* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Inducibility and Expression of Microvascular
Survey
Document related concepts
Transcript
Inducibility and Expression of Microvascular
Endothelial Adhesion Molecules in Lesional,
Perilesional, and Uninvolved Skin of Psoriatic Patients
Peter Petzelbauer, Jordan S. Pober, Agnes Keh,* and Irwin M. Braverman*
Boyer Center for Molecular Medicine and - D epartment of D ermatolo gy, Yale University School of M edicine, New Haven,
Connecticut, U.S.A.
Previous studies have demonstrated 1) that patterns of
inducible endothelial cell expression of endothelial
leukocyte adhesion molecule-l (ELAM-l) and vascular
cell adhesion molecule-l (VCAM-l) in response to cytokines varies both with anatomic position within the
dermal microvasculature and with the presence of
perivascular inflammatory infiltrates, and 2) that the
anatomic architecture of the dermal superficial plexus
(SVP) is altered in inflamed lesional but not in univolved skin of psoriatic patients. The present study was
designed to evaluate the pattern of cytokine inducibility ofELAM-l and VCAM-l in altered dermal microvessels of psoriatic patients. At the light microscope
level, preculture biopsies of uninvolved and perilesional skin were indistinguishable by morphology and
ELAM-l and VCAM-l expression were virtually absent. In contrast, biopsied lesional skin showed elongated capillary loops and increased numbers ofT cells
compared to uninvolved and perilesional skin. The
dermal microvasculature of the SVP of lesional skin
contained ELAM-l+ in 29.4% of vessels and VCAM-l+
endothelial cells in 8.7% of vessels. After 24 h of organ
culture in medium supplemented with tumor necrosis
factor and interleukin-4, ELAM-l + endothelial cells in
the SVP were increased significantly in uninvolved
(from mean 0.5% to 27% of vessels), perilesional (from
mean 5.5% to 41.8% of vessels), and lesional skin (from
mean 29.4% to 45.7% of vessels) . VCAM-l was not inducible on SVP endothelial cells in uninvolved skin
but VCAM- l+ endothelial cells were increased significantly in perilesional (from mean 0.7% to 23.7% of
vessels) and lesional skin (from mean 8.7% to 41.4% of
vessels). In uninvolved and perilesional skin ELAM-l
and VCAM-l were confined to endothelial cells below
the rete. In contrast, endothelial cells of the intrapapillary part of the capillary loop oflesional skin became
cytokine responsive, in that ELAM-l and VCAM-l
could be induced at this site. By immunoelectron microscopy, expression was most intense on the luminal
surface of venular endothelial cells and at the inter endothelial junctions. In conclusion, we have presented
evidence that the cytokine responsiveness of microvascular endothelial cells is altered in psoriasis in a pattern
that may explain both the circumscribed nature and
the epidermal involvement of the psoriatic plaque. Key
words: ELAM-1 / VCAM-1 / organ culture/ superficial vascular plexus.] Invest DermatoI103:300-305, 1994
icrovascular endothelial cells of human skin contribute to the recruitment of inflammatory leukocytes by expressing inducible leukocyte adhesion
molecules such as endothelial leukocyte adhesion
molecule-1 (ELAM-l, also called E-selectin) , vascular cell adhesion molecule-1 (VCAM-1), and intercell ular adhesion molecule-l (ICAM-1 , also called CD54). ELAM- l appears
particularly important in the recruitment of neutrophils and may
also participate in recruitment of other leukocytes such as inflammatory T cell s and monocytes [1,2]. VCAM-l contributes to selective recruitment of T cells and eosinophils but not neutrophils
[1 ,3,4]. Elevated IC AM-1 also appears more closely associated with
T-cell infiltration ill lIillo [5,6]' but also contributes to neutrophil
adhesion and transmigration in vitro [1,7]. I " vivo as well as cell and
organ-culture experiments have identified inflammatory cytokines,
including interleukin (IL)-l, tumor necrosis factor (TNF), interferon (IFN)-y, and IL-4, as the major signals that induce the expression of these adhesion mo lecules [8 - 15]. Furthermore, skin organculture experiments have revealed that the responsiveness of
microvascular endothelial cells to cytokines varies with anatomic
position. Specifically, in the superficial vascular plexus (SVP),
inducible ELAM-1 expression is largely confined to the venules of
the horizontal plexus and the venular portions of the capillary
loops, i.e. , that portion below the level of the rete just proximal to anastomosis with the horizontal vessels [15]. TNF and IL-l
are the most potent signals for induction ofELAM-l. VCAM-l , in
normal skin, is not inducible on endothelial cells of the SVP by any
combination of cytokines and its expression is confined largely to
vessels of the deep vascular plexus. In organ-cultured acutely inflamed skin, ELAM-l is basally expressed and VCAM-l becomes
inducible on SVP venular endothelial cells by a combination
of TNF and IL-4. Even in dermatitis, these adhesion molecules
M
Manuscript received N ovember 10 , 1993; accepted for publication March
28, 1994.
