* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 11 Blood and Immune System notes
Molecular mimicry wikipedia , lookup
Adaptive immune system wikipedia , lookup
Atherosclerosis wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Innate immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
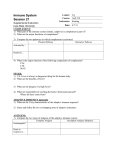
BIOLOGY 20 CHAPTER 11 BLOOD AND IMMUNE SYSTEM Nelson Pages 348 – 375 Dividing the cell into its parts (or fractions) is called cell fractionation and is achieved by the process of centrifugation using a centrifuge. Average 70 kg person has about 5 L of blood Blood 55 % fluid or plasma 45 % blood cells Plasma 90 % H2O Also: Proteins, glucose, vitamins, minerals, dissolved gases, and waste products of metabolism Types Functions •Albumins •Osmotic balance – maintain H2O levels •Globulins •Antibodies, immunity (immunoglobulins) •Fibrinogen •Blood clotting Red blood cells or RBC’s Transport O2 Packed with hemoglobin Greatly increases capacity of RBC to carry O2, by 70 X Heme – iron containing pigment Globin – protein structure Oxyhemoglobin - gives blood its red color RBC’s Are biconcave Greater surface area for gas exchange Are enucleated (no nucleus) when mature More room for cell to carry hemoglobin Are made in bone marrow – erythropoieses Are broken down by spleen and liver Heme is transformed into bile pigments Iron returns to liver for storage and bone marrow for reuse RBC’s and low O2 levels Exercise, high altitude, hemorrhage Lowers O2 levels in blood kidneys release REF RBC production in bone marrow Anemia Reduction in blood O2 due to low levels of hemoglobin or poor RBC production Causes: hemorrhage, dietary deficiency in iron White blood cells or WBC’s Outnumbered by RBC’s Have a nucleus Types of WBC’s a.) Granulocytes b) Agranulocytes Why You Are Still Alive https://www.youtube.com/watch?v=zQGOcOUB i6s c) Phagocytes Destroy invading microbes by phagocytosis Diapedesis – move like an amoeba • Lysosomes release digestive enzymes Digests microbe as well as itself • Pus forms – fragments of WBC and invader Phagocytosis http://faculty.ccbcmd.edu/~gkaiser/biotutori als/eustruct/images/phagocyt.gif http://highered.mheducation.com/sites/007 2495855/student_view0/chapter2/animatio n__phagocytosis.html A colored scanning electron micrograph of a macrophage engulfing a parasite of the Leishmania genus. To defend the body, macrophages will surround a foreign invader, bring it inside the cell, then use enzymes to digest the material. Types of Phagocytes: a.) Neutrophils: Toxins, hemorrhage, fever, burns b.) Eosinophils: Allergies and parasitic worms c.) Basophils: Damage to tissues http://www.wisconline.com/objects/index_tj.asp?objid=AP1 4704 Other WBC’s form antibodies which interfere with invading microbes Neutrophils are very active in phagocyting bacteria and are present in large amount in the pus of wounds. 11 Eosinophils attack parasites and phagocyte antigenantibody complexes. 12 Basophil secrete anticoagulant and vasodilatory substances as histamines and serotonin. Even if they have a phagocytory capability, their main function is secreting substances which mediate the hypersensitivity reaction. 13 The lymphocytes are the main constituents of the immune system which is a defense against the attack of pathogenic microorganisms such as viruses, bacteria, fungi and protista. Lymphocytes yield antibodies and arrange them on their membrane. Two types: B and T lymphocytes 14 Monocytes are the precursors of macrophages. After attaining maturity in the bone marrow, enter the blood circulation. Then they migrate into the connective tissue, where they become macrophages and move within the tissues. In the presence of an inflammation site, monocytes quickly migrate from the blood vessel and start an intense phagocytory activity. 15 thrombocytes A.k.a Do not contain a nucleus Produced in bone marrow Move through blood vessels and initiate blood clotting reactions Prevent blood loss Process: platelet Platelet breaks 2+ and Ca strikes a apart thromboplastin becomes and torn thrombin activates releases blood prothrombin thrombo vessel -plastin cannot enter but WBC’s can Microbes splices fibrinogen converted into fibrin wraps around cut and seals it Thrombus – blocks a blood vessel Types: Coronary Cerebral – stroke If a blood clot moves or dislodges, it becomes an embolus Types of embolisms: Pulmonary, coronary, cerebral Hemophilia An inherited defect in the clotting process Experiments with blood transfusions, the transfer of