* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Genotype–phenotype correlations in laminopathies
Designer baby wikipedia , lookup
Public health genomics wikipedia , lookup
BRCA mutation wikipedia , lookup
Genome (book) wikipedia , lookup
Genetic code wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Population genetics wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
No-SCAR (Scarless Cas9 Assisted Recombineering) Genome Editing wikipedia , lookup
Tay–Sachs disease wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Koinophilia wikipedia , lookup
Microevolution wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Oncogenomics wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
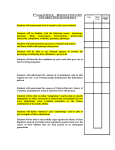
Nuclear Envelope Disease and Chromatin Organization 2009 Genotype–phenotype correlations in laminopathies: how does fate translate? Juergen Scharner, Viola F. Gnocchi, Juliet A. Ellis1 and Peter S. Zammit1 King’s College London, Randall Division of Cell and Molecular Biophysics, New Hunt’s House, Guy’s Campus, London SE1 1UL, U.K. Abstract A-type laminopathies are a group of diseases resulting from mutations in the intermediate filament proteins lamin A and C (both encoded by the LMNA gene), but for which the pathogenic mechanisms are little understood. In some laminopathies, there is a good correlation between the presence of a specific LMNA mutation and the disease diagnosed. In others however, many different mutations can give rise to the same clinical condition, even though the mutations may be distributed throughout one, or more, of the three functionally distinct protein domains of lamin A/C. Conversely, certain mutations can cause multiple laminopathies, with related patients carrying an identical mutation even having separate diseases, often affecting different tissues. Therefore clarifying genotype–phenotype links may provide important insights into both disease penetrance and mechanism. In the present paper, we review recent developments in genotype–phenotype correlations in laminopathies and discuss the factors that could influence pathology. Introduction Mutations in the LMNA gene cause a variety of diseases collectively called ‘laminopathies’. To date, more than 340 unique LMNA mutations (http://www.umd.be) [1] are known that cause 16 different diseases including A-EDMD (autosomal Emery–Dreifuss muscular dystrophy), DCM (dilated cardiomyopathy), LGMD1B (limb-girdle muscular dystrophy 1B), L-CMD (LMNArelated congenital muscular dystrophy), FPLD2 (familial partial lipodystrophy 2), HGPS (Hutchinson–Gilford progeria syndrome), atypical WRN (Werner syndrome), MAD (mandibuloacral dysplasia) and CMT2B (Charcot– Marie–Tooth disorder type 2B). The LMNA gene is alternatively spliced to produce the type V intermediate filament proteins lamin A, C, C2 and del10. Together with B-type lamins, lamin A and C are the major components of the nuclear lamina (a fibrous proteinaceous meshwork underlying the nuclear envelope). The nuclear lamina functions to maintain both nuclear and cellular architecture and plays a role in chromatin organization and gene expression [2]. The presence of mutant forms of lamin A/C is thought to perturb some, or all, of these functions of the nuclear lamina, but it is generally unclear how specific mutations result in a particular laminopathy. Phenotypic clustering, the Key words: autosomal Emery–Dreifuss muscular dystrophy (A-EDMD), dilated cardiomyopathy (DCM), familial partial lipodystrophy 2 (FPLD2), Hutchinson–Gilford progeria syndrome (HGPS), lamin, laminopathy, LMNA, limb-girdle muscular dystrophy 1B (LGMD1B). Abbreviations used: A-EDMD, autosomal Emery–Dreifuss muscular dystrophy; CMT2B, Charcot– Marie–Tooth disorder type 2B; DCM, dilated cardiomyopathy; FPLD2, familial partial lipodystrophy 2; HGPS, Hutchinson–Gilford progeria syndrome; L-CMD, LMNA-related congenital muscular dystrophy; LGMD1B, limb-girdle muscular dystrophy 1B; MAD, mandibuloacral dysplasia; SNP, single nucleotide polymorphism; SREBP, sterol-regulatory-element-binding protein; WRN, Werner syndrome. 