Reprint requests to: Dr. Peter Petze lbauer, Department of Dermatology,
University o[V ienna, A-I090 Vienna, Austria.
Abbreviations: SVP, superficia l vascular plexus; UEA I, ulex ellropeus agglutinin I.
0022-202X!94!S07.00
Copyright © 1994 by The Society for Investigative D ermatology,Inc.
300
VOL. 103, NO.3
SEPTEMBER 1994
cannot be induced on the intrapapillary parts of the capillary loops
[1 ?fhe architecture of the SVP is altered in psoriasis. Specifically,
the capillary loops of lesional skin are tortuous and elongated [16]
and the normally well-defined boundary between capillary endothelial cells resting on an arteriolar-like homogeneous basement
membrane and endothelial cells on a venular-like laminated basement membrane are aberrant [17]. Microvascular endothelial cells
in lesional psoriatic skin express both ELAM-1 and VCAM-1 molecules [10,18], but the anatomic distributions and cytokine responsiveness of altered psoriatic microvessels have not previously been
described. In addition, the evaluation of perilesional microvessels
presents the opportu~ity ~o sepa~at~ the contributio~s of primary
microvascular alteratlOllS 111 psonasls from those of 1I1flammation
observed in lesional vessels.
C YTOKlNE RESPONSIVENESS OF PSORIATIC ENDOTHELIUM
60
ELAM · ' uninvolve d skin
60
VC AM· , uninvol ve d skin
T cells I HPF
--<>--
60 ELAM · ' pe rilesional skin
60 VC AM · ' perilesional skin
T col!s / HPF
---
--<>--
skin Specimens Trunk skin of eight different psoriatic patients, ranging
--0--
in age from 40 to 60 years, was obtained according to a protocol approved by
the Yale Human Investigations Committee. Superficial 3-mm punch biopsies were taken from lesional skin (n = 7; six with plaque-type and one with
guttate psoriasis), from normal~appearing skin at a 5- to 10-mm distance
from the leSion (penleslOnal skill, n = 8), and from chlllcally umnvolved
skin at sites at least 50 mm away from the nearest lesion (uninvolved skin,
Skin Organ Culture Each punch biopsy was bisected perpendicular to
the epidermis. One part was immediately embedded in OCT (Miles, Naperville, IL), snap frozen, and stored at -70 ' C. The other half was placed in
skin organ cultures as described previously [15]. In brief, skin specimens
were placed in C24-well plates (Falcon, Bedford, MA) with the epidermis
facing up, and attached to the plastic by air drying. RPMI 1640 culture
medium (Gibco, Grand Island, NY) supplemented with 10% human AB
serum (vol/vol; Gibco), L-glutamine (10 mM; Gibco), penicillin (100 U/
rnl; Gibco), streptomycin (100 ,ug/ml; Gibco), recombinant TNF, 200 U/
mI, obtained from Biogen (Cambridge, MA), and recombinant IL-4, 2000
V/ml, obtained from Schering Plough Research (Bloomfield, NJ) was gently added to each well so that just the epidermis remained uncovered. This
combination and dosage of cytokines was identified previously as that producing maximal changes in VCAM-l expression on dermal microvascular
endothelial cells (DMECs) in organ culture [15]. Explants were incubated at
37" C in humidified CO 2 /95% air for 24 h. At the end of the incubation
period, explants were embedded in OCT and snap frozen.
