* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The Glucose/Fatty Acid Cycle 1963–2003
Survey
Document related concepts
Amino acid synthesis wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Biosynthesis wikipedia , lookup
Butyric acid wikipedia , lookup
Citric acid cycle wikipedia , lookup
Blood sugar level wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Biochemistry wikipedia , lookup
Transcript
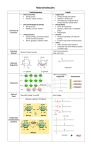
Regulation in Metabolism Group Colloquium Edited by M.A. Titheradge (Sussex) and P. Ferré (INSERM, Paris). Sponsored by AstraZeneca and Institut de Recherches Servier. 679th Meeting of the Biochemical Society held at the University of Essex, Colchester, on July 2–4 2003. The glucose–fatty acid cycle: a physiological perspective K.N. Frayn1 Oxford Centre for Diabetes, Endocrinology and Metabolism, University of Oxford, Churchill Hospital, Oxford OX3 7LJ, U.K. Abstract Glucose and fatty acids are the major fuels for mammalian metabolism and it is clearly essential that mechanisms exist for mutual co-ordination of their utilization. The glucose–fatty acid cycle, as it was proposed in 1963, describes one set of mechanisms by which carbohydrate and fat metabolism interact. Since that time, the importance of the glucose–fatty acid cycle has been confirmed repeatedly, in particular by elevation of plasma non-esterified fatty acid concentrations and demonstration of an impairment of glucose utilization. Since 1963 further means have been elucidated by which glucose and fatty acids interact. These include stimulation of hepatic glucose output by fatty acids, potentiation of glucose-stimulated insulin secretion by fatty acids, and the cellular mechanism whereby high glucose and insulin concentrations inhibit fatty acid oxidation via malonyl-CoA regulation of carnitine palmitoyltransferase-1. The last of these mechanisms, discovered by Denis McGarry and Daniel Foster in 1977, provides an almost exact complement to the mechanism described in the glucose–fatty acid cycle whereby high concentrations of fatty acids inhibit glucose utilization. These additional discoveries have not detracted from the important of the glucose–fatty acid cycle: rather, they have reinforced the importance of mechanisms whereby glucose and fat can interact. Introduction Glucose and fatty acids are the major oxidative fuels in mammals. In humans they account typically for 80% of oxidative metabolism. Cells can only dispose of as much ATP as they have a need for. It is not surprising that powerful regulatory mechanisms have evolved to co-ordinate control of the utilization of glucose and fatty acids. It is within this context that we should see the physiological importance of the concept of the glucose–fatty acid cycle. In current literature the ‘glucose–fatty acid cycle’ is often taken to refer to pathophysiology brought about by elevated plasma NEFA (non-esterified fatty acid) concentrations. (Indeed, all too often the term ‘Randle cycle’ is used to refer Key words: glucose utilization, hepatic glucose output, insulin resistance, insulin secretion, nonesterified fatty acid, tissue triacylglycerol. Abbreviations used: ACC, acetyl-CoA carboxylase; CPT-1, carnitine palmitoyltransferase-1; NEFA, non-esterified fatty acid(s); TG, triacylglycerol. 1 e-mail [email protected] The Glucose/Fatty Acid Cycle 1963–2003 The Glucose/Fatty Acid Cycle 1963–2003: A Tribute to Sir Philip Randle to events in skeletal muscle only, thus ignoring what makes it a cycle, as well as the contributions of Peter Garland, Nick Hales and Eric Newsholme.) Those who take the trouble to read the original paper by Philip Randle and his colleagues [1] will realize that a major part of the paper concerned the operation of the cycle in normal physiology. Here I would like to stress how a careful reading of the paper shows that the authors were amazingly prescient in their views of both