blood or blood components into a person's blood stream, have been carried out for hundreds of years. Many patients have died and it was not until 1901, when the Austrian Karl Landsteiner discovered human blood groups, that blood transfusions became safer. Mixing blood from two individuals can lead to blood clumping or agglutination. This can have fatal consequences. Karl Landsteiner discovered that blood clumping was an immunological reaction which occurs when the receiver of a blood transfusion has antibodies against the donor blood cells. Karl Landsteiner's work made it possible to determine blood types and thus paved the way for blood transfusions to be carried out safely. For this discovery he was awarded the Nobel Prize in Physiology or Medicine in 1930. IMPORTANT TERMS Antigen Molecules that cause the synthesis of antibodies when injected into another organism Antibody Proteins found in blood that attack and neutralize substances that are foreign to the body The differences in human blood are due to the presence or absence of certain protein molecules called antigens (agglutinogens) and antibodies (agglutinins). The antigens are located on the surface of the red blood cells and the antibodies are in the blood plasma. Individuals have different types and combinations of these molecules. The blood group you belong to depends on what you have inherited from your parents. According to the AB0 blood typing system there are four different kinds of blood types: A, B, AB or 0 Blood group A If you belong to the blood group A, you have A antigens on the surface of your red blood cells and B antibodies in your blood plasma. Blood group B If you belong to the blood group B, you have B antigens on the surface of your red blood cells and A antibodies in your blood plasma. Blood group AB If you belong to the blood group AB, you have both A and B antigens on the surface of your red blood cells and no A or B antibodies at all in your blood plasma. Blood group 0 If you belong to the blood group 0, you have neither A or B antigens on the surface of your red blood cells but you have both A and B antibodies in your blood plasma. ABO BLOOD TYPE SUMMARY: AGGLUTINATION REACTION According to above blood grouping systems, you can belong to either of following 8 blood groups: A Rh+ (34%) B Rh+ (9%) AB Rh+ (3%) 0 Rh+ (38%) A Rh(6%) B Rh(2%) AB Rh(1%) 0 Rh(7%) 1. You mix the blood with three different reagents including either of the three different antibodies, A, B or Rh antibodies. 2. Then you take a look at what has happened. In which mixtures has agglutination occurred? The agglutination indicates that the blood has reacted with a certain antibody and therefore is not compatible with blood containing that kind of antibody. If the blood does not agglutinate, it indicates that the blood does not have the antigens binding the special antibody in the reagent. 3.If you know which antigens are in the person's blood, it's easy to figure out which blood group he or she belongs to! Try your luck with the Blood typing game!!! http://nobelprize.org/medicine/educational/ landsteiner/index.html People with blood group 0 are called "universal donors" and people with blood group AB are called "universal receivers." Universal Donors! Universal Recipients! Many people also have a so called Rh factor on the red blood cell's surface. This is also an antigen and those who have it are called Rh+. Those who haven't are called Rh-. A person with Rh- blood does not have Rh antibodies naturally in the blood plasma. But a person with Rh- blood can develop Rh antibodies in the blood plasma if he or she receives blood from a person with Rh+ blood, whose Rh antigens can trigger the production of Rh antibodies. A person with Rh+ blood can receive blood from a person with Rh- blood without any problems. First studied in rhesus monkeys Types Rh positive: Have these antigens present on surface of RBCs Rh negative: Do not have these antigens present Hemolytic disease of the newborn (HDN) Mother produces anti-Rh antibodies that cross placenta and cause agglutination and hemolysis of fetal RBCs ERYTHROBLASTOSIS FETALIS Type and crossmatch Blood typing determines the ABO and Rh blood groups of a blood sample. A crossmatch tests for agglutination reactions between donor and recipient blood •Complete blood count……The complete blood count consists of the following: red blood cell count, hemoglobin measurement (grams of hemoglobin per 100mL of blood), hematocrit measurement (percent volume of red blood cells), and