Monoclonal Antibodies (MoAbs) and Lectins The following mouse
MoAbs wereIgG1 isotypes: anti - ELAM-1 (H4/18), anti- VCAM- 1 (E1/6;
gift of M .P. Bevilacqua, Universiry of California at San Diego, San Diego,
CAl, anti-CD36 {OKM-5; Ortho, Raritan, NJ, and non-binding control
(K16/16; gift of D.L. Mendrick, Brigham and Women's Hospital, Boston,
MA) . Mouse anti-human CD3, COla, and CD68 MoAbs were IgG2a isotypes and obtained from Dakopatts (Carpinteria, CAl. Ulex europells agglutinin I {UEA I)-biotin was purchased from Vector Labs (Burlingame, CAl.
Inununohistochemistry Four-micrometer sections were processed and
double-stained as described [15]. In brief, the first MoAb {H4/18, El/6, or
OKM-5} was visualized using the alkaline phosphatase anti-alkaline phosphatase (APAAP) technique and stained in blue by the alkaline phospatase
substrate kit obtained from Vector. The biotinylatcd lectin UEA I was visualized using peroxidase-labeled avidin-biotin complexes and stained in red
by 3-amino-9-ethylcarbazole (Sigma Chemical Co., St. Louis, MO). Controls were performed by using a non-binding control MoAb (K16/16) as a
first-step reagent and/or by omitting the lectin. For CDla, CD3, or CD68
antigens, single antibody staining was performed using the peroxidase VectaStain ABC kit (Vector).
Scoring and Statistical Analysis CD36, ELAM-l and VCAM-l expression on endothelial cells were quantified on sections double stained with
UEA I as described [15] . The total number of vascular profiles (as identified
by UEA I staining) within the superficial vascular plexus (SVP) was determined in four randomly selected high-power fields in two different sections/skin specimens and then the number of CD36-, ELAM-1 - , and
VCAM-l-positive vessels were determined in the same fields. Vessels of the
deep vascular plexus were excluded because the deeper portions of the
dermis were usually not present in the biopsy specimens. Vessel cross-sections were considered to be positively stained when at least one cell in the
cross-section was clearly reactive with the specific MoAb. Staining intensity
was not considered. Data are expressed as the percentage of the total vessels
7
8
5
7
MATERIALS AND METHODS
n =4).
301
60
ELAM· ' lesionai skin
60
6
8
6
9
4
9
57
16
VCAM· ' lesio nal skin
T cells I H PF
---0---
----
ptO-
cu ltured
s k in
pre cu l1 ured
sk in
CYloktnoInduced
phenotype
46
200
120
--0--
-
26
26
-------
"0
45
c yloki noInduced
phenolype
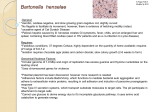
Figure 1. Percentage of ELAM-l+ or VCAM-l+ SVP vessel crosssections in uninvolved, perilesional, and lesional psoriatic skin. Each
liue connects preculture valu.es (left). with the percentage of positive vessels
after 24 h of organ culture 111 medium supplemented with TNF and IL-4
(right) of an individual skin specimen evaluated as described in Materials OIl d
Methods. The numbers to the right of the figure indicate the densities of
CI?3+ cells within the papillary dermis for uninvolved , perivascular, or
leslOual skill pnor to culture. Although VCAM-l expression is significantly
II1duclble III organ-cultured penleslOnal skin, the density of dermal T cells in
perilesional skin is comparable to th at seen in uninvolved skin.
(UEA 1+) in the SVP showing C D36 , ELAM-I, or VCAM-l expression .
Num~ers of T+ cells were quantified in the preculture skin specimen by
countlllg CD3 cells I~ four lugh-power fields (HPF; 0.5 mm in diameter)
wlthlll the upper dernus Il1 two different sections and the mean densiry / HPF
was detenlll~l~d. All specllnens were scored by a single observer (PP) blinded
to th e conditIOns .. The interobserver correlation coefficient (R2) has been
preVIOusly determllled as being 0.95 [15]. Data were pooled for each rype of
specimen {lesional, perilesional , or normal skin} and for each MoAb, and are
presented as mean ± SEM. Statistics were performed using the Student t test.
