, complement components (C1-INH inhibits C1; C1INH deficiency → HAE = recurrent episodes of local edema; factor H acts with factor I the inhibition of C3b; S protein binds to C5b67 → prevention of MAC binding to cell membrane) Regulatory mechanisms of the complement system • Regulatory proteins in cell membranes (DAF (decay-accelerating factor) – it has the same function as factor H → the inactivation of C3b and C4b; membrane cofactor protein – it serves as a cofactor for inactivation of C4b and C3b) Functions of the complement system • C3a, C5a – anaphylatoxins (= they cause release of histamine and other vasoactive compounds from basophils and mast cells, increasing capillary permeability) • C3b, C4b – opsonization (they bind IC to macrophages and neutrophils, enhancing phagocytosis; also binds complexes to erythrocytes, facilitating removal by the liver and spleen) • C5a – chemotaxis (attracts phagocytic cells to sites of inflammation and increases their overall activity) Functions of the complement system • C8, C9 – components of MAC • Ba – neutrophil chemotaxis • Bb – macrophage activation Functions of the complement system - overview • Inflammation (mast cell degranulation, chemotaxis, increases vascular permeability, margination and diapedesis of polymorphonuclears, smooth muscle contraction, activation of polymorphonuclears, NK cells and macrophages) • Clearance of immune complexes • Cell lysis (G negative bacteria, Protozoa, some viruses) • Viral neutralization • Opsonization The complement system overview • The alternative and lectin pathways are clear components of innate immune system, whereas the classical pathway depends on addaptive immune response (it is triggered through antigenantibody reaction) • Three functions of the complement system: 1/ C3b coats microbes and promotes the binding of these microbes to phagocytes (by receptors for C3b) The complement system overview 2/some breakdown products of complement proteins are chemoattractants for neutrophils and monocytes and promote inflammation at the site of complement activation 3/ complement activation results to the formation of a polymeric protein complex (MAC), causing osmolysis or apoptosis of microbes Antigen • A substance, which is recognized by immune system and induces the immune response • It comes from environment (exoantigen), or from individual’s own structures (autoantigen) • Usually proteins or polysaccharides (lipids and nucleic acids can act as antigens when combined with proteins or polysaccharides) Haptens • Small and well-defined chemical structures, which are not immunogenic themselves, but can add a new epitope when combined to an existing antigen • The antibody directed against the new epitope will react with the free hapten as well as the haptenepitope site in the altered antigen • Typically drugs (e.g.penicillin ATB, hydralazine) Epitope • The portion of antigen, which is recognized by the immune system (lymphocytes, Ig) • Epitopes may be linear (amino acid sequence important), conformational (space conformation important) • Some epitopes are on the antigen’s surface, others are internal • Cross-reactive antigens – share one or more identical or similar epitopes Antigen-antibody reaction • Binding sites of antibodies (paratope) interract with the corresponding sites of the antigen (epitope) • The bonds that hold the antigen-antibody complex are non-covalent (hydrogen, electrostatic and hydrophobic bonds, Van der Waals forces) • Antigen-antibody complex is reversible T cell dependent and independent antigens 1/ T cell dependent antigens - more common, typically contain protein component - a help from T helper cells is necessary for specific humoral immune response generating, otherwise the response is not so effective - the help comes in form of cytokines secreted by the T cell T cell dependent and independent antigens 2/ T cell independent antigens - in some antigens, antibody production can be induced directly, without help from T cells - bacterial lipopolysaccharides and polymeric forms of proteins (e.g. Haemophilus, Str.pneumoniae) Superantigens • Antigenic structures, capable to induce response of T cells by external binding to MHC molecules (i.e. outside of the usual binding site) • The stimulation is polyclonal and extensive • Some bacterial toxins (Staph.aureus, Str.pyogenes, Pseud.aeruginosa) Sequestered antigens • The antigens, which are normally hidden from the immune system at privileged sites, and thus the immune system cannot identify them (e.g. lens, testes) • However, if these allergens are released (injury), the immune system could response to them (the potential mechanism of autoimmunity development) Immunologically privileged tissue • In allogeneic transplantation, some tissues are rejected less frequently (e.g. CNS, cornea, gonades). • The mechanisms of protection from the immune system: separation from the immune system (haematoencephalic barrier); the preference of Th2- and suppression of Th1-reactions; active protection from effector T cells • The privileged status is not absolute (see MS) Molecular size of antigens • Molecules < 5 kDa are not able to induce immune response, the optimal molecular size for immune response induction is approximately 40 kDa Degree of foreignness • An antigen must be foreign or alien to the host • The greater the phylogenetic difference, the more foreign something becomes; based on this fact, we can distinguish the following types of antigens: Degree of foreignness • Autologous – are found within the same individual (e.g. a skin graft from an individual’s thigh to his chest); that is, they are not foreign • Syngeneic – are found in genetically identical individuals (e.g. identical twins); that is, they are not foreign • Allogeneic (alloantigens) – are found in genetically dissimilar members of the same species (e.g. a kidney transplant from mother to daughter); it is foreign • Xenogeneic (heterogeneic) – are found in different species (e.g. a transplant of monkey kidneys to human); it is foreign