1 Correspondence may be addressed to either of these authors (email [email protected] or [email protected]). Biochem. Soc. Trans. (2010) 38, 257–262; doi:10.1042/BST0380257 systematic correlation of phenotype with genotype, is becoming increasingly important to understand underlying mechanisms of monogenic diseases [3–5]. Here, we review the correlation of LMNA mutation with clinical diagnosis, to explore genotype–phenotype links within laminopathies (Figure 1). Laminopathies with a more consistent genotype–phenotype link To date, mutations distributed throughout the gene and affecting almost 20% of the coding sequence of LMNA have been reported from more than 1000 patients, and arise mainly from missense or frameshift mutations (http://www.umd.be) [1]. In some laminopathies such as HGPS, ‘hot-spot’ or founder mutations result in a similar phenotype. HGPS is almost always caused by the de novo base mutation c.1824C>T/p.G608G, which results in a cryptic splice donor site in the lamin A-specific exon 11, and deletion of the remaining 50 amino acids of the C-terminus [6]. The resulting truncated protein (termed progerin) retains the CAAX box but lacks the endoproteolytic cleavage site, so it cannot be processed by Zmpste24, and is incorporated into the nuclear lamina carrying the C-terminal farnesyl group. Two unrelated patients with severe forms of HGPS have recently been reported carrying two new mutations (c.1968+1G>A and c.1821G>A), but both cause a frequent use of the splice donor site that is activated in typical HGPS patients [7]. Other laminopathies also appear to arise from a common LMNA mutation, such as WRN (R133L), CMT2B (R298C) and MAD (R527H) (although R133L also causes FPLD2, and R527H additionally results in A-EDMD) (Figure 1) [8]. Although the number of patients developing HGPS, WRN, CMT2B or MAD is small, it is likely that the presence of a particular mutation will have a predictive value on the C The C 2010 Biochemical Society Authors Journal compilation 257 258 Biochemical Society Transactions (2010) Volume 38, part 1 Figure 1 Distribution of lamin A mutations and their related laminopathies (a) Schematic diagram of the LMNA gene, with exons encoding their respective protein domains colour coded and the lamin A splice site indicated in red above. HGPS mutations causing a new splice donor site are indicated in black boxes. (b) The lamin A protein with mutations indicated that result in A-EDMD (blue), DCM (green), LGMD1B (black), L-CMD (gold), FPLD2 (red) and CMT2B (plum). ‘†’ indicates that the same amino acid change causes different laminopathies. *R133L also causes WRN, *S143F additionally results in HGPS, *R527H causes MAD too and *R644C also gives rise to a range of other disorders [26–29]. ◦ Patients carrying R527C develop either a severe form of MAD and/or progeria [52,53]. Mutation/laminopathy correlations are from [1,9]. Interacting proteins and their corresponding binding regions on lamin A are indicated below [54]. clinical diagnosis and that the pathogenic mechanism will be similar for a given disorder (Figure 2a). Importantly, these disorders are characterized by systemic effects, with many tissues affected, unlike the more common laminopathies. Laminopathies with an inconsistent genotype–phenotype link By contrast, laminopathies with striated muscle involvement (A-EDMD, LGMD1B, L-CMD and DCM), together accounting for ∼60% of all laminopathies, along with those affecting adipose tissue (FPLD2), are caused by a large number of different mutations (Figure 1). A-EDMD (blue in Figure 1) and L-CMD (gold in Figure 1) mutations are distributed throughout the gene, whereas LGMD1B (black in Figure 1) mutations tend to cluster in both the Ig-like fold and coil 2 [1,9]. DCM (green in Figure 1) patients tend to carry mutations throughout the rod domain and can share clinical characteristics with A-EDMD patients, where an isolated cardiac involvement has been described. For FPLD2, there is an apparent ‘hot spot’ for mutations in the Ig-like fold where 75% C The C 2010 Biochemical Society Authors Journal compilation of all mutations occur. The remaining 25% are distributed throughout the protein and are distinct from those causing A-EDMD (Figure 1). Interestingly, muscle involvement has not been observed in FPLD2 patients. The C-terminal domain of lamin A binds SREBP1 (sterol-regulatoryelement-binding protein 1) and SREBP2, which play a key role in adipocyte differentiation and cholesterol biosynthesis respectively [10]. Thus certain mutations may disrupt lamin A–SREBP1/2 interactions to specifically affect adipocyte