* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Histology of the mucosal lymphatic tissues The lymphoid system is
Molecular mimicry wikipedia , lookup
Immune system wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
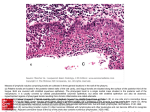
بسم هللا الرحمن الرحيم Histology of the mucosal lymphatic tissues MUCOSO-LYMPHOID ORGANS Peyer’s patch V. APPENDIX ILEUM The lymphoid system is divided into a series of functional anatomical compartments, of which the 2 most important are: The peripheral lymphoid system (made up of the lymphatic organs e.g. spleen & lymph nodes): this is the compartment that responds to antigens that have entered the tissues or spread into the blood. The mucosal lymphoid system located near the surfaces where most pathogens invade: is the mucosal immune system (commonly described as MALT). 2 further distinct compartments are: The body cavities (peritoneum and pleura). Skin associated lymphatic tissue (SALT). The Mucosal Immune System The mucous membranes are one of the largest organs of the body. They comprise the linings of the gastrointestinal, urogenital & respiratory tracts. The mucosal surfaces of the body are highly vulnerable to infection. They are thin and permeable barriers to the interior of the body because of their physiological activities in gas exchange (the lungs), food absorption (the gut), sensory activities (eyes, nose, mouth, and throat), and reproduction (uterus and vagina). The immune system of the MALT differs from that of the rest of the peripheral lymphoid system in several respects: The types and distribution of T cells differ, with significantly greater numbers of intraepithelial T lymphocytes (IEL) in and lamina propria (LPL) in the gut mucosa compared with peripheral L.Ns & blood. The major antibody type secreted across the epithelial cells lining mucosal surfaces is secretory IgA. This is synthesized by plasma cells in the lamina propria and transported into the lumen of the gut through epithelial cells (enterocytes) at the base of the intestinal crypts by transcytosis. IgA binds to the mucus layer overlying the gut epithelium and acts as an antigen-specific barrier to pathogens and toxins in the gut lumen. The mucosal lymphoid system is exposed to foreign antigens from foods, commensal bacteria of gut & from pathogenic microorganisms and parasites. No immune response can normally be detected to food antigens. Indeed, soluble antigens taken by mouth may induce antigen-specific tolerance or antigen-specific suppression. In contrast, pathogenic microorganisms induce strong protective response. Gut-associated lymphoid tissue (GALT) This is comprised of: A) Mucoso-lymphoid organs Tonsils (palatine, lingual, pharyngeal). Peyer's patches in ileum. Lymphoid aggregates in the appendix and large intestine. Lymphoid tissue accumulating with age in the stomach. Small lymphoid aggregates in the esophagus. B) Diffusely distributed immune cells Lymphocytes and plasma cells. M (microfold) cells. Mucosal mast cells. Antigen Presenting Cells (APC). A) Mucoso-lymphoid organs 1. The tonsils are incompletely encapsulated lymphatic organs at the entrance of the gut and airways: Palatine tonsils: possess crypts, deep invaginations of stratified squamous epithelium of the covering tonsils; the crypts frequently contain debris. Some of lymphoid nodules in lamina propria have germinal centers (secondary nodules). The tonsils are separated from subjacent structure by a C.T. capsule. Pharyngeal tonsils: is a single tonsil located in the posterior wall of the nasopharynx covered by pseudostratified columnar epithelium. Lingual tonsils: are located on the dorsum of the posterior third of the tongue and are covered by a stratified non keratinized squamous epithelium. Ducts of the mucous lingual glands often open into the base of their crypts. MUCOSO-LYMPHOID ORGANS Tonsils branching crypt SSE Stratified Squamous Epithelium TONGUE: Lingual tonsils Lingual tonsil PALATINE deep Lingual mucous gland capsule cleft pseudostratified columnar epithelium PSCE Connective tissue PHARYNGEAL LINGUAL tonsil has SSE, but is shallow, wedged intermittently between the muscular & glandular tongue core and the dorsal posterior epithelium Muscular core LINGUAL tonsil has SSE, but is shallow, wedged intermittently between the muscular & glandular tongue core and the dorsal posterior epithelium 2. Peyer's patches: of the ileum have a distinctive structure, forming domelike structures extending into the lumen of the intestine. The bulk of the Peyer`s patches is B cells, organized in a large and highly active domed follicle. T cells occupy the areas between follicles. The antigen enters across a