physiology and pathophysiology. The glucose–fatty acid cycle and normal physiology Randle and his colleagues called it a cycle because it describes a series of events that interlink carbohydrate and fat metabolism. The basic outline is simple and was well understood in the 1960s. In brief, an elevated glucose concentration stimulates insulin secretion, which then suppresses NEFA C 2003 Biochemical Society 1115 1116 Biochemical Society Transactions (2003) Volume 31, part 6 Figure 1 Substrate and energy balance measured over 5 h following ingestion of three different isoenergetic meals varying in macronutrient composition Meal composition is shown below the histogram. Substrate and energy balance are caculated from the amount ingested and the amount oxidized/expended, measured by indirect calorimetry. Energy balance (solid bars) was identical after the three meals but oxidation of carbohydrate (hatched bars) and fat (open bars) varied reciprocally in accordance with the composition of the meal. Data from [45]. release from adipose tissue depots. This removes competition for substrate utilization in muscle, so that glucose utilization may be stimulated by insulin, unimpeded by high concentrations of fatty acids. When plasma NEFA concentrations are high, usually it is because glucose and insulin concentrations are low, and fatty acids then naturally become the major fuel for skeletal muscle. The original contribution from Randle et al. was the demonstration that there is an additional level of control: elevated fatty acid oxidation in muscle will reduce glucose uptake and oxidation. This much all makes perfect physiological sense. The ‘coarse’ control of the reciprocal utilization of glucose and fatty acids in the body is brought about through insulin secretion: fine-tuning is provided in skeletal muscle, by the mechanism Randle et al. elucidated in a series of studies prior to the ‘cycle’ paper. The intimate but reciprocal relationship between carbohdyrate and fat oxidation in vivo is illustrated in Figure 1. After isoenergetic meals of differing macronutrient composition, energy balance is identical, but the carbohydrate and fat balances that contribute to energy balance change reciprocally in accordance with meal composition. The inhibitory effect of elevated NEFA concentrations on glucose utilization by skeletal muscle has been shown repeatedly in human experiments in vivo. The experimental paradigm invariably involves infusion of an intravenous TG (triacylglycerol) emulsion together with heparin, which releases the enzyme lipoprotein lipase into the circulation. C 2003 Biochemical Society Lipoprotein lipase rapidly hydrolyses circulating TG to raise plasma NEFA concentrations. Under these conditions, the plasma NEFA concentration is often reported to be elevated to supra-physiological levels, although these may be artefactual, caused by continuing lipolysis in vitro [2]. It should also be noted that this is not a pure elevation of plasma NEFA concentrations: plasma TG, monoacylglycerol [3] and glycerol concentrations are also raised. Nevertheless, the results are consistent: whole-body or, more specifically, muscle glucose utilization is impaired [4,5], typically after delay of about 2 h [6]. Since 1963, further aspects of the mutual interrelationships of glucose and fatty acids have come to light. These include the effects of fatty acids themselves upon glucose-stimulated insulin secretion, the effects of fatty acids upon hepatic glucose metabolism and the mechanism discovered by the late Denis McGarry and Daniel Foster in 1977 [7], whereby high glucose and insulin concentrations can suppress fatty acid oxidation – the exact complement to the mechanism described by Randle and colleagues. Again, all these can be seen as further ‘fine-tuning’ of the balance between glucose and fatty acid metabolism. Fatty acids and insulin secretion The recognition that fatty acids may