* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Immune homeostasis in the respiratory tract and its impact on
Survey
Document related concepts
Lymphopoiesis wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
DNA vaccination wikipedia , lookup
Infection control wikipedia , lookup
Molecular mimicry wikipedia , lookup
Neonatal infection wikipedia , lookup
Hepatitis B wikipedia , lookup
Immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Transcript
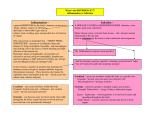
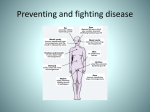
G Model YSMIM-695; No. of Pages 9 ARTICLE IN PRESS Seminars in Immunology xxx (2009) xxx–xxx Contents lists available at ScienceDirect Seminars in Immunology journal homepage: www.elsevier.com/locate/ysmim Review Immune homeostasis in the respiratory tract and its impact on heterologous infection Erika Wissinger, John Goulding, Tracy Hussell ∗ Imperial College London, National Heart and Lung Institute, Leukocyte Biology Section, Sir Alexander Fleming Building, Exhibition Road, London SW7 2AZ, United Kingdom a r t i c l e i n f o Keywords: Lung Innate immunity Homeostasis Secondary bacterial pneumonia Infection history a b s t r a c t Innate immunity at mucosal surfaces requires additional restraint to prevent inflammation to innocuous antigens or commensal microorganisms. The threshold above which airway macrophages become activated is raised by site-specific factors including the receptors for transforming growth factor beta, interleukin 10 and CD200; the ligands for which are produced by, or expressed on, respiratory epithelium. We discuss such site-specific regulation and how this is continually altered by prior infections. Resetting of innate reactivity represents a strategy for limiting excessive inflammation, but in some may pre-dispose to secondary bacterial pneumonia. © 2009 Elsevier Ltd. All rights reserved. 1. Introduction An immune response ensues when a pathogen or traumatic event is sufficiently dangerous that it exceeds a specific threshold of innate restraint. The restraint of innate (and ultimately adaptive) immunity occurs throughout the entire body, but the threshold of reactivity is adjusted in a site-specific manner [1,2]. Certain body compartments are bombarded with foreign material and must ignore the majority of it (the gut and lung), whereas others are essentially sterile and tend to respond immediately (the blood and spleen). Lung alveolar macrophages, for example, exist in an environment high in antigenic material, the majority of which must be ignored except when the antigen represents a serious threat [3,4]. Even the ignorance of antigen requires that the environment is sampled to ensure that particles present should indeed be ignored. For example, M cells [5,6] in the gut and parts of the lung sample the luminal contents for signs of a threat. Sub-mucosal immune cells are present and poised to react should they be required. Lung dendritic cells extend processes into the airway lumen to scan, interact with and, potentially draw antigens towards the waiting sub-mucosal immune population [7,8]. This site-specific immune response and the status of innate immunity in homeostasis however need to be adaptable. It would not make evolutionary sense for our threshold of reactivity (above which innate immunity activates) to be set before or immediately Abbreviations: TGF, transforming growth factor beta; CD200R, CD200 receptor; SP-A, surfactant protein A; LTA, lipoteichoic acid; LCMV, lymphocytic choriomeningitis virus. ∗ Corresponding author. Tel.: +44 2075943184. E-mail address: [email protected] (T. Hussell). after birth and remain in the same state throughout life. It would also possibly not make sense for innate immunity to return to the exact same state after resolution of a serious inflammatory event. Innate homeostasis may therefore be adaptable; altered by environmental influences, genetics, diet, stress, age and the sequence of prior inflammatory events. This adaptability will contribute to the diversity of responses to the same stimulus seen in any given population and probably helps to ensure that at least a proportion of those affected will survive. If thresholds of innate activation alter between body compartments and with each inflammatory event, what pathways are involved? What dictates whether a macrophage in a particular environment responds readily to antigen or essentially tolerates its presence? A tissue-specific switch must exist that is made up of a unique signature composed of immune regulatory versus immune potentiator pathways. This phenomenon of innate homeostasis and adaptability will be described for the lung microenvironment, in particular the airways. We will highlight similar processes in other sites where data is available and describe the consequences for subsequent immune reactions to respiratory pathogens. 