Immunoelectron Microscopy The organ-culture specimens were hand
cut into approximately 100-lim sections and fixed by immersion in 30/0
paraformaldehyde in 0.1 M phosphate buffer, pH 7.4, for 2 h at 4' C ,
followed by rinsing in phosphate buffer for 1 h. Immunohistochemistry was
performed using the peroxidase Vectastain ABC kit (Vector) . The sections
were incubated with the prima.ry MoAbs (H4/ 18 and E1 / 6) overnight at
4 ' C and the reaction products were visualized with diaminobezidine
(Sigma). Sections were post-fixed with half-strength Karnovsky 's fixative
and .wlth 1% OS04 and then embedded in Spurr's epoxy res in [19). Ultrathin
sectIOns were prepared for viewin g usin g a Zeiss electron microscope model
EM-l09.
RESULTS
Uninvolved Skin The mean density of CD3+ cells/HPF in uninvolved skin from psoriatic patients was 6.7 ± 0.6 (Fig 1), which
302
PETZELBAUER ET AL
is comparable to previously published CD3 counts in normal skin
[20]. In the preculture specimens, endothelial cells did not express
ELAM-l (0.5% ± 0.5% of vessels) or VCAM-l (0.7% ± 0.7% of
vessels) molecules, consistent with previous reports [15,21]. The
percentage of CD36+ vessel cross-sections within the SVP ranged
from 15% to 25%, which is identical to that seen in normal nonpsoriatic skin specimens [15]. CD36 molecule expression was unaltered by the cytokine treatment used and no differences were observed among uninvolved, periesional, or lesional skin specimens
and will not be discussed further.
When uninvolved skin was placed in organ-culture medium supplemented with TNF and IL-4 for 24 h, ELAM-l expression on
endothelial cells was significantly upregulated (27% ± 1.7% of
vessels; p < 0.001 compared to precultured skin; Fig 1) and was
restricted to venular endothelial cells. This extent of ELAM-l upregulation is comparable to that seen in normal, non-psoriatic skin
[15]. The capillary loops within the tips of the papillae above the
lower level of the rete ridges remained ELAM-l negative, as previously noted in normal skin [15] . VCAM-l expression on endothelial cells was undetectable after 24 h of organ culture (1.5% ± 1.0%
of vessels; Figs 1,2a), also consistent with previous findings in
endothelial cells of the SVP in normal skin.
Perilesional Skin At the light microscope level, perilesional skin
was generally indistinguishable from uninvolved skin in terms of
vascularization and density of dermal leukocytes. The rete were not
elongated in any of the eight specimens, although the epidermis in
two of eight specimens was slightly acanthotic. The mean density of
CD3+ cells/HPF was 14.3 ± 6.2, difference not significant compared to uninvolved skin (Fig 1). The num.bers of CD1a+ dendritic
cells and CD68+ macrophages were also comparable to those seen in
uninvolved skin (data not shown). Only 5.5% ± 2.3% of vessels
contained ELAM-l + endothelial cells, difference not significant
compared to uninvolved skin. VCAM-l expression on endothelial
cells was virtually undetectable (0.7% ± 0.4% of vessel cross sections ·contained VCAM-l + endothelial cells).
After 24 h of organ culture in medium supplemented with TNF
and IL-4, ELAM-1 + endothelial cells were significantly increased to
41.8% ± 4.2% of vessel cross-sections (p < 0.001 compared to precultured perilesional skin; Fig 1), which is similar to the findings in
uninvolved skin. In striking contrast to uninvolved skin, VCAM-1
expression was induced on endothelial cells in cytokine-treated perilesional skin to a level of 23.7% ± 7.1 % of vessel cross-sections;
p < 0.05 compared to precultured skin (Fig 1). The expression of
both ELAM-l and VCAM-l (Fig 2b) was restricted to the horizontal venules and the venular limb of the capillary loops below the
level of the rete. No ELAM-1+ or VCAM-1+ endothelial cells were
noted in the capillary loops above the level of the rete. By immunoelectron microscopy, staining for VCAM-1 molecules was found
on the luminal side of the venular endothelial cells and on the
interendothelial junctions. VCAM-l + endothelial cells could be
detected next to VCAM-1 - endothelial cells within the same microvessel.