act directly upon the pancreatic β-cell to regulate glucose-stimulated insulin The Glucose/Fatty Acid Cycle 1963–2003 Figure 2 Plasma insulin concentrations in response to glucose, in the presence of elevated concentrations of specific NEFA Glucose was infused from 210 min to stimulate insulin secretion. The effect of elevation of fatty acids compared with the control was highly significant (P < 0.001) and the effects of the various types of fatty acid were also different from one another (P < 0.01). Data are from eight normal subjects, reproduced from Diabetologia, “Interaction between specific fatty acids, GLP-1 and insulin secretion in humans”, C. Beysen, F. Karpe, B.A. Fielding, A. Clark, J.C. Levy and K.N. Frayn, c Springer-Verlag GmbH & Co., with permission. Elevated NEFA: 䉱, monounsaturated; vol 45, pp. 1533–1541, fig. 3, 2002 䊉, polyunsaturated; 䉭, saturated; 䊊, control (no elevation of fatty acid concentrations). secretion is not new [8,9] but has received a boost with more intensive study in recent years. It is now clear that the effect of fatty acids upon glucose-stimulated insulin secretion is biphasic. Initially fatty acids potentiate the effects of glucose. After some hours of prolonged exposure to high fatty acid concentrations (somewhere between 12 and 24 h) this changes to an inhibition [10]. Since prolonged high fatty acid concentrations are a feature of pathophysiology rather than normal daily life, we might imagine that the normal physiology of this system is that high levels of fatty acids, if present together with an elevated glucose concentration, tend to limit their own utilization by some stimulation of insulin secretion [11,12]. It is also clear that there is a critical need for fatty acids for the β-cell to be able to respond to glucose [13]. One feature of this mechanism that has caused some interest is that, at least in perifused or isolated islets, the effect of fatty acids upon glucose-stimulated insulin secretion is fatty acidspecific [14]. Saturated fatty acids cause more potentiation than do unsaturated ones [15]. This has led to speculation that dietary saturated fatty acids might tend to lead to insulin resistance through chronic stimulation of insulin secretion. However, when tested in vivo in humans, the effect is not so clear cut, perhaps because of interaction with glucagonlike peptide-1 secretion; in fact the greatest effect is then seen with monounsaturated fatty acids [16] (Figure 2). The mechanism for the stimulatory effect of fatty acids upon glucose-stimulated insulin secretion is not yet entirely clear although a cell-surface G-protein-coupled receptor for fatty acids has recently been described in β-cells [17]. The longerterm inhibitory effects seem to reflect accumulation of TG and long-chain acyl-CoA in the β-cell with possible direct effects of the latter on ATP-channel activity [18]. Fatty acids and hepatic glucose production The effect of fatty acids upon hepatic glucose metabolism was first shown in vivo in humans by Ferrannini and colleagues [4]. They showed that elevated circulating NEFA concentrations stimulated hepatic glucose output in the presence of relative insulinopaenia. This effect has been the subject of many investigations (e.g. [6,19–21]). It has also been debated to a considerable extent. Hepatic glucose production in the fasted state is via two routes: glycogenolysis and gluconeogenesis. Some studies suggest that fatty acids stimulate one or other of these processes, but that ‘hepatic autoregulation’ adjusts the other to compensate so that total glucose output is unaffected [19,22]. On balance, however, what seems clear is that fatty acids will counteract the normal insulin-suppression of hepatic glucose output [20,22,23]. At first sight this seems like pathophysiology rather than physiology. Inappropriately elevated fatty acid concentrations – as seen in type 2 diabetes, for example [24] – stimulate