function. Phenotypic clustering using mutation type Bonne et al. [11] first attempted a genotype–phenotype correlation by mutation type in LMNA. Of the 53 patients analysed, all 12 with isolated heart involvement carried a nonsense mutation in Q6X of the head domain. In the remaining 41 patients with muscle weakness however, attempts to correlate disease severity with the protein domain affected by the missense mutations proved inconclusive. Our own analysis of LMNA patients (http://www.interfil.org) Nuclear Envelope Disease and Chromatin Organization 2009 Figure 2 Modes of LMNA genotype–phenotype correlation (a) A consistent genotype–phenotype correlation indicates a likely common disease mechanism. (b) LMNA mutations distributed throughout the protein can each cause a particular laminopathy. Some groups of mutations probably have a common disease mechanism, while other mutations appear to operate by separate pathways to cause the same laminopathy. (c) Specific LMNA mutations combined with LMNA SNPs, or mutations/SNPs in other proteins, act through combined mechanisms to cause modified phenotypes, such as atypical laminopathies or different laminopathies in individual patients carrying identical mutations. the domain surface without affecting structural integrity: with R482W, for example, not changing the crystal structure of the mutant protein [13–15]. However, tetrameric aggregates of mutant molecules were found that did not occur in the original structure, such that R482W or R482Q might cause an allosteric effect, allowing the repositioning of the C-terminal β-strand g , leading to a novel aggregation state and so possibly contributing to disease [13]. A similar phenomenon occurs with the F12L mutation in porphobilinogen synthase, which initiates a transition of the aggregation state, significantly changing the enzyme kinetics [16]. Certain mutations, therefore, could have a common mechanism to cause a particular laminopathy, but it is less clear how mutations located in functionally distinct protein domains could operate by the same disease mechanism (Figures 1 and 2b). Differential effects of LMNA mutations in post-mitotic cells compared with dividing cells [1] with frameshift mutations found that 62% (18/29) developed DCM, again associating DCM with truncated protein species (J. Scharner, V. Gnocchi, J.A. Ellis and P.S. Zammit, unpublished work). Benedetti et al. [12] separated neuromuscular patients according to the age of disease onset. The type of LMNA mutation differed, such that 89% (17/19) early-onset patients carried missense mutations and in-frame deletions, while only 63% (5/8) of late-onset patients did. The remaining three late-onset patients had frameshift mutations, presumably resulting in a truncated protein. Interestingly, variants associated with early onset were primarily found in the Ig-like fold (35%) and in coil 2A (24%), while variants associated with late onset mainly occurred in coil 2B (60%) [12]. These results indicate that the underlying disease mechanism may be associated with the functional properties of the affected protein domain rather than with the type of mutation. Structural changes of mutant lamin A in A-EDMD, but not in FPLD2 Mutations in the Ig-like fold provide evidence of a genotype– phenotype correlation [13,14]. This globular region in the C-terminal domain harbours both A-EDMD (e.g. R453W and R572P) and FPLD2 (e.g. R482W, R482Q and K486N), causing mutations in close proximity (Figure 1). Mutations causing laminopathies with striated muscle involvement occur at positions that play a critical role in the structural stability of the C-terminal domain. Conversely, those that lead to FPLD2 result from a lost positive charge on An LMNA mutation causing A-EDMD (R453W) perturbs myogenic differentiation, while an FPLD2-causing mutation (R482W) does not, again suggesting that certain mutations can have tissue-specific effects [17]. Many LMNA mutations probably have common effects, including compromised nuclear integrity and transcriptional regulation, but some may also have additional actions. Particular mutant lamin A variants delay cell cycle progression by prolonging S-phase [18], and some also hinder the exit from cell cycle and/or the nuclear rearrangements, required for myogenic differentiation in immortalized cell lines [17,19]. The functional