Lesional Skin Morphologically, lesional specimens showed epidermal hyperproliferation, elongation of the rete ridges, tortuous
elongation of the capillary loops, and a moderate perivascular round
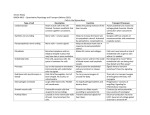
Figure 2. Uninvolved (a), perilesional (b), and lesional (c) psoriatic
skin after 24 h of organ culture in medium supplemented with TNF
and IL-4, stained immunohistochemically with anti- VCAM-l
MoAb in blue and the panendothelial marker UEA I in red. In uninvolved skin (a), VCAM-l cannot be induced on SVP endothelial cells; in
pcrilesional skin (b), VCAM-l expression is found on the horizontal venules
of the SVP (arrows). Capillary loops extending upward to the papillae are
VCAM-l - (arrowhead). In lesional skin (e), VCAM-l expression is found on
capillaries and small venulcs of the SVP (arrows), but also extends upward
into the intrapapillary portion of the capillary loop (arrowhead). Bar,
SO lim.
THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
VOL. 1.03, NO.3
SEPTEMBER 1994
C YTOKlNE RESPONSIVENESS OF PSORIATIC ENDOTHELIUM
303
DISCUSSION
Figure 3. The proximal part of a dermal capillary loop in lesional
psoriatic skin after 24 h of organ culture in medium supplemented
with TNF and IL-4 shown in a i-ttm plastic section. The epidermis (E)
is separated from the dermal papilla (P); arterial limb (A); venous limb (V).
cell infiltrate. The mean density of dermal CD3+ cells/HPF was
81.8 ± 24.4, which is significantly higher than in perilesional or
uninvolved skin (p < 0.05; Fig 1). The percentage of vascular pro@es containing ELAM-1+ endothelial cells was 29.4% ± 6% and
8.7% ± 3.2% contained VCAM-1+ endothelial cells (Fig 1). The
expression of both molecules was detectable on endothelial cells in
the venules of the SVP and in the capillary loops below the lower
level of the rete ridges. Of note, these molecules were also expressed
on capillary endothelial cells within the tips of the papillae in that
part of the loop that is in close anatomical proximity to the basal
keratinocytes.
In lesional skin, treatment with cytokines in organ culture increased ELAM-1 + endothelial cells to 45.7% ± 3.1 % of vessels;
p < 0.05 (Fig 1). VCAM-1+ endothelial cells were further increased to 41.4% ± 4.6% of vascular profiles; p < 0.005 compared
to precultured skin (Fig 1), Again, as seen in fresh lesional skin,
inducible ELAM-1 and VCAM-1 (Fig 2c) expression was detectable on capillary loops below and above the lower level of the rete
ridges. Furthermore, the staining intensity appeared enhanced in
organ-cultured skin compared to preculture specimens. Immunoelectron microscopy confirmed the light microscopic observations.
Within the horizontal part of the SVP ELAM-1+ and VCAM-1
endothelial cells (Fig 2) were found to be present within venules
but not arterioles. Immunoelectron microscopic evaluation was also
used to localize ELAM-1 and VCAM-1 within the capillary loops.
This is best illustrated by comparing Figs 3 and 4. Figure 3 is a 1-l1m
plastic section of organ-cultured lesional skin showing a capillary
loop. As seen in Fig 4, only the endothelial cells of the venular side
of the loop characterized by a laminated basement membrane express ELAM- l molecules.
We have examined the ELAM-1 and VCAM-1 expression patterns
in uninvolved, perivascular, and lesional psoriatic skin before and
after 24 h of organ culture in medium supplemented with TNF and
IL-4. We found that in preculture uninvolved and in perilesional
skin ELAM-1 and VCAM-l molecules are virtually absent on SVP
endothelium, whereas these molecules are expressed on endothelial
cells in lesional skin. After 24 h of cytokine treatment in organ
culture. ELAM-l is inducible on venules in uninvolved, perilesional, and in lesional skin. In contrast, VCAM-1 is not inducible in
uninvolved skin of psoriatic patients, consistent with our previous
report on organ-cultured normal skin of non-psoriatics [15]. Unexpectedly, cytokine stimulation of perilesional skin causes a significant upregulation of VCAM-1 expression on venular endothelial
cells of the SVP, compared to the preculture specimen, which is
comparable to the cytokine-induced upregulation ofVCAM-1 expression in organ-cultured lesional skin. Arteriolar endothelial cells
are consistently ELAM-1 and VCAM-1 negative in all specimens.