specialized epithelium made up of M cells. MUCOSO-LYMPHOID ORGANS Peyer’s patch V. APPENDIX ILEUM Peyer`s Patches Dome (M-cell) epithelium Villus Mantle zone Germinal center Solitary nodule/follicle Diffuse lymphoid tissue - T & B lymphocytes, Plasma cells, APCs, Ms 3. The appendix: The appendix is a short diverticulum arising from the blind terminus of the cecum. It has a narrow, irregular lumen, which often contains debris. The wall is thickened due to the presence of large aggregates of lymphoid nodules in the mucosa and even in submucosa (in middle aged and older individuals). Mucosa: VERMIFORM APPENDIX Simple columnar (contains surface columnar cells and goblet cells). Lamina propria displays numerous lymphoid nodules (capped by M cells) and lymphoid cells. It does not form villi but possess shallow crypts with some goblet cells, surface columnar cells and numerous enteroendocrine cells. Muscularis mucosa is composed of an inner circular and outer longitudinal layer of smooth muscle. Submucosa is composed of fibroelastic C.T. containing confluent lymphoid nodules and associated cells. Glands - thinned out Lamina propria Muscularis mucosae Tunica submucosa Lymphoid nodules in lamina propria and submucosa, often erasing the muscularis mucosae T muscularis externa - thin Tunica serosa & No villi Muscularis externa is composed of an inner circular and an outer longitudinal layer of smooth muscle. Serosa completely surrounds the appendix. B) Immune cells Lymphocytes In addition to the organized lymphoid tissue in which induction of immune responses occurs within the mucosal immune system, small foci of lymphocytes and plasma cells are scattered widely throughout the lamina propria of the gut wall. These represent the effector cells of the gut mucosal immune system. M (Microfold) cells: Site: they are specialized epithelial cells in the epithelium overlying the Peyer's patches. They are much less prominent than the absorptive gut epithelial cells (enterocytes). Shape and structure: they have microfolds on their luminal surface, instead of the microvilli present on the absorptive epithelial cells of the intestine. M cells lack a thick surface glycocalyx and do not secrete mucus. Hence they are adapted to interact directly with molecules and particles within the lumen of the gut. Function: they take up molecules and particles from the gut lumen by phagocytosis, then transported them through the interior of the cell to the basal cell membrane, where it is released into the extracellular space. This process is known as transcytosis. At their basal surface, the cell membrane of M cells is extensively folded around underlying lymphocytes and antigenpresenting cells, which take up the transported material, released from the M cells and process it for antigen presentation. Because M cells are much more accessible than enterocytes to particles within the gut, a number of pathogens target M cells to gain access to the subepithelial space, even though such pathogens then find themselves in the heart of the adaptive immune system of the intestine, the Peyer's patches. MUCOSAL IMMUNE DEFENSE Antigen Antigen M CELL APC Y M cells take up antigens from the lumen of the gut by endocytosis. The cell membrane at the base of these cells is folded around lymphocytes and dendritic cells within the Peyer's patches. T Y B Y B PROBLEM - Bugs in lumen, defensive cells below epithelium. Epithelium includes M cells to deliverantigen to APCs, & the main epithelial cells transport IgA from Plasma cells up to the lumen. P M (Microfold) cells Antigens are transported through M cells by the process of transcytosis and delivered directly to antigen-presenting cells and lymphocytes of the mucosal immune system. 3. Mast cell Two types of mast cells are recognized; those from connective tissue and a distinct set of mucosal mast cells (MMC). The activities of the latter are dependent on T-cells. Site: Mast cells are present in most tissues in the vicinity of blood vessels, and are especially prominent near the boundaries between the outside world and the internal milieu, such as the skin, mucosa of the lungs and digestive tract, as well as in the mouth, conjunctiva and nose. Structure: it possess a small oval pale staining nucleus and a cytoplasm filled with coarse deeply stained metachromatic granules. It has a well-developed golgi complex and RER. Function: Although best known for their role in allergy and anaphylaxis, mast cells play an important protective role as well, being intimately involved in wound healing and defense against pathogens. 4. Antigen Presenting Cells: Macrophages, Dendritic cells and B cells: Appendix Appendix Palatine Tonsil Lingual Tonsil