cells of cardiac muscle, skeletal muscle and adipose tissue are post-mitotic, but skeletal muscle retains a well-characterized stem cell compartment, responsible for homoeostatic myonuclear turnover, hypertrophy and repair [20]. Thus skeletal muscle may additionally be vulnerable to mutations that also affect cell cycle and/or differentiation of myogenic stem cells. Such a mutation, therefore, may not only influence the onset and severity of A-EDMD [21] or produce L-CMD [9], but even influence which tissue is affected and so the type of laminopathy caused. Lamin A or lamin C or both? Since LMNA is alternatively spliced [22], another way to classify mutations is whether they affect both lamin A and lamin C or just one protein. Of the 12 exons in LMNA, exons 11 and 12 are specific to lamin A, while alternative splicing at codon 566 in exon 10 gives lamin C, a unique exon coding for six amino acid residues (Figure 1). As expected given its size, only two mutations, R571S causing DCM [23] and R571C causing muscular dystrophy with axonal neuropathy [24], have been associated with the lamin C-specific tail. Exon 12 encodes eight amino acids that are cleaved during posttranslational modification of prelamin A, so unless mutations affect prelamin A processing, they would not be expected to affect lamin A function. Interestingly, few mutations occur in lamin A-specific exon 11 and those that do are less C The C 2010 Biochemical Society Authors Journal compilation 259 260 Biochemical Society Transactions (2010) Volume 38, part 1 associated with skeletal muscle involvement: for example, of 18 mutations in exon 11 [1], 56% (10/18) cause DCM and 33% (6/18) result in FPLD2, with only one each causing A-EDMD or LGMD1B (J. Scharner, V. Gnocchi, J.A. Ellis and P.S. Zammit, unpublished work). It is worth noting that as HGPS predominately, but not exclusively, targets lamin A and generates the most severe laminopathy, it has been interpreted as being the more important protein. However, the apparent normal phenotype of the lmnaLCO/LCO mouse, where lamin C is the only A-type lamin present, suggests that both lamin A and the other isoforms are dispensable [25]. Effect of modifying genes and SNPs (single nucleotide polymorphisms) on phenotypic variability in laminopathies Patients carrying, for example, the R644C mutation have a range of clinical conditions including DCM, LGMD2B, atypical HGPS, lipodystrophy etc. [26–29]. This extreme phenotypic variability indicates that genetic background contributes to the disease diagnosed [29]. Furthermore, a single mutation can result in DCM either with or without A-EDMD. This provides evidence of epistasis, i.e. effects of the mutated LMNA gene are altered by one or more other genes, the so-called modifying genes (Figure 2c). There are, indeed, rare examples of where an additional mutation in either desmin or emerin results in a more severe disease than might be expected from the LMNA mutation alone [30]. Where patients carry two different pathogenic LMNA mutations, it is not unexpected that they develop a more severe phenotype [31]. However, LMNA also contains SNPs with no apparent pathological phenotype: of 40 on the Leiden Open Variation Database (www.dmd.nl/lmna_seqvar.html), 75% (30/40) are silent mutations, and the rest are missense mutations affecting the head (one), central rod (three) or tail (six) domains (J. Scharner, V. Gnocchi, J.A. Ellis and P.S. Zammit, unpublished work). Depending on the context however, these mutations can cause disease: T528M or M540T alone appear non-pathogenic, but when inherited together, they result in an apparently typical HGPS but without prelamin A accumulation [32]. Certainly, a particular LMNA pathogenic mutation/SNP combination can increase the penetrance of a phenotype, which offers an explanation for intra- and inter-familiar variations [33], but may also alter the clinical condition diagnosed: while the S583L mutation normally causes FPLD2, when present with T528M it results in FPLD1 [34]. Modifying genes/SNPs are likely to explain inconclusive attempts to associate mutation with laminopathy (Figure 2c), where, for example, a single mutation has been reported to express phenotypic variability, such as with R60G, Y267C, R377H/L and R644C (Figure 1). Mouse models of laminopathies Modelling diseases in mice is a powerful