However, in psoriatic lesional skin, the intrapapillary portion of the
capillary loop acquires cytokine responsiveness and is able to express
ELAM- 1 or VCAM-1 molecules. These altered cytokille responses
parallel the elongation of the venular side of the loop characterized
by a laminated basement membrane.
The phenotypic change ofSVP endothelial cells consisting in the
ability to express VCAM-1 in perilesional psoriatic skin may be
relevant to the pathogenesis of psoriasis. VCAM-1 expression has
been observed in SVP endothelial cells ill lIillo only in settings of
natural or cytokine-induced inflammation [9,18,22,23J, and our
previous organ culture experiments of inflamed skin suggested that
the infiltrating leukocytes were necessary for endothelial cells to
display this capacity [15]. This led us to propose that infiltrating
leukocytes provide an as-yet unidentified co-factor that relieved
some inhibitory constraint. The present study suggests that SVP
endothelial cells can be relieved of this inhibition in the absence of
infiltrating leukocytes. The basis of this change is unknown but is
consistent with previous observations that the function of the microvasculature in perilesional psoriatic skin is altered. For example,
there is increased blood flow in perilesional psoriatic skin in the
absence of any microscopically detectable changes [24]. This alteration in the behavior of endothelial cells only at the advancing edge
of a psoriatic plaque may contribute to the sharply circumscribed
character of psoriatic lesions.
The other finding in this paper relevant for the pathogenesis of
psoriasis involves the phenotypic alteration of the endothelial cells
in the capillary loop in lesional skin of psoriasis that is not found in
acute dermatitis [15]. The expression ofELAM-1 and VCAM-1 in
this part of the capillary loop that is in proximity to the epidermis
probably contributes to the typical histopathologic appearance of
psoriatic lesions with epidermotropic neutrophils and T cells.
ELAM-1 is important for neutrophil recruitment [1,2]' and thus
expression of ELAM-1 at that site could initiate neutrophil traffic
into the epidermis that results in the characteristic picture of
"mounds of neutrophils on top of parakeratosis," which are typically localized above a tip of a papilla [25]. Epidermotropic T cells
that express the ELAM-1 ligand detected with MoAb HECA 452
(sometimes called cutaneous lymphocyte-associated antigen-1)
could also adhere in this part of the capillary loop [26,27]. Endothelial cell VCAM-1 interactions with T-cell VLA-4 may aJso contribute to epidermotropism of these cells [2]. These speculations are
supported by adhesion assays that demonstrate the enhanced binding of leukocytes, especially CD4+ lymphocytes, to psoriatic SVP
endothelium within the intra papillary part of the capillary loop
[28-30].
In conclusion, we have presented evidence that the cytokine responsiveness of microvascular endothelial cells is a.ltered in psoriasis
in a pattern that may explain both the circumscribed nature and the
epidermal involvement of the psoriatic plaque. These findings also
suggest the more general proposition that analysis of the contribution of endothelial cell adhesion molecules to inflammatory disease
must not only take into account the presence of inflammatory cyto-
304
THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
PETZELBAUER ET AL
Figure 4. Immunoelectron microscopy ofELAM-l from the section shown in Fig 3. Arterial limb with a homogenous basement membrane
(A); venous limb with a laminated basement membrane (V); de granulated mast cells (M). Bar, 111m. Lift upper itlSct, higher magnification of the
arterial limb indicated by the box. The endothelial cell (E) surface is nega tive for the peroxidase reaction product. Bar, 111m. Right upper inset, higher
magnification of the venous limb indicated by the box and shows the endothelial cell (E) surface positive for the peroxidase reaction product. Bar, 111 m .
kines that induce these molecules but the variable ability of specific
endothelial cells to respond.
4.
5.
This work was supported by NIH grant HL36003 (to ]SP) , by aJellowship Jrom the
Max Kade FOlmdation, NY (to PP), atld by the Yale Skin Disease Research Center
grant AR41942. Th e Molecular Cardiobiology Program at the Boyer Cetlter Jor
Molecular Medicitle is supported by Americatl Cyanamid. We wish to thank Biogen
and Scllering-Plough Research Corporation Jor providing cytokines and Drs. Michael Bellilacqua. Dotma Mendrick, and Timothy SpringerJor providit'g antibodies.