glucose production, and glucose intolerance is worsened. But there is an alternative view. The interactions between C 2003 Biochemical Society 1117 1118 Biochemical Society Transactions (2003) Volume 31, part 6 glucose and fatty acids seem mainly to ensure preferential use of glucose when available, and preservation of fat stores. That could be said for the potentiation of glucose-stimulated insulin secretion by fatty acids: high fatty acid concentrations will down-regulate themselves. Just the same is true for the effect on hepatic glucose output. We should remember that the substrates for gluconeogenesis are mainly glucose-derived (i.e. recycled glucose from peripheral tissues in the form of lactate, pyruvate and alanine), so fatty acids are simply replacing carbohydrate-derived substrates as a fuel for hepatic metabolism and thereby regulating their own usage. The suppression of hepatic glucose output by insulin has been attributed, by some, to an indirect effect, possibly via lowering of NEFA supply to the liver [25,26]. This does not seem to be borne out in the liver-specific insulin-receptorknockout mouse: insulin-induced suppression of hepatic glucose output was lost, despite normal lowering of plasma NEFA by insulin [27]. But that is a very unphysiological system [28] and, on balance, a substantial role of NEFA in normal regulation of hepatic glucose output remains probable. Malonyl-CoA and fatty acid oxidation Finally, in ‘updating’ the normal physiology that the glucose– fatty acid cycle underlies, one must appreciate the beautiful complementarity of the regulation of fatty acid oxidation by glucose, achieved through malonyl-CoA inhibition of CPT-1 (carnitine palmitoyltransferase-1). Although McGarry et al. first described this as a mechanism whereby carbohydrate availability reduced ketogenesis in the liver [7], we now recognize that the same mechanism operates in muscle and perhaps other tissues. The muscle-specific isoform of CPT-1 is actually more sensitive to inhibition by malonyl-CoA than is the liver isoform [29]. An interesting feature to emerge from more recent work is that there also two isoforms of ACC (acetyl-CoA carboxylase; producing malonyl-CoA), one (ACC-1 or ACC-α) expressed in tissues that synthesize fatty acids (e.g. liver, adipose tissue), the other (ACC-2 or ACC-β) expressed in non-lipogenic tissues such as skeletal and cardiac muscle. ACC-2 is generally expressed along with the muscle isoform of CPT-1 [29]. There can be little doubt that the purpose of ACC-2 is to produce malonyl-CoA purely for the purpose of regulation of fatty acid oxidation. In summary, we now recognize more aspects in which fatty acid and glucose metabolism are inter-related than were known in 1963. But none of these detracts from the basic aspects of the glucose–fatty acid cycle as it was originally applied to explaining normal physiology: they simply reinforce the powerful need of the organism to regulate oxidation of these two major fuels. The glucose–fatty acid cycle and pathophysiology TG accumulation in tissues Most citations of the 1963 paper [1] refer to elevated NEFA concentrations inhibiting glucose utilization. In fact C 2003 Biochemical Society the paper was very clear in discussing elevated fatty acid supply, and Randle et al. recognized the potential importance of TG accumulation within tissues (especially muscle) in contributing acyl groups for β-oxidation: “We suggest that there is a distinct biochemical syndrome . . . due to breakdown of glycerides in adipose tissue and muscle, the symptoms of which are a high concentration of plasma NEFA, impaired sensitivity to insulin . . . ” Again, this was amazingly prescient. A close relationship between muscle TG accumulation and insulin resistance is now well established [30,31]. There is debate about whether TG accumulation in muscle is the cause or an effect of insulin resistance. Observations of