technology to explore genotype–phenotype correlations, disease mechanisms C The C 2010 Biochemical Society Authors Journal compilation and potential therapies. The majority of laminopathies arise from missense and frameshift mutations, but two nonsense mutations have been reported: patients heterozygous for Y259X have LGMD1B [35], but those heterozygous for Q6X develop DCM [36,37] and mice heterozygous for the targeted lmna null allele also develop a DCM phenotype [38]. The only LMNA-null homozygous subject identified carried Y259X and died at birth, and lmna−/− mice are characterized by postnatal growth retardation, muscular dystrophy, rapidly progressive DCM and death by 4–8 weeks of age [39,40]. In humans, both the L530P and H222P mutations cause A-EDMD. The H222P mouse recapitulates features of A-EDMD [41], while L530P causes a phenotype akin to HGPS, possibly due to the unintentional inclusion of an additional splicing defect in the C-terminus [42]. The N195K mutation causes DCM in humans and a DCM-like phenotype in mice [43]. Importantly, the L530P, H222P and N195K mouse models only show a phenotype when homozygous for the mutant alides, in contrast with the heterozygous state in patients. DCM with A-EDMD resulting from the M371K mutation also causes a heart phenotype in transgenic mice when under a heart-specific promoter [44]. Collectively, these mutant mice illustrate that aspects of human laminopathies can be successfully modelled in mice, with all the attendant advantages over experimenting on rare patient samples, but again emphasizes that genetic background exerts an influence on the penetrance of the condition, whether in mice or humans. Conclusions and perspectives It must be remembered that laminopathies are rare diseases, and in many cases there are very few patients with a particular mutation(s). That said, what can be concluded about genotype–phenotype correlations? In laminopathies such as HGPS, there is a high degree of consistency in the underlying mutation between patients, meaning that the disease mechanism is likely to be common to that particular disorder. There is also a degree of genotype–phenotype correlation in FPLD2 for example, where many mutations are in the Ig-like fold and so could have a common disease mechanism, although the rest give little clue as to why they cause this condition. For others however, including DCM, A-EDMD and LGMD1B, there is a much weaker correlation between mutation and disease (Figure 2). A-EDMD and FPLD2 may differ owing to the degree to which a particular mutation affects lamin A/C structure, but this does not, for example, explain how different amino acid substitutions lead to a specific phenotype. It should also be remembered that lamins A and C are distinct proteins and mutations in the common region of LMNA would generate two distinct mutated proteins that could function differently to cause disease and so need to be treated as individual entities [45]. Where a more severe or unexpected phenotype is found with a particular LMNA mutation, a number of factors may be contributing. Whether a mutation also affects cell cycle and differentiation, in addition to nuclear structure, chromosome Nuclear Envelope Disease and Chromatin Organization 2009 organization or transcriptional regulation, could certainly contribute to disease onset and severity, but maybe even the laminopathy diagnosed. The emerging evidence of modifying genes and SNPs affecting laminopathies means that, in future, it would be helpful if clinical data were to include the LMNAspecific SNPs, to determine if disease severity/diagnosis can be linked to certain mutation/SNP combinations. Screening LMNA for SNPs is also being used in non-laminopathies with overlapping phenotypes, to determine whether there is any correlation with disease severity [46]. Ultimately, genomewide sequencing would be needed to check for mutations in all regulatory regions of LMNA and fully explore the correlation with modifying genes. Finally, EDMD is divided into A-EDMD, and X-linked EDMD caused by mutations in EMD, but together these account for only ∼50% [47] of clinically diagnosed EDMD. Assuming that LMNA mutations/SNPs have not been overlooked, mutations in other genes may also result in disorders with a similar phenotype [48]. Indeed, it was recently shown that mutations in LAP2α can