* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Correlations among measles virus
Anti-nuclear antibody wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Molecular mimicry wikipedia , lookup
Immune system wikipedia , lookup
Globalization and disease wikipedia , lookup
Vaccination policy wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Innate immune system wikipedia , lookup
Adaptive immune system wikipedia , lookup
Social immunity wikipedia , lookup
Hepatitis B wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
DNA vaccination wikipedia , lookup
Herd immunity wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Immunocontraception wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
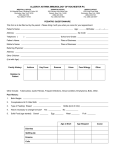
et al. Clinical and Experimental Immunology ORIGINAL ARTICLE doi:10.1111/j.1365-2249.2005.02931.x Correlations among measles virus-specific antibody, lymphoproliferation and Th1/Th2 cytokine responses following measles–mumps–rubella-II (MMR-II) vaccination N. Dhiman,* I. G. Ovsyannikova,* J. E. Ryan,* R. M. Jacobson,*† R. A. Vierkant,‡ V. S. Pankratz,‡ S. J. Jacobsen‡ and G. A. Poland*§ *Mayo Vaccine Research Group, †Department of Pediatric and Adolescent Medicine, ‡Department of Health Sciences, and §Program in Translational Immunovirology and Biodefense, Mayo Clinic College of Medicine, Rochester, MN, USA Accepted for publication 3 August 2005 Correspondence: Gregory A. Poland MD, Mayo Vaccine Research Group, Program in Translational Immunovirology and Biodefense, Mayo Clinic and Foundation, 611 C Guggenheim Building, 200 First Street, SW, Rochester, MN 55905, USA. E-mail: [email protected] Summary Immunity to measles is conferred by the interplay of humoral and cellular immune responses, the latter being critical in maintaining long-term recall response. Therefore, it is important to evaluate measles-specific humoral and cellular immunity in populations several years after vaccination and understand the correlations among these measures of immunity. We examined measles-specific antibodies, lymphoproliferation and the Th1/Th2 signature cytokines, interferon (IFN)-γγ and interleukin (IL)-4, in a population-based cohort of healthy children from Olmsted County, Minnesota after two doses of measles–mumps–rubella-II (MMR-II) vaccine. We detected positive measures of measles-specific cellular and humoral immunity in the majority of our study population. However, a small proportion of subjects demonstrated an immune response skewed towards the Th2 type, characterized by the presence of either IL-4 and/or measles-specific antibodies and a lack of IFN-γγ production. Further, we observed a significant positive correlation between lymphoproliferation and secretion of IFN-γγ (r = 0·20, P = 0·0002) and IL-4 (r = 0·15, P = 0·005). Measles antibody levels were correlated with lymphoproliferation (r = 0·12, P = 0·03), but lacked correlation to either cytokine type. In conclusion, we demonstrated the presence of both long-term cellular and humoral responses after MMR-II vaccination in a significant proportion of study subjects. Further, a positive correlation between lymphoproliferation and IL-4 and IFN-γγ suggests that immunity to measles may be maintained by both Th1 and Th2 cells. We speculate that the Th2 biased response observed in a subset of our subjects may be insufficient to provide long-term immunity against measles. Further examination of the determinants of Th1 versus Th2 skewing of the immune response and long-term follow-up is needed. Keywords: antibody, cellular immunity, cytokines, lymphoproliferation, measles Introduction Measles leads to nearly 1 million deaths each year, due primarily to failure to vaccinate and due in part to vaccine failure [1–6]. Antibody responses to measles infection or vaccination have been studied extensively and are used as correlates of protection against measles. Vaccine failure has been defined in terms of antibody response alone, and the markers of measles virus-specific cellular immunity after vaccination have been poorly characterized. Although the role and relative contribution of cellular immunity in imparting protection against measles in response to vaccina498 tion is unknown, CD4 T cell responses are known to influence indirectly the antibody responses [7–10]. Measles infection is known to cause an acute and profound state of immune suppression in few individuals, characterized by polarization of effector CD4 T cells to produce T helper type 2 (Th2) cytokines [7–9,11]. Similarly, measles vaccination can also cause immune suppression and predominant IL-4 production in some cases [10,12]. This skewing of the cytokine response towards predominant Th2-type cytokines results in a deficient or low Th1 cellular immune