impaired fatty acid oxidation in muscle in insulin-resistant states might suggest the latter [32– 34], but when muscle TG concentrations are manipulated acutely by altering NEFA supply, insulin resistance runs in parallel [35]. It has been suggested that acyl-CoAs are the active species in mediating insulin resistance in this context [36,37]; parenthetically, it should be noted that Randle and colleagues also anticipated this: “One possibility . . . is inhibition of the enzymes concerned by acyl coenzyme A compounds” [1]. More recently, imaging techniques to measure liver TG content have also shown close relationships with insulin resistance [38,39]. This can also be linked to the longer-term suppressive effect of fatty acids on glucosestimulated insulin secretion, referred to above: this effect may relate to TG accumulation within the pancreatic islet [40]. In fact, in animal models in which the tissue TG content is varied (e.g. by adenoviral expression of leptin to reduce fat stores), there is a close relationship between whole-body insulin sensitivity and the TG content of muscle, liver and pancreas [41]. Metabolic ‘inflexibility’ The concept of ‘metabolic inflexibility’ has recently been discussed in association with insulin resistance [42–44]. The idea is that tissues (such as skeletal muscle) normally adapt their use of metabolic fuels in a dynamic manner according to nutrient supply. Skeletal muscle, for instance, oxidizes mainly fatty acids in the postabsorptive state but mainly glucose in the postprandial state. David Kelley and colleagues proposed that insulin resistance is characterized by ‘metabolic inflexibility’. They illlustrated this with data from studies of human leg glucose oxidation in vivo. In the postabsorptive state, glucose oxidation (relative to fat oxidation, as measured by the local respiratory quotient) is not reduced in insulin-resistant obese or type 2 diabetic subjects; in fact it is higher than in lean, insulin-sensitive subjects. But when the postprandial state is simulated by infusion of glucose and insulin, then glucose oxidation rises sharply in the leg of lean subjects, whereas it does not change in obese and diabetic subjects, with the result that under hyperinsulinaemic conditions muscle glucose oxidation is lower in insulin-resistant than in insulin-sensitive subjects The Glucose/Fatty Acid Cycle 1963–2003 [42]. The explanation may well relate to the glucose–fatty acid cycle. This condition of metabolic inflexibility is closely associated with muscle TG accumulation [43,44]. It could be that lipid fuel supply to the muscle is dominated by the intracellular lipid deposits, and continues to be available even in the presence of high external glucose and insulin concentrations. The concept of metabolic flexibility (insulin sensitivity) and inflexibility (insulin resistance) may, in fact, be an alternative way of looking at the glucose–fatty acid cycle. I thank the Wellcome Trust and the Humane Research Trust for funding our work in this area. References 1 Randle, P.J., Garland, P.B., Hales, C.N. and Newsholme, E.A. (1963) Lancet i, 785–789 2 Beysen, C., Belcher, A.K., Karpe, F., Fielding, B.A., Herrera, E. and Frayn, K.N. (2003) Am. J. Physiol. Endocrinol. Metab. 284, E18–E24 3 Fielding, B.A., Humphreys, S.M., Allman, R.F.C. and Frayn, K.N. (1993) Clin. Chim. Acta 216, 167–173 4 Ferrannini, E., Barrett, E.J., Bevilacqua, S. and DeFronzo, R.A. (1983) J. Clin. Invest. 72, 1737–1747 5 Kelley, D.E., Mokan, M., Simoneau, J.-A. and Mandarino, L.J. (1993) J. Clin. Invest. 92, 91–98 6 Boden, G., Chen, X., Ruiz, J., White, J.V. and Rossetti, L. (1994) J. Clin. Invest. 93, 2438–2446 7 McGarry, J.D., Mannaerts, G.P. and Foster, D.W. (1977) J. Clin. Invest. 60, 265–270 8 Greenough, W.B., Crespin, S.R. and Steinberg, D. (1967) Lancet ii, 1334–1336 9 Seyffert, Jr, W.A. and Madison, L.L. (1967) Diabetes 16, 765–776 10 Grill, V. and Qvigstad, E. (2000) Br. J. Nutr. 83, (suppl. 