cause a condition similar to DCM [49], whereas mutations in SYNE1 or FHL1 produce an EDMD-like phenotype [50,51]. Funding J.S. is supported by a Ph.D. studentship funded by the Biomedical and Health School, King’s College London, and V.F.G. is funded by The Medical Research Council [grant number G0700307]. The P.S.Z. laboratory is supported by The Muscular Dystrophy Campaign, The Wellcome Trust and OPTISTEM (contract 223098), through the European Union 7th Framework Programme. References 1 Szeverenyi, I., Cassidy, A.J., Chung, C.W., Lee, B.T., Common, J.E., Ogg, S.C., Chen, H., Sim, S.Y., Goh, W.L., Ng, K.W. et al. (2008) The Human Intermediate Filament Database: comprehensive information on a gene family involved in many human diseases. Hum. Mutat. 29, 351–360 2 Broers, J.L., Ramaekers, F.C., Bonne, G., Yaou, R.B. and Hutchison, C.J. (2006) Nuclear lamins: laminopathies and their role in premature ageing. Physiol. Rev. 86, 967–1008 3 Freimer, N. and Sabatti, C. (2003) The human phenome project. Nat. Genet. 34, 15–21 4 Hegele, R. (2005) LMNA mutation position predicts organ system involvement in laminopathies. Clin. Genet. 68, 31–34 5 Scriver, C.R. (2004) After the genome – the phenome? J. Inherit. Metab. Dis. 27, 305–317 6 Eriksson, M., Brown, W.T., Gordon, L.B., Glynn, M.W., Singer, J., Scott, L., Erdos, M.R., Robbins, C.M., Moses, T.Y., Berglund, P. et al. (2003) Recurrent de novo point mutations in lamin A cause Hutchinson–Gilford progeria syndrome. Nature 423, 293–298 7 Moulson, C.L., Fong, L.G., Gardner, J.M., Farber, E.A., Go, G., Passariello, A., Grange, D.K., Young, S.G. and Miner, J.H. (2007) Increased progerin expression associated with unusual LMNA mutations causes severe progeroid syndromes. Hum. Mutat. 28, 882–889 8 Ben Yaou, R., Muchir, A., Arimura, T., Massart, C., Demay, L., Richard, P. and Bonne, G. (2005) Genetics of laminopathies. Novartis Found. Symp. 264, 81–90 9 Quijano-Roy, S., Mbieleu, B., Bonnemann, C.G., Jeannet, P.Y., Colomer, J., Clarke, N.F., Cuisset, J.M., Roper, H., De Meirleir, L., D’Amico, A. et al. (2008) De novo LMNA mutations cause a new form of congenital muscular dystrophy. Ann. Neurol. 64, 177–186 10 Lloyd, D.J., Trembath, R.C. and Shackleton, S. (2002) A novel interaction between lamin A and SREBP1: implications for partial lipodystrophy and other laminopathies. Hum. Mol. Genet. 11, 769–777 11 Bonne, G., Mercuri, E., Muchir, A., Urtizberea, A., Becane, H.M., Recan, D., Merlini, L., Wehnert, M., Boor, R., Reuner, U. et al. (2000) Clinical and molecular genetic spectrum of autosomal dominant Emery–Dreifuss muscular dystrophy due to mutations of the lamin A/C gene. Ann. Neurol. 48, 170–180 12 Benedetti, S., Menditto, I., Degano, M., Rodolico, C., Merlini, L., D’Amico, A., Palmucci, L., Berardinelli, A., Pegoraro, E., Trevisan, C.P. et al. (2007) Phenotypic clustering of lamin A/C mutations in neuromuscular patients. Neurology 69, 1285–1292 13 Dhe-Paganon, S., Werner, E.D., Chi, Y.I. and Shoelson, S.E. (2002) Structure of the globular tail of nuclear lamin. J. Biol. Chem. 277, 17381–17384 14 Krimm, I., Ostlund, C., Gilquin, B., Couprie, J., Hossenlopp, P., Mornon, J.P., Bonne, G., Courvalin, J.C., Worman, H.J. and Zinn-Justin, S. (2002) The Ig-like structure of the C-terminal domain of lamin A/C, mutated in muscular dystrophies, cardiomyopathy, and partial lipodystrophy. Structure 10, 811–823 15 Magracheva, E., Kozlov, S., Stewart, C.L., Wlodawer, A. and Zdanov, A. (2009) Structure of the lamin A/C R482W mutant responsible for dominant familial partial lipodystrophy (FPLD). Acta Crystallogr. Sect. F Struct. Biol. Cryst. Commun. 65, 665–670 16 Breinig, S., Kervinen, J., Stith, L., Wasson, A.S., Fairman, R., Wlodawer, A., Zdanov, A. and Jaffe, E.K. (2003) Control of tetrapyrrole biosynthesis by alternate quaternary forms of porphobilinogen synthase. Nat. Struct. Biol. 10, 757–763 17 Favreau, C., Higuet, D., Courvalin, J.C. and Buendia, B. (2004) Expression of a mutant lamin A that causes Emery–Dreifuss muscular dystrophy inhibits in vitro differentiation of C2C12 myoblasts. Mol. Cell. Biol. 24, 1481–1492 18 Emerson, L.J., Holt, M.R., Wheeler, M.A., Wehnert, M., Parsons, M. and Ellis, J.A. (2009) Defects in cell spreading and ERK1/2 activation in fibroblasts with lamin A/C mutations. Biochim. Biophys. Acta 1792, 810–821 19 Markiewicz, E., Ledran, M. and Hutchison, C.J. (2005) Remodelling of the nuclear lamina and nucleoskeleton is required for skeletal muscle differentiation in vitro. J. Cell Sci. 118, 409–420 20 Zammit, P.S. (2008) All muscle satellite cells are equal, but are some more equal than others? J. Cell Sci. 121, 2975–2982 21 Gnocchi, V.F., Ellis, J.A. and Zammit, P.S. (2008) Does satellite cell dysfunction contribute to disease progression in Emery–Dreifuss muscular dystrophy? Biochem. Soc. Trans. 