response and increases susceptibility to co-infections with various other pathogens [13,14]. The preferential expansion of the © 2005 British Society for Immunology, Clinical and Experimental Immunology, 142: 498–504 Humoral and cellular immunity to MMR-II CD4 T cell pool into Th2 cells is characterized by an increase in IgE, IgG1 and IgG4, diminished production of the Th1 signature cytokine interferon (IFN)-γ and heightened production of interleukin (IL)-4 (a cytokine critical for establishing the Th2 type response) [8,15]. Further, cellular immunity is known to play a critical role in controlling measles virus replication. Children with cellular immune deficiencies are known to develop severe complications associated with measles virus infection and recover poorly compared to their healthy counterparts [16,17]. Because cellular immunity plays a critical role in the maintenance of recall responses and control of measles virus infection, it is important to evaluate the presence of measles-specific cellular immunity in addition to antibody levels in populations several years after vaccination and understand the possible correlations among these measures of immunity. In the current study, we examined the correlation among measles virus-specific antibodies, lymphoproliferation and Th1/Th2 cytokine responses following two doses of measles– mumps–rubella-II (MMR-II) vaccine. The purpose of this study was to identify markers of immune response to each effector arm of immunity and to assess if correlations exist among these measures of immunity. Materials and methods Human subjects The details of our study sample recruitment have been described previously [18]. Briefly, we recruited a populationbased, stratified random sample of 346 healthy children and young adults (12–18 years of age) from all socio-economic strata residing in Rochester, Minnesota. Study subjects had documentation in their medical records of receiving two doses of the MMR-II vaccine containing the Edmonston strain of measles virus (tissue culture infective dose TCID50 ≥ 1000), the Jeryl Lynn B-strain of mump virus (≥ 20 000 TCID50) and the Wistar RA 27/3-strain of rubella virus (≥ 1000 TCID50) on or after the age of 12 months. There had been no circulating wild-type measles virus in this geographical area of residence during the subjects’ lifetimes. We determined the level of measles-specific antibodies, lymphoproliferation and cytokine production after ex vivo measles stimulation to characterize overall immunity to measles in our study population. We included 339 subjects in the final analysis for whom we had all four measures of immunity. The study was approved by the Mayo Clinic’s Review Board. We obtained written, informed consent or assent (from younger subjects) from subjects and/or parents/guardians from all the subjects at the time of enrolment in the study. Antibody assays Quantitative levels of measles-specific IgG antibody titres for all serum specimens were determined by the Enzygnost (Dade Behring, Marburg, Germany) anti-masern-virus/IgG enzyme immunoassay (sensitivity = 99·6%; specificity = 100%), as described previously [18]. Briefly, sera were separated from whole blood by centrifugation. Sera were aliquoted and stored at −80°C until the time of the assay. Serum samples were added in duplicate to a microtitre plate, which contained two parallel wells coated with a test whole measles virus antigen or control antigen derived from noninfected cells. Optical densities were determined at 450 nm and corrected at 650 nm on a microplate reader (Molecular Devices Corporation, Sunnyvale, CA, USA). The difference in mean absorbance between the viral test antigen and the control antigen for each sample was calculated and multiplied by a correction factor (determined by dividing a kitspecific nominal value by the mean of the reference standard) to give the corrected change in absorbance (∆A). Measles-specific IgG antibody levels (mIU/ml) were calculated from the antilog of the following formula: log10 = α*∆Aβ (where α and β are lot-dependent constants). Positive antibody response was defined as a change in absorbance (∆A) > 0·2. The coefficient of variation for this assay in our laboratory was 3·8%. Preparation of peripheral blood mononuclear cells (PBMC) PBMC were separated from heparinized venous blood by Ficoll-Hypaque (Sigma, St Louis, MO, USA) density gradient centrifugation and washed in RPMI-1640 medium (Celox Laboratories, Inc., St Paul, MN, USA) supplemented with 100 µg/ml streptomycin (Sigma), 100 U/ml penicillin (Sigma) and 8% heat-inactivated fetal calf serum (FCS) (Hyclone, Logan, UT, USA). Cells were then counted, resuspended in RPMI freezing media containing 10% dimethyl sulphoxide (Sigma), 20% FCS, frozen at −80°C overnight and stored in liquid nitrogen until cultured. Lymphoproliferation assay Lymphoproliferation to measles vaccine virus was assessed using an in vitro [3H]-thymidine incorporation assay as described previously [18]. Briefly, PBMC (2 × 105cells/well) were incubated for 72 h in RPMI-1640 medium, supplemented with 5% autologous sera, in the presence of live attenuated measles vaccine virus [75 plaque-forming units (pfu)/well]. Plain RPMI media served as the unstimulated control, and phytohaemagglutinin (PHA, 5 µg/ml) was used as a positive control for lymphoproliferation. The PBMC were then pulsed with [3H]-thymidine for 18 h, harvested on glass fibre filters and counted for the amount of incorporated radioactivity. Results were then expressed as stimulation indices (SI), which are defined as the ratio of the median counts per minute (cpm) of antigen-stimulated wells to the median cpm of unstimulated control wells. Stimulation indices of three or higher were considered to be © 2005 British Society for Immunology, Clinical and Experimental Immunology, 142: 498–504 499 N. Dhiman et al. an indicator of a positive lymphoproliferation response [19]. Measurement of IFN-γγ and IL-4 cytokines The details of the IFN-γ and IL-4 cytokine assays are described in detail elsewhere [20]. Briefly, for IFN-γ determination, thawed PBMC were cultured at a concentration of 2 × 105 in RPMI 1640 media containing 10% normal human serum (NHS), 100 U/ml penicillin and 100 µg/ml streptomycin with or without measles (MV) virus (Edmonston B vaccine strain of MV cultured in African green monkey kidney cells) at a multiplicity of infection (moi) of 0·5 for 6 days. For IL-4 determination, we cultured thawed PBMC at a concentration of 4 × 105 in RPMI-1640 media, supplemented with 10% NHS, 100 U/ml penicillin and 100 µg/ml streptomycin. Cells were cultured in the presence of 2 µg/ml of monoclonal IL-4 receptor antibody (R&D Systems, Minneapolis, MN, USA) with measles virus at a moi of 0·1 for 6 days as previously described [21,22]. These doses were chosen carefully to operate in approximately 70% measlesvirus stimulation dose for immune activation (and not too high or too low a dose) to avoid skewing the immune response to either direction due to overloading or underpresentation of the antigen. Stimulation with PHA, 5 µg/ml, was used as a positive control. Vero cell lysate was used as unstimulated control. Cell culture supernatants were collected and assayed for IFN-γ and IL-4 using a standard enzyme-linked immunosorbent assay (ELISA) protocol (OptiEIA Human IFN-γ and IL-4) (PharMingen, San Diego, CA, USA). The IFN-γ and IL-4 concentration of each test sample was calculated by reference to the standard curve. Median background levels of IFN-γ and IL-4 cytokine production in unstimulated wells were subtracted from the median measles-induced responses to produce ‘corrected’ secretion values. Any value above the unstimulated control was considered positive. Negative corrected values indicate that the unstimulated secretion levels were, on average, higher than the stimulated secretion levels. Statistical analysis Data were summarized descriptively using frequencies and percentages for all categorical variables and medians and interquartile ranges (IQR) for all continuous variables. Associations of immune response with demographic and clinical variables were assessed using analysis of variance methods. Due to data skewness, all P-values were calculated using rank-transformed values. An intraclass correlation coefficient (ICC) and corresponding 95% confidence interval was calculated to assess the magnitude of variance across the four different immune response measures relative to error variance [23]. Ranktransformed values were used to calculate the ICC due to data skewness in the immunity variables. Spearman’s 500 Table 1. Demographic variables of the study population. Variable n = 339 Age, years (median, IQR*) Gender (n, %) Female Male Race (n, %) Caucasians Others Age, months at first MMR-II immunization (median, IQR) Age, years at second MMR-II immunization (median, IQR) Time, years since last MMR-II immunization to blood draw (median, IQR) 15 (13,17) 159, 47% 180, 53% 316, 93% 23, 7% 15·6 (15·1, 17·5) 12·1 (11·5, 12·6) 4·8 (2·8, 6·1) *IQR, interquartile range; MMR-II, measles–mumps–rubella-II. correlation coefficients were then used to assess all pairwise associations between the immunity measures. All statistical tests were two-sided, and all analyses were carried out using SAS software system (SAS Institute, Inc., Cary, NC, USA). Results Demographic variables Our study population had a median age of 15 years at the time of recruitment with near equal gender representation (53% males). The majority of subjects