2. The airways in homeostasis: innate immunity The healthy airways in man and mouse are dominated by alveolar macrophages (>95%). The remaining 5% are predominantly T cells expressing CD103+, ␥/␦ or ␣/ TCR and are generally CD4-/CD8- (or combinations of these phenotypes). Though alveolar macrophages express typical phenotypic markers (F4/80+, CD11chi , CD11bint ), functionally they behave differently to their tissue counterparts, even compared to those in the sub-mucosal tissues of the lung parenchyma. For example, alveolar macrophages are thought to be less efficient as antigen-presenting cells, with 1044-5323/$ – see front matter © 2009 Elsevier Ltd. All rights reserved. doi:10.1016/j.smim.2009.01.005 Please cite this article in press as: Wissinger E, et al. Immune homeostasis in the respiratory tract and its impact on heterologous infection. Semin Immunol (2009), doi:10.1016/j.smim.2009.01.005 G Model YSMIM-695; 2 No. of Pages 9 ARTICLE IN PRESS E. Wissinger et al. / Seminars in Immunology xxx (2009) xxx–xxx lower levels of MHC Class II and co-stimulatory molecules, than their tissue-resident counterparts [9]. In the steady-state they display a suppressive phenotype mediated by the secretion of IL-10, nitric oxide or TGF [10,11]. They are also poorly phagocytic compared to peritoneal macrophages [12] and actively inhibit T cell responses via secretion of prostaglandins and transforming growth factor beta (TGF) [13]. Alveolar macrophages produce a state of reversible T cell inactivation that is mediated either by defective expression of co-stimulatory molecules [14], or an increased expression of CD80 [15], a receptor that preferentially binds to the negative T cell receptor CTLA-4. The direct or indirect interaction of alveolar macrophages with other cells in the airways may also limit inflammatory responses in the steady-state. In addition to the suppression of T cell activation described above, alveolar macrophages also actively inhibit the antigen presentation function of interdigitating dendritic cells in the airways [16]. Reciprocally, the DCs exposed to antigen in the airway lumen produce IL-10, a broadly inhibitory cytokine which further limits the local inflammatory response [17]. Macrophages in the airways are functionally different to phenotypically identical counterparts elsewhere by several other suppressive pathways that in combination limit their responsiveness to external stimuli. Surfactant proteins and lipids are abundant in the alveolar spaces where they function to decrease surface tension at the air–fluid interface, allowing the airspaces to remain open [18]. Surfactant protein A (SP-A) has recently been shown to inhibit downstream signalling via Akt from TLR2 and TLR4, and as a result decreases pro-inflammatory cytokine production from stimulated human airway macrophages [19]. SP-A also binds to TLR4 and thus blocks binding of LPS to the receptor and subsequent downstream activation signals [20]. Furthermore, SP-A, along with a related family member SP-D, reduces the phagocytic activity of alveolar macrophages by binding to and activating the signal inhibitory regulatory protein alpha (SIRP␣), an inhibitory receptor highly expressed on these cells [12]. MUC1, a transmembrane mucinlike glycoprotein expressed on epithelial cells, suppresses mouse airway epithelial cell and alveolar macrophage TLR 2–5, 7 and 9 signalling pathways, suggesting yet another anti-inflammatory strategy [21]. This plethora of negative regulators maintains airway luminal cells in a quiescent state during homeostasis in a unique environmental niche that is unlikely to be found elsewhere. We have recently identified another novel homeostatic loop mediated by CD200 receptor (CD200R), which is required for homeostasis and resolution of lung myeloid cell activity. CD200 receptor is almost exclusively expressed by myeloid cells, including macrophages and dendritic cells [22–26]. CD200 ligand however is expressed by a variety of cells such as thymocytes, B cells, some peripheral T cells, neurons in the central nervous system and endothelium [27–32]. Binding of CD200 to CD200R imparts a unidirectional negative signal to CD200R bearing cells [22,25–27,33]. All of the cells expressing CD200 ligand can therefore potentially negatively regulate innate myeloid responses. The precise molecular mechanisms leading to suppression via CD200R signalling is not currently known. CD200R lacks ITIM domains commonly found in immune inhibiting receptors that cause recruitment of phosphatases and down regulation of inflammatory pathways. The cytoplasmic tail is 67 amino acids in length and contains 3 tyrosine residues as potential