36, 1344–1349 22 Lin, F. and Worman, H.J. (1993) Structural organization of the human gene encoding nuclear lamin A and nuclear lamin C. J. Biol. Chem. 268, 16321–16326 23 Fatkin, D., MacRae, C., Sasaki, T., Wolff, M.R., Porcu, M., Frenneaux, M., Atherton, J., Vidaillet, Jr, H.J., Spudich, S. et al. (1999) Missense mutations in the rod domain of the lamin A/C gene as causes of dilated cardiomyopathy and conduction-system disease. N. Engl. J. Med. 341, 1715–1724 24 Benedetti, S., Bertini, E., Iannaccone, S., Angelini, C., Trisciani, M., Toniolo, D., Sferrazza, B., Carrera, P., Comi, G., Ferrari, M. et al. (2005) Dominant LMNA mutations can cause combined muscular dystrophy and peripheral neuropathy. J. Neurol. Neurosurg. Psychiatry 76, 1019–1021 25 Fong, L.G., Ng, J.K., Lammerding, J., Vickers, T.A., Meta, M., Cote, N., Gavino, B., Qiao, X., Chang, S.Y., Young, S.R. et al. (2006) Prelamin A and lamin A appear to be dispensable in the nuclear lamina. J. Clin. Invest. 116, 743–752 26 Brown, C.A., Lanning, R.W., McKinney, K.Q., Salvino, A.R., Cherniske, E., Crowe, C.A., Darras, B.T., Gominak, S., Greenberg, C.R., Grosmann, C. et al. (2001) Novel and recurrent mutations in lamin A/C in patients with Emery–Dreifuss muscular dystrophy. Am. J. Med. Genet. 102, 359–367 27 Csoka, A.B., Cao, H., Sammak, P.J., Constantinescu, D., Schatten, G.P. and Hegele, R.A. (2004) Novel lamin A/C gene (LMNA) mutations in atypical progeroid syndromes. J. Med. Genet. 41, 304–308 28 Mercuri, E., Brown, S.C., Nihoyannopoulos, P., Poulton, J., Kinali, M., Richard, P., Piercy, R.J., Messina, S., Sewry, C., Burke, M.M. et al. (2005) Extreme variability of skeletal and cardiac muscle involvement in patients with mutations in exon 11 of the lamin A/C gene. Muscle Nerve 31, 602–609 29 Rankin, J., Auer-Grumbach, M., Bagg, W., Colclough, K., Nguyen, T.D., Fenton-May, J., Hattersley, A., Hudson, J., Jardine, P., Josifova, D. et al. (2008) Extreme phenotypic diversity and nonpenetrance in families with the LMNA gene mutation R644C. Am. J. Med. Genet. A 146, 1530–1542 C The C 2010 Biochemical Society Authors Journal compilation 261 262 Biochemical Society Transactions (2010) Volume 38, part 1 30 Muntoni, F., Bonne, G., Goldfarb, L.G., Mercuri, E., Piercy, R.J., Burke, M., Yaou, R.B., Richard, P., Recan, D., Shatunov, A. et al. (2006) Disease severity in dominant Emery Dreifuss is increased by mutations in both emerin and desmin proteins. Brain 129, 1260–1268 31 Hegele, R.A., Cao, H., Anderson, C.M. and Hramiak, I.M. (2000) Heterogeneity of nuclear lamin A mutations in Dunnigan-type familial partial lipodystrophy. J. Clin. Endocrinol. Metab. 85, 3431–3435 32 Verstraeten, V.L., Broers, J.L., van Steensel, M.A., Zinn-Justin, S., Ramaekers, F.C., Steijlen, P.M., Kamps, M., Kuijpers, H.J., Merckx, D., Smeets, H.J. et al. (2006) Compound heterozygosity for mutations in LMNA causes a progeria syndrome without prelamin A accumulation. Hum. Mol. Genet. 15, 2509–2522 33 Ellis, J.A. (2006) Emery–Dreifuss muscular dystrophy at the nuclear envelope: 10 years on. Cell. Mol. Life Sci. 63, 2702–2709 34 Savage, D.B., Soos, M.A., Powlson, A., O’Rahilly, S., McFarlane, I., Halsall, D.J., Barroso, I., Thomas, E.L., Bell, J.D., Scobie, I. et al. (2004) Familial partial lipodystrophy associated with compound heterozygosity for novel mutations in the LMNA gene. Diabetologia 47, 753–756 35 van Engelen, B.G., Muchir, A., Hutchison, C.J., van der Kooi, A.J., Bonne, G. and Lammens, M. (2005) The lethal phenotype of a homozygous nonsense mutation in the lamin A/C gene. Neurology 64, 374–376 36 Bonne, G., Di Barletta, M.R., Varnous, S., Becane, H.M., Hammouda, E.H., Merlini, L., Muntoni, F., Greenberg, C.R., Gary, F., Urtizberea, J.A. et al. (1999) Mutations in the gene encoding lamin A/C cause autosomal dominant Emery–Dreifuss muscular dystrophy. Nat. Genet. 