were Caucasians (93%) and the median age at the first and second immunization was 15·6 months and 12·1 years, respectively. Measles virus-specific immune responses were measured after a median time period of 4·8 years after the last immunization (Table 1). Immunological variables The median value for measles-specific IgG was 1553 mIU/ ml, and the median SI for the lymphoproliferation was 3·8 (Table 2). We observed an increase in the antibody levels to measles with increasing age at the first MMR-II vaccination (P = 0·05). Similarly, an increase in age at the second MMRII vaccination showed an increasing trend in antibody levels to measles (P = 0·04) (data not shown). No association was found between the lymphoproliferative response and any of the demographic variables (data not shown). Median values for measles-specific IFN-γ and IL-4 cytokines were 40·7 pg/ ml and 9·7 pg/ml, respectively (Table 2). The IFN-γ and IL-4 responses to measles vaccination were found to be independent of gender, age or time lapsed since last immunization in our study cohort (data not shown). The proportion of individuals that had a positive response for measles specific antibody, lymphoproliferation, IFN-γ and IL-4 as per our cut-off criteria was 0·86, 0·58, 0·83 and 0·85, respectively (Table 2). Overall, 37·5% of our study © 2005 British Society for Immunology, Clinical and Experimental Immunology, 142: 498–504 Humoral and cellular immunity to MMR-II Table 2. Characterization of measles-specific cellular and humoral positive responses in study subjects. Variable (n = 339) IgG (mIU/ml) Stimulation index (SI) IFN-γ (pg/ml) IL-4 (pg/ml) Median (IQR) n, % Subjects with positive response* 1553 (737, 2637) 3·8 (1·9, 6·6) 40·7 (8·1, 176·7) 9·7 (2·8, 24·3) 290, 86% 195, 58% 281, 83% 288, 85% *Positive antibody response = change in absorbance (∆A) > 0·2. Measles-specific IgG antibody levels (mIU/ml) are calculated from the antilog of the following formula: log10 = α*∆Aβ (where α and β are lotdependent constants). *Positive stimulation index (SI) response ≥ 3. *Positive cytokine response is any value above background. Median background levels of interferon (IFN)-γ and interleukin (IL)-4 cytokine production in unstimulated wells were subtracted from the median measles-induced responses to produce ‘corrected’ secretion values. The uncorrected median (IQR) for IFN-γ (pg/ml) was 40·7 (3·7, 196·3) and −2·9 (−9·9, 6·85) for measles virus (MV) stimulated and unstimulated control, respectively. The uncorrected median (IQR) for IL-4 (pg/ml) was 15·5 (5·0, 30·8) and 3·46 (−1·42, 10·48) for MV stimulated and unstimulated control, respectively. subjects had a positive response for all four measures of immunity, 98·8% for at least one measure of immunity, while only 1·2% lacked positivity to any of the measured variables (Table 3). From the 98·8% of subjects that measured positive for at least one variable, 7·4% of the subjects demonstrated undetectable levels of IFN-γ production and negative measles-specific lymphoproliferation (Table 3). Correlation between immunological variables Table 4 shows the correlation among the pairs of measures of measles-specific antibody, lymphoproliferation, IFN-γ and IL-4 as represented by a Spearman’s correlation matrix. The antibody levels were correlated to lymphoproliferation (r = 0·12, P = 0·03), but lacked any correlation with the measures of IFN-γ and IL-4 secretion. Alternatively, we found a significant correlation between lymphoproliferation and IFN-γ (r = 0·20, P = 0·0002) as well as lymphoproliferation and IL-4 (r = 0·15, P = 0·005) secretion. Further, measles-specific IFN-γ had a significant positive correlation Table 3. Characterization of measles-specific humoral and cellular immunity in study subjects. Immune measure Variable positive Frequency* Percentage* % Cumulative Cellular and humoral IgG, SI, IFN-γ, IL-4 IgG, SI, IFN-γ IgG, SI, IL-4 IgG, IFN-γ, IL-4 SI, IFN-γ, IL-4 IgG, SI IFN-γ, IL-4 IgG, IFN-γ SI, IL-4 127 20 21 82 17 4 17 15 3 37·5 5·9 6·2 24·2 5·0 1·2 5·0 4·4 0·9 90·2 Th1-biased SI, IFN-γ SI IFN-γ 2 1 1 0·6 0·3 0·3 1·2 Th2-biased IgG, IL-4 IL-4 IgG 17 4 4 5·0 1·2 1·2 7·4 None – 4 1·2 1·2 *Frequency and percentage for individual immune measure are based on the cut-off criteria mentioned in the text. Table 4. Correlation between measles-specific antibody, lymphoproliferation, interferon (IFN)-γ and interleukin (IL)-4 responses in study subjects as represented by a Spearman’s correlation matrix. Variable IgG level (mIU/ml) Stimulation index (SI) IFN-γ (pg/ml) IL-4 (pg/ml) IgG level (mIU/ml) Stimulation index (SI) IFN-γ (pg/ml) IL-4 (pg/ml) 1·00 – – – 0·12 (0·03) 1·00 – – 0·03 (0·56) 0·20* (0·0002) 1·00 – 0·04 (0·45) 0·15* (0·005) 0·29* (< 0·0001) 1·00 The values in parentheses