white blood cell count Differential White blood count It determines the percentage of each type of white blood cell Clotting Platelet count and prothrombin time measures the ability of the blood to clot •Blood chemistry….The composition of materials dissolved or suspended in plasma (e.g. glucose, urea, nitrogen, bilirubin and cholesterol) can be used to assess the functioning and status of the body’s system 11.2 THE BODY’S LINE OF DEFENSE PAGES 357 - 366 Biology 20 Unit D 11.2 THE BODY’S LINE OF DEFENCE Pathogen: an organism causing disease An infectious disease may be caused by: Viruses, bacteria, fungi, protozoa, flatworms and roundworms Staphylococcus aureus can be pathogen in the right conditions on the surface of the skin (causing impetigo and other skin conditions) Parasites Head Lice (adult stage) Malaria: Singlecelled protozoan parasites of the genus Plasmodium. Four species infect humans by entering the bloodstream. Giardia: a fungi that infects the intestines of animals causing “beaver fever”. People most often get it from drinking contaminated water TAPEWORMS, PATHOGENS RINGWORMS, AND OTHER VIRUSES Influenza Virus (Flu) Human Immunodeficiency Virus (AIDS) BACTERIA Salmonella typhimurium (Food Poisoning) Syphilis- is an infectious venereal disease caused by the spirochete Treponema pallidum I.) FIRST LINE OF DEFENCE: NONSPECIFIC AND EXTERNAL Skin – protective Acidic secretions (pH of 3 – 5) Respiratory tract (windpipe) – mucus and cilia sweep foreign material away from lung Stomach – acids and protein digesting enzymes destroy microbes Tears, saliva, mucous secretions – lysozyme (enzyme) destroys bacterial cell walls (P357) II.) SECOND LINE OF DEFENCE – NONSPECIFIC AND INTERNAL (P357) A. Phagocytes (WBC’s) destroy microbes T YPES OF PHAGOCYTES Phagocytosis Ingestion of invading microbes by certain WBCs Pus - remaining fragments of protein, dead WBCs, digested invader B. INFLAMMATORY RESPONSE Tissue damage due to physical injury Initiates an inflammatory response Nonspecific response that results in swelling, heat, and pain Clues to second line of defence: Pus Inflammation Neutrophils and macrophages digest invaders Release chemicals Reach hypothalamus Reset body temperature to about 40OC Fever makes it difficult for harmful bacteria to survive Fevers 40OC can be unsafe Enzymes start to denature D. PROTECTIVE PROTEINS i) - prevent multiplication of bacteria and viruses complement active against bacteria once activated, some complements form pores in bacterial cell walls and membranes pores allow salts and fluids to enter bacterial cell bacterium expands until it bursts E. INTERFERON active against viruses tissue cells infected by viruses produce and secrete interferon chemical binds to uninfected cells these cells now produce substances that interfere with viral replication slower, but more specific white blood cells and lymph system are involved WBC respond to antigens: any substance recognized as foreign to the body often antigens are part of a bacterial cell wall, viral coat, or foreign cell membrane CELLS OF THE IMMUNE SYSTEM OVERVIEW: BONE MARROW RBC Stay and Mature WBC GRANULAR AGRANULAR: 1. Basophils 1. Monocytes: -mature into macrophages 2. Neutrophils 2. Lymphocytes 3. Eosinophils mature in Thymus Gland mature in Bone Marrow T- cells B - cells migrate to lymph nodes and spleen circulate in blood and lymph Immune system detects an antigen T-cells multiply which attack the invader directly called cell-mediated immunity: cells move thru blood and lymph target: bacteria, viruses, etc. that have toxins infected host cells; cancer cells, implanted tissues B-cells multiply which produce antibodies Called antibody mediated immunity: antibodies move thru blood and lymph target: free bacteria, viruses, and in body fluids 1. CELL-MEDIATED IMMUNITY a macrophage engulfs a bacterium, then the bacterial antigen, along with an identification protein, will be displayed on the macrophage membrane appropriate T-cell and its receptor is presented with the antigen, and is now activated T-cell then grows and divides into the following: a) Helper T-cell directly stimulates a B-cell by presenting an antigen to it b) Killer T-cell release a chemical which forms a pore in foreign cell membrane bearing an antigen; cell swells and bursts c) Suppressor T-cells number increases slowly suppress immune response d) Memory T-cells recognizes original invading antigen; can last a life-time lymphokines: to divide chemicals which stimulate immune cells 2. ANTIBODY-MEDIATED