* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Sistem Keta - IGP355 – PATOFISIOLOGI PENYAKIT II
Complement system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Adaptive immune system wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Innate immune system wikipedia , lookup
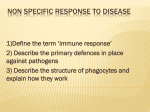
Sistem Ketahanan Tubuh dan Alergi Patofisiologi Gizi Pokok Bahasan pengertian sistem ketahanan tubuh, mekanisme seluler dan humoral mekanisme alergi dan hipersensitivitas alergi makanan Immune System Nonspecific Defenses Specific Defenses •Physical barriers •Phagocytes •Immunological surveillance •Interferons •Complement •Inflammatory response •Fever Limfosit B IgG IgA IgM IgD IgE Limfosit T Th (Th1&Th2) Ts Tdh Tc Physical Barriers Epidermal epithelium multiple layers of dead, keratinized cells and a network of desmosomes locking the cells together prevent pathogen entry. secretions such as sweat (the low pH of which is bacteriostatic) and sebum (which is bactericidal). linked by tight junctions and supported by a dense fibrous basement membrane. Tract mucus plays a big role in trapping infiltrating pathogens. Physical Barriers The epithelia lining the digestive, respiratory, reproductive, and urinary tracts Respiratory cilia help move the respiratory tract mucus upwards away from the delicate lung tissue. The stomach contains a very low pH and proteases that can destroy pathogens. Urine flushes the urinary tract while glandular secretions flush the reproductive tract. Many secretions contain chemicals and certain enzymes (such as lysozyme) which damage or kill bacteria. Here, we have pathogens traveling down the pharynx trying to attack the surface cells. How can they be repelled??? The mucosal cells lining the trachea have released a flood of mucus, trapping the pathogens! Now what??? The cilia successfully sweep the pathogens up and away! Phagocytes Phagocytes remove cell debris and respond to foreign invasion. They are the first line of cellular defense. Phagocytes include neutrophils, eosinophils, and macrophages. Phagocytes remove foreign invaders primarily via phagocytosis. The cell can phagocytose and kill bacteria for minutes to hours before expiring. Dead phagocytes (primarily neutrophils) are a major constituent of pus. Phagocytes Immunological Surveillance Refers to the constant monitoring of body cells by Natural Killer Cells recognizing and destroying any abnormal body cells, e.g., tumor cells or cells infected by a virus. NK cells destroy abnormal cells by releasing molecules called perforins adjacent to the abnormal cell. These perforins form a tube that punctures the abnormal cell membrane and causes it to lyse. INTERFERONS Small proteins released by macrophages, lymphocytes, and tissue cells infected with a virus. Note that interferon is not species-specific. Complement Plasma contains a set of proteins (made by the liver) known as the complement system. Inflammation A localized tissue response to injury that results in local sensations of pain, redness, swelling, and heat. Any stimulus that destroys cells (abrasion, chemical irritation, pathogen infection, extreme temperatures) will cause inflammation. The goals of inflammation are: Perform temporary repair and prevent additional pathogen entry. Slow the spread of pathogens away from the area. Mobilize local, regional, and systemic defenses that can overcome the pathogens and facilitate permanent repair. Steps of Inflammation Fever The hypothalamus contains a cluster of temperature-sensitive neurons that function in maintaining our stable body temperature. Bacterial toxins, antigen-antibody complexes, and interleukin-1 (a chemical released by active macrophages) all act as pyrogens. Pyrogens reset the body's thermostat and cause a rise in temperature. The rise in temperature causes an increase in the body's metabolic rate which allows the WBCs to function with greater efficiency. Also, fever induces the liver and spleen to sequester zinc and iron - 2 minerals necessary for bacterial metabolism. Specific Immunity Specific resistance is provided by the coordinated activities of T and B lymphocytes which respond to specific antigens. T cells are responsible for cellmediated immunity - our defense against abnormal cells and pathogens living within our cells. B cells are responsible for humoral immunity - our defense against antigens and pathogenic organisms in body fluids. Both mechanisms are quite important. Consider the fact that activated T cells do not respond to antigens in solution while antibodies produced by B cells cannot cross the cell membrane There are 3 major types of T cells: Cytotoxic T cells Helper T cells Suppressor T cells T Cells T cells recognize antigens when they are bound to special proteins in cell membranes. These membrane proteins are known as MHC proteins. Cell mediated Immunity T cells that contain the CD8/4 membrane protein interact with MHC proteins. The binding of another T cell membrane protein to a "costimulation protein”. Once costimulation has taken place, the T cell has been activated. Activated CD8 cells undergo a series of divisions that generate cytotoxic T cells and memory TC cells. Cell mediated Immunity Cytotoxic T cells (a.k.a. killer T cells) roam thru injured tissue