represent the corresponding P-values. *P-value ≤ 0·005 are shown in bold type. © 2005 British Society for Immunology, Clinical and Experimental Immunology, 142: 498–504 501 N. Dhiman et al. with measles-specific IL-4 secretion (r = 0·29, P < 0·0001) (Table 4). The overall value of the intraclass correlation for all four measures of immunity for measles was 0·14 (95% CI = 0·09–0·19). However, as these correlations are weak in magnitude (r < 0·3), they should be interpreted with caution. Discussion In the current study, we demonstrate the presence of longterm cellular and/or humoral immunity after vaccination with two doses of the currently recommended MMR-II vaccine in the majority of our study population by measuring measles-specific lymphoproliferation, antibodies and Th1/ Th2 signature cytokines, IFN-γ and IL-4. However, a small fraction of individuals (7·4%) demonstrated a Th2-biased immune response characterized by the presence of antibodies and IL-4 and undetectable IFN-γ and lymphoproliferative response. Although protective efficacy of measles vaccine is defined in terms of antibodies alone, several ‘experiments of nature’ demonstrate that cellular immunity is critical and sufficient to recover from measles infection. Children with agammaglobulinaemia have a normal course of clinical measles and recover uneventfully from measles infection, while those with defective cellular immunity (e.g. leukaemia, HIV) develop progressive illnesses and have high mortality from measles infection [14,24]. Previous studies demonstrate that measles infection can result in an acute and profound state of immune suppression and skew the immune response towards the Th2 phenotype, characterized by high production of IL-4 and increased immunoglobulin levels [7–11]. In addition, there is substantial evidence for a biased Th2 response after measles vaccine administration as documented by decreased responsiveness to mitogens [12] and predominant IL-4 production [10]. However, we have limited understanding of these measures of immunity to measles in populations several years after vaccination. In the current cohort, we demonstrate that a majority (90%) of the subjects had evidence for measles-specific immune markers for both the humoral and cellular effector arms years after measles vaccination. However, a small yet significant proportion (7·4%) of subjects did show a preferential bias towards the Th2 type response. Further, an even smaller fraction (1%) demonstrated no evidence of any of the four measures of immunity to measles. Although there is no critical requirement of vaccine-induced cellular response in imparting protection against infection, the individuals lacking cellular immunity may be at a disadvantage for virus clearance. No data are available on evaluation of the potential roles of Th1 and Th2 cells in measles viral clearance in humans. However, a recent study using the rhesus monkey model of measles infection demonstrates clearly that CD8 lymphocytes are major mediators of protection, and antibodies have a limited role in the control of measles replication and clearance [25]. The lack of correlation between measles-specific 502 antibodies and prolonged measles virus shedding in HIVinfected Zambian children also re-emphasizes the importance of cellular immunity in recovery from measles infection [26]. In contrast, antibodies alone can certainly mediate protection against measles virus infection as infants with immature cellular immunity can be protected by maternally acquired antibodies [27], or neutralizing antibodies from vaccination [28]. Similarly, a formalin-inactivated vaccine incapable of priming CD8 T cells is protective if antibody titres are high [29,30]. However, as antibodies wane over time, cellular immunity may be more important for maintaining long-term immunity and recovery from the disease. Similar discordance between the contribution of humoral immunity in viral clearance and protection has been established for other viruses, such as herpes simplex virus and hepatitis B virus [31,32]. The large sample size from our current study allowed us to determine correlations between measures of humoral and cellular immunity after vaccination, compared to solely looking at antibodies as markers for vaccine-induced immunity. We demonstrate a significant positive correlation between lymphoproliferation and two cytokines, IL-4 and IFN-γ, which play a crucial role in both the generation and regulation of immune responses. Further, the levels of IL-4 and IFN-γ were correlated positively in the study subjects. The results suggest that recall immunity to measles is maintained as a fine-tuned and tightly regulated immunological balance, where both IL-4 and IFN-γ play a key role. IFN-γ is critical