REFERENCES
Bochner BS, Luscinskas FW, Gimbrone Jr MA, Newman W, Sterbinsky SA,
Derse-Anthony CP, Klunk D, Schleimer RP: Adhesion of human basophils,
eosinophils, and neutrophils to interleukin I-activated human vascular endothelial cells: contributions of endothelial cell adhesion molecules. ] Exp Med
173:1553 - 1557,1991
2. Shimizu Y, Newman W, Gopal TV, Horgan KJ, Graber N, Beall LD, van
Seventer GA, Shaw S: Four molecular pathways ofT cell adhesion to endothelial cel ls: roles of LFA-l, VCAM-l, and ELAM-l and changes in pathway
hierarchy under different activation conditions.] Cell Bioi 113:1203-1212,
1991
3. Oppenheimer-Marks N, Davis LS, Tompkins-Bogue D, Ramberg), Lipsky PE:
Differential utilization of rCAM-l and VCAM-l du.ring the adhesion and
transendothelial migration of human T lymphocytes. ] [",,,,""01147:2913 292 1,1991
6.
7.
8.
1.
9.
10.
Weller PF, Rand TH, Goelz SE, Chi-Rosso G, Lobb RR: Human eosinophil
. adherence to vascular endothelium mediated by binding to vascular cell adhesion molecule 1 and endothclialleukocyte adhesion molecule 1. Proc Nad Arad
Sci USA 88:7430- 7433, 1991
Munro jM, Pober jS, Cotran RS: Recruitment of neutrophils in the local endotoxin response: association with de novo endothelial expression of endothelial
leukocyte adhesion molecule-1. Lab Illvest 64:295-299, 1991
Munro ]M, Pober JS, Cotran RS: Tumor necrosis f.1ctor and interferon-), induce
distinct patterns of endothelial activation and associated leukocyte accumulation in skin of Papio Anubis. Alii] PatllO/135:121-133, 1989
Smith CW,Roth lein R, Hughes BJ, Mariscalco MM, Rudloff HE, Schmalstieg
FC, Anderson DC: Recognition of an endothelial determinant for CDI8-dependent human neutrophil adherence and transendothelial migration. J C/i"
[rlVest 82:1746-1756,1988
Groves RW, Ross E, Barker JNWN , Ross jS, Camp RDR, MacDonald OM:
Effect of in vivo interleukin-l on adhesion molecule expression in nonnal
human skin. ] Illvest Derlllato/98:384 -387, 1992
Briscoe DM, Cotran RS, Pober jS: Effects of tumor necrosis factor, lipopolysaccharide, and IL-4 on the expression of vascular cell adhesion molecule-l in
vivo. Correlation with CD3+ T cell infiltration.] 1111111111101149: 2954-2960,
1992
Groves R W, Ross EL, Barker) N, MacDonald DM: Vascular cell adhesion molecule-l: expression in normal and diseased skin a_n d regulation in vivo interferon
11.
gamma.] Alii Acad Derlllato/ 29:67 - 72, 1993
Pober is, Bevilacqua MP, Mendrick DL, Lapierre LA, Fiers W , Gimbrone Jr MA:
Two distinct monokincs. intcrlcukin 1 and tumOr necrosis factor. each inde-
pendently induce biosynthesis and transient expression of the same antigen on
the surface of cultured human vascular cells.] Ittutllwo/136: 1680 - 1687 , 1986
12. Thornhill MH, Haskard DO: lL-4 regulates endothelial cell activation by IL-l ,
tumor necrosis factor, or IFN-gamma.] IlIIttIlIlIO/145:865-872, 1990
VOL. 103, NO.3
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
CYTOKINE RESPONSIVENESS OF PSORIATIC ENDOTHELIUM
SEPTEMBER 1994
305
Masinovski B, Urdal D , Gallatin WM: IL-4 acts synergisticall y with IL-1P to
promote lymphocyte ad hesion to microvascular endothelium by induction of
vascular cell adhesion molecule-I.] l",mIIll01145 :2886-2895, 1990
Pober JS , Gimbrone Jr MA, Lapierre LA , Mendrick DL, Fiers W , Rothlein R,
SpringerTA: Overlapping patterns of activation by human endothelial cells by
interleukin 1, tumor necrosis factor and immune interferon. ] Imrn'lII o/
137:1893 -1 896, 1986
Petzel bauer P, Bender JR, W ilson J, Pober JS: Heterogeneity of dermal microvascular endothelial ce ll antigen expression and cytokinc responsiveness in situ and
in cell culture.] [l/ImllllOl (in press)
Telner P, Fekete Z: The capillary responses in psoriatic skin.] Invest Dermato!