1), S79–S84 11 McGarry, J.D. and Dobbins, R.L. (1999) Diabetologia 42, 128–138 12 McGarry, J.D. (2002) Diabetes 51, 7–18 13 Dobbins, R.L., Chester, M.W., Stevenson, B.E., Daniels, M.B., Stein, D.T. and McGarry, J.D. (1998) J. Clin. Invest. 101, 2370–2376 14 Gravena, C., Mathias, P.C. and Ashcroft, S.J. (2002) J. Endocrinol. 173, 73–80 15 Stein, D.T., Stevenson, B.E., Chester, M.W., Basit, M., Daniels, M.B., Turley, S.D. and McGarry, J.D. (1997) J. Clin. Invest. 100, 398–403 16 Beysen, C., Karpe, F., Fielding, B.A., Clark, A., Levy, J.C. and Frayn, K.N. (2002) Diabetologia 45, 1533–1541 17 Itoh, Y., Kawamata, Y., Harada, M., Kobayashi, M., Fujii, R., Fukusumi, S., Ogi, K., Hosoya, M., Tanaka, Y., Uejima, H. et al. (2003) Nature (London) 422, 173–176 18 Gribble, F.M., Proks, P., Corkey, B.E. and Ashcroft, F.M. (1998) J. Biol. Chem. 273, 26383–26387 19 Chen, X., Iqbal, N. and Boden, G. (1999) J. Clin. Invest. 103, 365–372 20 Shah, P.V., Vella, A., Basu, A., Basu, R., Adkins, A., Schwenk, W.F., Johnson, C.M., Nair, K.S., Jensen, M.D. and Rizza, R.A. (2002) Diabetes 51, 301–310 21 Staehr, P., Hother Nielsen, O., Landau, B.R., Chandramouli, V., Holst, J.J. and Beck-Nielsen, H. (2003) Diabetes 52, 260–267 22 Lam, T.K., Carpentier, A., Lewis, G.F., van de Werve, G., Fantus, I.G. and Giacca, A. (2003) Am. J. Physiol. Endocrinol. Metab. 284, E863–E873 23 Fanelli, C., Calderone, S., Epifano, L., De Vincenzo, A., Modarelli, F., Pampanelli, S., Perriello, G., De Feo, P., Brunetti, P., Gerich, J.E. and Bolli, G.B. (1993) J. Clin. Invest. 92, 1617–1622 24 Reaven, G.M., Hollenbeck, C., Jeng, C.-Y., Wu, M.S. and Chen, Y.-D.I. (1988) Diabetes 37, 1020–1024 25 Rebrin, K., Steil, G.M., Getty, L. and Bergman, R.N. (1995) Diabetes 44, 1038–1045 26 Cherrington, A.D., Edgerton, D. and Sindelar, D.K. (1998) Diabetologia 41, 987–996 27 Fisher, S.J. and Kahn, C.R. (2003) J. Clin. Invest. 111, 463–468 28 Barrett, E.J. (2003) J. Clin. Invest. 111, 434–435 29 Zammit, V.A. (1999) Biochem. J. 343, 505–515 30 Phillips, D.I.W., Caddy, S., Ilic, V., Fielding, B.A., Frayn, K.N., Borthwick, A.C. and Taylor, R. (1996) Metab. Clin. Exp. 45, 947–950 31 Forouhi, N.G., Jenkinson, G., Thomas, E.L., Mullick, S., Mierisova, S., Bhonsle, U., McKeigue, P.M. and Bell, J.D. (1999) Diabetologia 42, 932–935 32 Blaak, E.E., Van Baak, M.A., Kemerink, G.J., Pakbiers, M.T., Heidendal, G.A. and Saris, W.H. (1994) Am. J. Physiol. 267, E306–E315 33 Mensink, M., Blaak, E.E., van Baak, M.A., Wagenmakers, A.J. and Saris, W.H. (2001) Diabetes 50, 2548–2554 34 Blaak, E.E. and Wagenmakers, A.J. (2002) Diabetes 51, 784–789 35 Boden, G., Lebed, B., Schatz, M., Homko, C. and Lemieux, S. (2001) Diabetes 50, 1612–1617 36 Ellis, B.A., Poynten, A., Lowy, A.J., Furler, S.M., Chisholm, D.J., Kraegen, E.W. and Cooney, G.J. (2000) Am. J. Physiol. Endocrinol. Metab. 279, E554–E560 37 Thompson, A.L. and Cooney, G.J. (2000) Diabetes 49, 1761–1765 38 Ryysy, L., Häkkinen, A.-M., Goto, T., Vehkavaara, S., Westerbacka, J., Halavaara, J. and Yki-Järvinen, H. (2000) Diabetes 49, 749–758 39 Seppälä Lindroos, A., Vehkavaara, S., Häkkinen, A.-M., Goto, T., Westerbacka, J., Sovijarvi, A., Halavaara, J. and Yki-Järvinen, H. (2002) J. Clin. Endocrinol. Metab. 87, 3023–3028 40 Segall, L., Lameloise, N., Assimacopoulos Jeannet, F., Roche, E., Corkey, P., Thumelin, S., Corkey, B.E. and Prentki, M. (1999) Am. J. Physiol. 277, E521–E528 41 Koyama, K., Chen, G., Lee, Y. and Unger, R.H. (1997) Am. J. Physiol. 273, E708–E713 42 Kelley, D.E. and Mandarino, L.J. (2000) Diabetes 49, 677–683 43 Kelley, D.E. and Goodpaster, B.H. (2001) Diabetes Care 24, 933–941 44 Kelley, D.E., Goodpaster, B.H. and Storlien, L. (2002) Annu. Rev. Nutr. 22, 325–346 45 Whitley, H.A., Humphreys, S.M., Samra, J.S., Campbell, I.T., MacLaren, D.P.M., Reilly, T. and Frayn, K.N. (1997) Br. J. Nutr. 78, 15–26 Received 11 June 2003 C 2003 Biochemical Society 1119