IMMUNITY B-cells produce antibodies: proteins which combine with and inactivate antigens antigen binds to membrane-bound antibody on B-cell B-cell divides into: many plasma cells which produce and release antibodies into blood and lymph memory B-cells that remain in bloodstream antibody level increases, and antigens disappear from body SUMMARY OF 3RD LINE OF DEFENCE KILLER T-CELLS (CYTOTOXIC T CELL) DESTROY INFECTED HOST CELLS…KILL THE VIRUS WHERE IT’S MADE! http://bcs.whfreeman.com/thelifewire/content/chp18/1 802004.html http://highered.mcgrawhill.com/olc/dl/120110/micro33.swf Biology 20 Unit D Section 11.3: Malfunctions of the Immune System – Pages 367-370 Directions: READ Section 11.3 In the TEXTBOOK and complete your own notes using the following slides as a guide. 11.3 MALFUNCTIONS 1. OF THE IMMUNE SYSTEM Can cause two types of problems: Immunodeficiency diseases Caused by: Virus (HIV) Hereditary condition (severe combined immunodeficiency) SCID Gene mutation Inability to produce T and B cells Exposure to cancer therapy or use of anti – inflammatory drugs 1. Inappropriate attacks of immune system against non – threatening agents Allergies Autoimmune disorders I.) ALLERGIES Immune system mistakes harmless cells as harmful Symptoms: Tissue swelling Mucus secretion Constricted air passages Severe allergic reactions may cause anaphylactic reactions Hives, itching, swelling Cells that “believe” they are in danger release bradykinin Stimulates release of histamine Produced by basophils (WBCs) and mast cells •Increases permeability of cells of capillaries Causes reddening •PROTEINS AND WBCS LEAVE CAPILLARY IN SEARCH OF MICROBE •Hypertonic, thus, water follows by diffusion Reactions may be brought on by: Medications, vaccines, foods Anaphylactic shock can occur quickly Weakness, sweating, difficulty breathing Nausea, diarrhoea, drop in blood pressure Treatments or prevention: Antihistamines Medical alert bracelet or necklace Read labels II.) AUTOIMMUNE DISORDERS Immune system mistakenly attacks own cells of body Renegade lymphocytes treat body’s cells as foreign and attack own body’s cells Usually held in check Mutated T and B cells Theory: suppressors secrete a substance that tells macrophage to engulf renegade cells Failure of suppressor T cells to control renegade lymphocytes Rheumatoid arthritis Against connective tissue of joints Rheumatic fever Scars heart muscle Type I diabetes Against insulin – producing cells of pancreas Lupus Accumulation of antigen – antibody complexes that build up on walls of blood vessels, kidneys, joints, and skin Multiple sclerosis Against myelin sheath of nerve cells III.) ORGAN TRANSPLANT REJECTION Main challenge is immune system’s ability to distinguish “self” from “nonself” Donor organ is identified by distinctive protein markers on its cell membranes Major histocompatability complex (MHC) Unique to each individual Organ recipient makes antibodies designed to destroy foreign invader Attempts are made to match MHC of the tissues of donors and recipients as closely as possible Close relatives Recently deceased donors To reduce rejection, immunosuppressant drugs are administered Also reduces immune system’s ability to fight off invading microbes Place patients at risk for infections ORGAN TRANSPLANTS IN ALBERTA Alberta’s Capital Health Regional Transplant Program At the U of A Hospital and Stollery Children’s Hospital HOPE (human organ procurement and exchange) Coordination, recovery, and distribution of organs in Alberta Tissues include: eyes (cornea and sclera), skin, heart valves, and bone IV.) STEM CELL RESEARCH Stem cells Are pluripotent Can give rise to different types of body cells Can replace pancreatic islet cells that have been damaged Can repair damaged cartilage or cardiac tissue Exist in adult skin stems cells as multipotent stem cells Can be directed to become neurons or muscle cells Weakening of suppressor T cells: Drugs or serious infections Decline with age Some people are born with defective suppressor T cells Treatment Immune suppressing drugs Reduce intensity of renegade cells Autoimmune disease Immune system mistakenly attacks own cells of body Mutated T and B cells Failure of suppressor T cells Attempts are made to match MHC of the tissues of donors and recipients as closely as possible Close relatives Recently deceased donors To reduce rejection, immunosuppressant drugs are administered Also reduces immune system’s ability to fight off invading microbes Place patients at risk for infections