36:225 - 230, 1961
Braverman 1M, Sibley J : Role of the microcirculation in the treatment and pathogenesis of psoriasis. ] !tavest Dermato! 78:12- 17, 1982
Groves RW, Allen MH , Barker JNWN, H askard DO, MacDonald DM: Endothelial leukocyte adhesion molecule-I (ELAM-1) expression in cutaneous inflammation . Br] Dermato!1 24: 11 7 - 123, 1991
(VCAM-1) in experimenta l cutaneous inflammation: a comparison of ul traviolet B erythema and delayed hypersensitivity.] Invest Dermato! 96:763-770,
199 1
23. Griffiths CE, Barker IN, Kunkel S, NickoloffBJ: Modulation ofieukocyte ad hesion molecules, a T-cell chemotaxin (IL-8) and a regulatory cytokine (TNF-alpha) in allergic contact dermatitis (rhus dermatitis). Br] Dermato! 124:519526,1991
24. Hull SM, Goodfield M , Wood EJ, Cunliffe W]: Active and inactive edges of
psoriatic plaques: identification by tracing and investigation by laser-doppler
f1 0wmetry and immunocytochemical techniq ues. ] Invest D ermato! 92:782785, 1989
25. Pinkus H , Mchregan AM: The primary Ilistologic lesion of seborrheic dernutitis
and psoriasis. ] Invest Dermato!46:109 - lt6, 1966
26. Picker LJ, Kishimoto TK, Smith CW, Warnock RA, Butcher EC: ELAM- l is an
adhesion molecule for skin-homing T cells. Naill" 349:796-799,1991
27. Picker LJ, Treer JR, Ferguson-Darnell B, Collins PA, Bergstresser PR, Terstappen L WMM: Control of lymphocyte recirculation in man. II. Differential
Y e n A, Braverman 1M: Ultrastruc ture of the human derl11::t1 m icrocirculation: th e
regulation of the cu taneous lymphocyte-associated antigen, a tissue-selec ti ve
horizontal plexus of the dermis.] Invest Dermato!66:131 - 142, 1976
Petzelbauer P, W olff K: Effects of cyclosporin A on resident and passenger immune cells of normal human skin and UV-induced erythema reactions. Br]
Dermato!1 27:560 - 565 , 1992
Cotran RS, Gimbrone Jr MA, Bevilacqua MP, Mendrick DL, Pober JS: Induction
and detection of human endothelial activation antigen in vivo.] Exp Med
164:661 -666 , 1986
Norris P, Poston RN , Thomas DS , Thornhill M , H awk J, Haskard DO: The
expression of endothelial leukocyte adhesion molecule-I (ELAM-1), intercellular adhesion molecule-I (ICAM- I), and vascular cell adhesion molecule-l
28.
29.
30.
homing receptor for skin homing T cells.] Illlmu Il0!150:1122-1136, 1993
C hin YH , Fa langa V, Taylor JR, CaiJP, Bax J : Adherence of human heIper/ memory T-cell subsets to psoriatic dermal endothelium.] [ liVest Derlll aloI 94:413 417,1990
Barker IN, Groves R W, Allen MH , MacDonald DM: Preferential ad herence ofT
lymphocytes and neutrophils to psoriatic epidermis. Br] Derm ato!127:2052 11 , 1992
Sackstein R, Falanga V, StrcileinJW, C hin YH: Lymphocyte ad hesion to psoriatic dermal endothelium is mediated by a tissue-specific receptor/ ligand interaction.] /tlllest Dermato! 91 :423 - 428 , 1988
ANNOUNCEMENT
"The Board of the Austrian Society of Dermatology and Venereology (hoc tempore president,
Klaus Wolff, M.D.) has awarded the Ferdinand von Hebra Medal in gold to Professor John
Thorne Crissey, University of Southern California, Los Angeles for achievements in the history of medicine (dermatology} ." (Upon application by Karl Holubar, M .D., past president and
historian) .