for macrophage activation, T cell proliferation and differentiation and up-regulation of human leucocyte antigens [33–35]. IFN-γ exerts an antiviral effect by promoting the lysis and clearance of measles-infected cells and by inhibiting viral gene expression and replication [25,36,37]. In comparison, a Th2 response is characterized by IL-4 production and high levels of measles-specific antibodies after measles infection [8,10,38], which is used traditionally as the measure of protective immunity against subsequent infection. Because we found a positive correlation between lymphoproliferation and IL-4 and IFN-γ, our results suggest that measles immunity is maintained by both Th1/Th2 cells (or Th0-type T cells that are producers of both IL-4 and IFN-γ) [39]. Similar Th0 responses to wild-type measles virus-infected dendritic cells have also been observed [40]. However, measles vaccine-infected dendritic cells or subjects immunized with the measles vaccine predominantly produce a Th1 cytokine response [40,41]. This implies that to mount an immune response at various stages of viral invasion, the host cells maintain a functional pool of mixed Th1/Th2 cell populations. The Th1 response may help to clear intracellular viruses from infected host cells, and the Th2 response may help to clear extracellular viruses, which can be neutralized by antibodies and inflammatory cytokines. For example, a high intact rate of humoral and cellular immunity and the presence of both Th1/Th2 cytokines are observed in influenza vaccinated subjects, which suggests the © 2005 British Society for Immunology, Clinical and Experimental Immunology, 142: 498–504 Humoral and cellular immunity to MMR-II presence of Th0 cells [42]. In addition, we did not find any correlation between antibody levels to measles and measures of Th1/Th2 cytokines. This agrees with our previous findings demonstrating that correlations between measles-specific antibodies and IFN-γ and IL-4-secreting cell frequencies did not reach statistical significance [43]. Similar disagreement in quantitative correlation between antibody levels to measles and measures of T cell immunity can also be found in other studies [44–46]. Further work on the determinants of Th1 versus Th2 skewing of the immune response is needed. The major strength of our study is the stratified random sample of our population. The resulting sample well represents the US Caucasian population with high vaccination rates. An advantage of an ethnically homogeneous population is decreased confounding variables (ethnicity, previous viral exposure history, etc.), increasing the confidence in our findings. Further, the immunity measures were true responses to vaccination, as these subjects had not encountered wild measles virus in their lifetimes. We understand that an ideal control to evaluate the specificity of measles responses would be testing for immune measures to measles stimulation in naive cells. However, we are confident that the IFN-γ and IL-4 levels detected in our study are measlesspecific. For example, in our previous studies we were not able to detect any IL-4 and only very low levels of IFN-γ in naive cells after strong mitogen stimulation such as PHA [41]. However, we could detect significant IL-4 and IFN-γ secretion in response to ex vivo PHA stimulation in PBMC from these subjects after MMR-II vaccination [41]. This suggests that when we did observe IL-4 and IFN-γ secretion with measles stimulation in vaccinated individuals, it is represented as measles-specific response. A limitation of our study may be that we used different stimulation doses for IL-4 and IFN-γ secretion assays which may influence the differentiation to either Th1 or Th2 response. However, our selected doses had given us approximately 70% immune activation in our optimization studies, which is not too high or too low a dose to skew the immune response to either direction due to overloading or under-presentation of the antigen. Another limitation of our study is measurement of whole measles antibodies instead of neutralizing antibodies. Neutralizing antibodies would specifically measure protective antibody titres [28]. We were prompted to measure whole antibodies due to the correlation of neutralizing antibody titres with whole antibody enzyme immunoassays [47] and the ease of performing whole antibody immunoassays on a large sample size. Further, we measured Th1 and Th2 cytokines in a whole lymphocyte population instead of isolated CD4 and CD8 populations due to a limitation in cell numbers available. However, we believe that CD4 cells are the predominant producers of the Th1/Th2 mixed response to measles based on our previous studies characterizing cytokine secreting cell types after measles stimulation [22,39]. In conclusion, we demonstrate that the majority of our study population had detectable measures of measles- specific cellular and humoral immunity following a median of 4·8 years after receipt of the second dose of MMR-II vaccine. However, 1·2% lacked a positive response to any measures of measles vaccine induced immunity, and 7·4% demonstrated a Th2-biased immune response. Our study provides insights into the mechanisms of measles vaccineinduced immune responses. It may be concluded that, in most cases, the immune system mounts a balanced Th1/Th2 response to vaccination. However, in a small fraction of individuals, a bias towards either type may be induced. However, it is speculated that individuals with humoral immunity alone may be at a disadvantage for decreased viral clearance and long-term protection due to waning of antibodies over time. Additional doses of vaccines or improved vaccination strategies such as peptide-based vaccines may need to be developed to overcome the lack of cellular immunity in those individuals who do not respond to the current vaccine. This is critical for recall immunity and lifelong protection, where humoral immunity alone may be insufficient to recover from infection. Acknowledgements We thank the parents and children who participated in this study. We acknowledge the efforts of the research fellows, nurses and students from the Mayo Vaccine Research Group. We also thank Carla Tentis for editorial assistance. This work was partially supported by NIH grants AI 33144 and AI 48793 and Mayo General Clinical Research Center (GCRC) grant M01-RR00585. References 1 Clements CJ, Cutts FT. The epidemiology of measles: thirty years of vaccination. In: ter Muelen V, Billeter M, eds. Measles virus. Berlin/Heidelberg: Springer-Verlag, 1995, pp. 13–33. 2 Centers for Disease Control and Prevention. Measles outbreak among school-aged children − Juneau, Alaska, 1996. JAMA 1996; 276:1294–5. 3 Jacobson RM, Poland GA. The genetic basis for measles vaccine failure. Acta Paediatr Suppl 2004; 445:1–6. 4 Markowitz LE, Katz ML. Measles vaccine. In: Plotkin SA, Mortimer EA Jr, eds. Vaccines. Philadelphia, PA: W. B. Saunders Co., 1994, pp. 229–76. 5 Yip FY, Papania MJ, Redd SB. Measles outbreak epidemiology in the United States, 1993–2001. J Infect Dis 2004; 189 (Suppl. 1):S54–60. 6 Coughlan S, Connell J, Cohen B, Jin L, Hall WW. Suboptimal measles–mumps–rubella vaccination coverage facilitates an imported measles outbreak in ireland. Clin Infect Dis 2002; 35:84–6. 7 Griffin DE, Ward BJ, Esolen LM. Pathogenesis of measles virus infection: an hypothesis for altered immune responses. J Infect Dis 1994; 170:S24–31. 8 Griffin DE, Ward BJ. Differential CD4 T cell activation in measles. J Infect Dis 1993; 168:275–81. 9 Ward BJ, Johnson RT, Vaisberg A, Jauregui E, Griffin DE. Cytokine production in vitro and the lymphoproliferative defect of natural © 2005 British Society for Immunology, Clinical and Experimental Immunology, 142: 498–504 503 N. Dhiman et al. 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 504 measles virus infection. Clin Immunol Immunopathol 1991; 61:236–48. Ward BJ, Griffin DE. Changes in cytokine production after measles virus vaccination: predominant production of IL-4 suggests induction of a Th2 response. Clin Immunol Immunopathol 1993; 67:171–7. Griffin DE. Immune responses during measles virus infection. Curr Top Microbiol Immunol 1995; 191:117–34. Smedman L, Joki A, José da Silva AP, Troye-Blomberg M, Aronsson B, Perlmann P. Immunosuppression after measles vaccination. Acta Paediatr 1994; 83:164–8. Ito I, Ishida T, Hashimoto T, Arita M, Osawa M, Tsukayama C. Familial cases of severe measles pneumonia. Intern Med 2000; 39:670–4. Markowitz LE, Chandler FW, Roldan EO et al. Fatal measles pneumonia without rash in a child with AIDS. J Infect Dis 1988; 158:480–3. Paul WE, Seder RA. Lymphocyte responses and cytokines. Cell 1994; 76:241–51. Burnet FM. Measles as an index of immunological function. Lancet 1968; 2:610–3. Kaplan LJ, Daum RS, Smaron M, McCarthy CA. Severe measles in immunocompromised patients. JAMA 1992; 267:1237–41. Ovsyannikova IG, Jacobson RM, Vierkant RA, Jacobsen SJ, Pankratz VS, Poland GA. The contribution of HLA class I antigens in immune status following two doses of rubella vaccination. Hum Immunol 2004; 65:1506–15. Gans HA, Maldonado Y, Yasukawa LL et al. IL-12, IFNg, and T cell proliferation to measles in immunized infants. J Immunol 1999; 162:5569–75. Ovsyannikova IG, Jacobson RM, Vierkant RA, Jacobsen SJ, Pankratz VS, Poland GA. Human leukocyte antigen class II alleles and rubella-specific humoral and cell-mediated immunity following measles–mumps–rubella-II vaccination. J Infect Dis 2005; 191:515–9. Dhiman N, Ovsyannikova IG, Howe RC, Ryan JE, Jacobson RM, Poland GA. Interleukin-4 induced by measles virus and measlesderived peptides as measured by IL-4 receptor-blocking ELISA. J Immunol Meth 2004; 287:217–25. Howe RC, Dhiman N, Ovsyannikova IG, Poland GA. Induction of CD4 T cell proliferation and Th1-like cytokine responses in vitro to measles virus. Clin Exp Immunol 2005; 140:333–42. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979; 86:420–8. Mitus A, Holloway A, Evans AE, Enders JF. Attenuated measles vaccine in children with acute leukemia. Am J Dis Child 1962; 103:413–8. Permar SR, Klumpp SA, Mansfield KG et al. Limited contribution of humoral immunity to the clearance of measles viremia in rhesus monkeys. J Infect Dis 2004; 190:998–1005. Permar SR, Moss WJ, Ryon JJ et al. Prolonged measles virus shedding in human immunodeficiency virus-infected children, detected by reverse transcriptase-polymerase chain reaction. J Infect Dis 2001; 183:532–8. Gans HA, Arvin AM, Galinus J, Logan L, DeHovitz R, Maldonado Y. Deficiency of the humoral immune response to measles vaccine in infants immunized at age 6 months. JAMA 1998; 280:527–32. Chen RT, Markowitz LE, Albrecht P et al. Measles antibody: reevaluation of protective titers. J Infect Dis 1990; 162:1036–42. 29 Polack FP, Auwaerter PG, Lee S-H et al. Production of atypical measles in rhesus macaques: evidence for disease mediated by immune complex formation and eosinophils in the presence of fusion-inhibiting antibody. Nat Med 1999; 5:629–34. 30 Guinee VF, Henderson DA, Casey HL et al. Cooperative measles vaccine field trial. I. Clinical efficacy. Pediatrics 1966; 37:649–65. 31 Mascola JR. Herpes simplex virus vaccines − why don’t antibodies protect. JAMA 1999; 282:379–80. 32 Szmuness W, Stevens CE, Zang EA, Harley EJ, Kellner A. A controlled clinical trial of the efficacy of the hepatitis B vaccine (Heptavax B): a final report. Hepatology 1981; 1:377–85. 33 Gogate N, Bakhiet M, Kristensson K, Norrby E, Olsson T. Gamma interferon expression and major histocompatibility complex induction during measles and vesicular stomatitis virus infections of the brain. J Neuroimmunol 1991; 31:19–26. 34 Goodbourn S, Didcock L, Randall RE. Interferons: cell signalling, immune modulation, antiviral responses and virus countermeasures. J Gen Virol 2000; 81:2341–64. 35 Paludan SR. Interleukin-4 and interferon-gamma: the quintessence of a mutual antagonistic relationship. Scand J Immunol 1998; 48:459–68. 36 Finke D, Brinckmann UG, ter Meulen V, Liebert UG. Gamma interferon is a major mediator of antiviral defense in experimental measles virus-induced encephalitis. J Virol 1995; 69:5469–74. 37 Bolt G, Berg K, Blixenkrone-Moller M. Measles virus-induced modulation of host-cell gene expression. J Gen Virol 2002; 83:1157–65. 38 Norrby E, Gollmar Y. Appearance and persistence of antibodies against different virus components after regular measles infections. Infect Immun 1972; 6:240–7. 39 Howe RC, Ovsyannikova IG, Pinsky NA, Poland GA. Identification of Th0 cells responding to measles virus. Hum Immunol 2005; 66:104–15. 40 Klagge IM, Abt M, Fries B, Schneider-Schaulies S. Impact of measles virus dendritic-cell infection on Th-cell polarization in vitro. J Gen Virol 2004; 85:3239–47. 41 Ovsyannikova IG, Reid KC, Jacobson RM, Oberg AL, Klee GG, Poland GA. Cytokine production patterns and antibody response to measles vaccine. Vaccine 2003; 21:3946–53. 42 Bernstein ED, Gardner EM, Abrutyn E, Gross P, Murasko DM. Cytokine production after influenza vaccination in a healthy elderly population. Vaccine 1998; 16:1722–31. 43 Ovsyannikova IG, Dhiman N, Jacobson RM, Vierkant RA, Poland GA. Frequency of measles virus-specific CD4+ and CD8+ T cells in subjects seronegative or highly seropositive for measles vaccine. Clin Diagn Lab Immunol 2003; 10:411–6. 44 Ward BJ, Boulianne N, Ratnam S, Guiot M-C, Couillard M, De Serres G. Cellular immunity in measles vaccine failure: Demonstration of measles antigen-specific lymphoproliferative responses despite limited serum antibody production after revaccination. J Infect Dis 1995; 172:1591–5. 45 Gans H, DeHovitz R, Forghani B, Beeler J, Maldonado Y, Arvin AM. Measles and mumps vaccination as a model to investigate the developing immune system: passive and active immunity during the first year of life. Vaccine, 2003; 21:3398–405. 46 Naniche D, Garenne M, Rae C et al. Decrease in measles virusspecific CD4 T cell memory in vaccinated subjects. J Infect Dis 2004; 190:1387–95. 47 Ratnam S, Gadag V, West R et al. Comparison of commercial enzyme immunoassay kits with plaque reduction neutralization test for detection of measles virus antibody. J Clin Microbiol 1995; 33:811–15. © 2005 British Society for Immunology, Clinical and Experimental Immunology, 142: 498–504