and when one encounters its target antigens bound to an MHC protein of another cell, it will destroy it. This cell destruction is mediated by perforin release as well as several other chemical weapons Cell mediated Immunity CD4 cells undergo a series of divisions that produce Helper T cells and memory TH cells. The memory cells remain in reserve while the Helper T cells secrete a variety of chemicals (cytokines) that: •Stimulate the cell divisions that produce memory T cells and accelerate the maturation of Cytotoxic T cells. •Attract macrophages and stimulate their phagocytic activity. •Attract and stimulate the activity of NK cells. •Promote B cell division, plasma cell maturation, and antibody production. Cell B proliferation It should also be noted that there exist suppressor T cells that act to depress the actions of both T and B lymphocytes so as to moderate the immune response and help prevent any self-attack. Antibody shaped like the letter Y. The base : constant region, the arms : variable region. The constant region determines the class of the antibody The variable regions contain the antigen binding sites. There are 5 classes of antibodies (immunoglobulins or Igs) in body fluids: IgM, IgA, IgD, IgG, and IgE. Antibodies in each class will contain the same constant regions but different variable regions. IgM: Ig M First antibody type released during immunization. Elevated levels indicate recent infection or recent exposure to antigen. Extremely good at agglutination b/c it typically exists as a pentamer (5 monomers hooked together). Each pentamer could potentially bind 10 antigens. Anti-A and anti-B antibodies are examples. Activates complement. IgA: Major antibody released in external secretions such as saliva, mucus, sweat, gastric fluid, and tears. Typically exists as a dimer 2 monomers linked together. Is of primary importance against local infection in areas such as the respiratory and gastrointestinal tract. IgD: Expressed on the surface of B lymphocytes where it acts as an antigen receptor. IgG: The predominant antibody in blood, lymph, and CSF. Functions include: Complement activation. Toxin neutralization. It is the antibody of choice for passive immunization against toxins and venoms. Opsonization. Immobilization of bacteria. IgE: Its constant region binds with high affinity to basophils and mast cells. Thus, it can be involved in allergic reactions. Also plays a role in protection against parasitic worm infections. How antibody works Neutralization - binding to a toxin or virus can prevent it from attaching to a cell and causing damage. Agglutination & Precipitation - because each antibody can bind to at least 2 antigens, antigens bound by antibodies become linked or clumped together. If cells are being clumped, this is referred to as agglutination. If extracellular molecules are being clumped, it's referred to as precipitation. In both cases, the clumped immune complexes are much more likely to be phagocytosed. How antibody works Activation of Complement many antibodies contain binding sites that become exposed when the antibody binds an antigen. Opsonization - antibodies also act to physically connect antigens to phagocytes and thus increase the likelihood of phagocytosis. Stimulation of Inflammation - the binding of antigens to IgE's embedded in the plasma membranes of mast cells and basophils will cause histamine release. Autoimmune Disease Failure to discern self and non-self. Auotimmune diseases can result if lymphocytes are not properly "educated," those lymphocytes that can attack self-antigens are not removed in the thymus or bone marrow during development. They can also occur if new self-antigens appear later in the life. The immune system can unfortunately see these new antigens as foreign. Also, sometimes, bacterial or viral antigens may resemble proteins normally on the cell surface (e.g., MHC proteins). Thus the antibodies directed against the bacterial/viral antigen could then also attack the normal self-protein. Allergy There are 4 types of immune reactions: Type I, II, III and IV The most common food allergic reaction is type I Contribution of non type I reaction is not clear Egg, cow’s milk, peanut, soy, wheat, etc Type I hypersensitivity Immediate hypersensitivity Involving Ig E Combination of allergen + allergen-specific Ig E release of chemical mediators (histamines, cytokines, prostaglandins, interleukin, etc) Itching, contraction of smooth muscle, vasodilation, mucus secretion Symptoms of food allergies No System involved Symptoms 1 Gastrointestinal Abdominal pain, nausea, vomiting, diarrhea, GI bleeding, protein losing enteropathy, oropharyngeal pruritus 2 Cutaneus Urticaria, angioedema, eczema, erythema, itching, flushing 3 Respiratory Rhinitis, asthma, cough, laryngeal edema, Heiner’s syndrome, airway tightening 4 Systemic Anaphylaxis, hypotension, dysrhytmias 5 Unproven manifestation Behavioral disorders, tension-fatigue syndrome, otitis media, neuropsychiatric disorder, etc Food intolerance Adverse reactions to food caused by nonimmunologic or non Ig E mechanism Including toxic, pharmacologic, metabolic or idiosyncratic reactions Symptoms includes GI, cutaneus, and respiratory disorders Often similar with food allergy Food additives, sulfites, carbohydrates