21, 285–288 37 Becane, H.M., Bonne, G., Varnous, S., Muchir, A., Ortega, V., Hammouda, E.H., Urtizberea, J.A., Lavergne, T., Fardeau, M., Eymard, B. et al. (2000) High incidence of sudden death with conduction system and myocardial disease due to lamins A and C gene mutation. Pacing Clin. Electrophysiol. 23, 1661–1666 38 Wolf, C.M., Wang, L., Alcalai, R., Pizard, A., Burgon, P.G., Ahmad, F., Sherwood, M., Branco, D.M., Wakimoto, H., Fishman, G.I. et al. (2008) Lamin A/C haploinsufficiency causes dilated cardiomyopathy and apoptosis-triggered cardiac conduction system disease. J. Mol. Cell. Cardiol. 44, 293–303 39 Sullivan, T., Escalante-Alcalde, D., Bhatt, H., Anver, M., Bhat, N., Nagashima, K., Stewart, C.L. and Burke, B. (1999) Loss of A-type lamin expression compromises nuclear envelope integrity leading to muscular dystrophy. J. Cell Biol. 147, 913–920 40 Nikolova, V., Leimena, C., McMahon, A.C., Tan, J.C., Chandar, S., Jogia, D., Kesteven, S.H., Michalicek, J., Otway, R., Verheyen, F. et al. (2004) Defects in nuclear structure and function promote dilated cardiomyopathy in lamin A/C-deficient mice. J. Clin. Invest. 113, 357–369 41 Arimura, T., Helbling-Leclerc, A., Massart, C., Varnous, S., Niel, F., Lacene, E., Fromes, Y., Toussaint, M., Mura, A.M., Keller, D.I. et al. (2005) Mouse model carrying H222P-Lmna mutation develops muscular dystrophy and dilated cardiomyopathy similar to human striated muscle laminopathies. Hum. Mol. Genet. 14, 155–169 C The C 2010 Biochemical Society Authors Journal compilation 42 Mounkes, L.C., Kozlov, S., Hernandez, L., Sullivan, T. and Stewart, C.L. (2003) A progeroid syndrome in mice is caused by defects in A-type lamins. Nature 423, 298–301 43 Mounkes, L.C., Kozlov, S.V., Rottman, J.N. and Stewart, C.L. (2005) Expression of an LMNA-N195K variant of A-type lamins results in cardiac conduction defects and death in mice. Hum. Mol. Genet. 14, 2167–2180 44 Wang, Y., Herron, A.J. and Worman, H.J. (2006) Pathology and nuclear abnormalities in hearts of transgenic mice expressing M371K lamin A encoded by an LMNA mutation causing Emery–Dreifuss muscular dystrophy. Hum. Mol. Genet. 15, 2479–2489 45 Motsch, I., Kaluarachchi, M., Emerson, L.J., Brown, C.A., Brown, S.C., Dabauvalle, M.C. and Ellis, J.A. (2005) Lamins A and C are differentially dysfunctional in autosomal dominant Emery–Dreifuss muscular dystrophy. Eur. J. Cell Biol. 84, 765–781 46 Gaudy-Marqueste, C., Boyer, A., Navarro, C., Rouzier, C., Harley, J.R., Weiller, P.J., Grob, J.J., Levy, N. and De Sandre-Giovannoli, A. (2009) LMNA, ZMPSTE24, and LBR are not mutated in Scleroderma. Genet. Test. Mol. Biomarkers 13, 635–639 47 Cohen, T.V. and Stewart, C.L. (2008) Fraying at the edge: mouse models of diseases resulting from defects at the nuclear periphery. Curr. Top. Dev. Biol. 84, 351–384 48 Stewart, C.L., Kozlov, S., Fong, L.G. and Young, S.G. (2007) Mouse models of the laminopathies. Exp. Cell Res. 313, 2144–2156 49 Taylor, M.R., Slavov, D., Gajewski, A., Vlcek, S., Ku, L., Fain, P.R., Carniel, E., Di Lenarda, A., Sinagra, G., Boucek, M.M. et al. (2005) Thymopoietin (lamina-associated polypeptide 2) gene mutation associated with dilated cardiomyopathy. Hum. Mutat. 26, 566–574 50 Zhang, Q., Bethmann, C., Worth, N.F., Davies, J.D., Wasner, C., Feuer, A., Ragnauth, C.D., Yi, Q., Mellad, J.A., Warren, D.T. et al. (2007) Nesprin-1 and -2 are involved in the pathogenesis of Emery–Dreifuss muscular dystrophy and are critical for nuclear envelope integrity. Hum. Mol. Genet. 16, 2816–2833 51 Gueneau, L., Bertrand, A.T., Jais, J.P., Salih, M.A., Stojkovic, T., Wehnert, M., Hoeltzenbein, M., Spuler, S., Saitoh, S., Verschueren, A. et al. (2009) Mutations of the FHL1 gene cause Emery–Dreifuss muscular dystrophy. Am. J. Hum. Genet. 85, 338–353 52 Cao, H. and Hegele, R.A. (2003) LMNA is mutated in Hutchinson–Gilford progeria (MIM 176670) but not in Wiedemann–Rautenstrauch progeroid syndrome (MIM 264090). J. Hum. Genet. 48, 271–274 53 Agarwal, A.K., Kazachkova, I., Ten, S. and Garg, A. (2008) Severe mandibuloacral dysplasia-associated lipodystrophy and progeria in a young girl with a novel homozygous Arg527Cys LMNA mutation. J. Clin. Endocrinol. Metab. 93, 4617–4623 54 Schirmer, E.C. and Foisner, R. (2007) Proteins that associate with lamins: many faces, many functions. Exp. Cell Res. 313, 2167–2179 Received 28 August 2009 doi:10.1042/BST0380257