phosphorylation sites. One of these tyrosine residues is located within a NPXY motif, which is phosphorylated upon ligation of the receptor. This leads to the recruitment of Dok1 and Doc-2, which are in turn phosphorlyated and associate with RasGAP and SHIP. In mast cells it is known that this then inhibits the phosphorylation of ERK, P38 and JNK [24]. Alveolar macrophages, unlike counterparts in any other site, express unusually high basal levels of CD200R. Its ligand, CD200, is only expressed on the luminal aspect of the airway epithelium during homeostasis and in vitro studies show that this interaction prevents activation of alveolar macrophages in the presence or absence of inflammatory stimuli. Low levels of CD200R on splenic macrophages can be increased by incubation with IL-10 and TGF. TGF is abundant in the lung and present on respiratory epithelial cells tethered to the intergrin ␣v 6 [34,35]. This together with high levels of IL-10 [36] are likely to increase CD200R on any macrophage trans-migrating into the airspaces and effectively sets up a tissue-specific microenvironment that governs the reactivity of innate immunity. Just taking into account CD200R, TGF and IL10 a picture emerges clearly implying site-specific immunity. We have combined such pathways, and their balance by innate immune potentiators (for example, Toll-like receptors) into a concept called the innate immune rheostat. Rheostats are more commonly found in electrical appliances and a good example is the one found in a dimmer switch for a light bulb. This variable rheostat can be adjusted to dim or brighten the light. Similarly, negative and positive immune pathways form a variable “innate immune rheostat”, which dictates the threshold above which a particle is deemed a threatening antigen leading to an inflammatory response. In the resting airway the alveolar macrophage “innate rheostat” is poised centrally, not too dim and not too bright (Fig. 1A). This concept is also highly relevant to immunity in the gastrointestinal tract. Once again IL-10 is abundant from macrophages [37,38] and possibly regulatory T cells [39] and TGF is provided by the epithelium and resident mast cells [40]. The gut is also abundant in thymic stromal lymphopoietin (TSLP), retinoic acid and vasoactive intestinal peptide that all down-regulate innate immune responses and provide an intestinal specific inhibitory signature (for a review see [41]). Similar to the events likely to occur on migration of macrophages into the airspaces, blood derived monocytes entering the gut will be conditioned by this controlled environment. 3. The airways in homeostasis: immune potentiators What of immune potentiators in the lung during homeostasis? The activity of these is likely to overcome the homeostatic pathways that limit inflammation described above. Once again, site-specific regulation of their activity, distribution and abundance must differ between body compartments. Pattern recognition receptors, the most studied of which are the Toll-like receptors [42], recognise pathogen associated molecular patterns on pathogenic, but also commensal, microorganisms [43]. Their wide distribution on dendritic cells, monocyte/macrophages and epithelial cells [44–46] would make non-sterile mucosal tissues a highly inflammatory environment were it not for their altered threshold of responsiveness [46–49], decreased expression [45,50] and altered distribution [41,51,52] (for a review see [41]). In the intestine there is even evidence to suggest that TLRs prevent inflammation [53] by increasing epithelial integrity [54] and promoting B cell responses and IgA production [55]. In the colon suppression of TLR responses is mediated by an increase of negative regulators such as IRAKM [56], SIGIRR [57] and Tollip [58]. In the lung however, much less is known about the expression and particularly the regulation of immune potentiators such as TLRs on airway macrophages and the vast epithelial surface. TLRs are clearly expressed on human bronchial epithelial cells and can respond to their agonists [47,59] (for a review see [47,60,61]). However, like the gut epithelium expression may be limited by site-specific regulatory mechanisms [47,62]. Other pattern recognition receptors are also present throughout the respiratory tree epithelium including the trachea [47]. TLR4 and the accessory molecule MD-2 are constitutively expressed in human alveolar and bronchial epithelial cells, though flow cytometry and confocal microscopy reveal them to be intracellular rather than displayed on the surface. Once again Please cite this article in press as: Wissinger E, et al. Immune homeostasis in the respiratory tract and its impact on heterologous infection. Semin Immunol (2009), doi:10.1016/j.smim.2009.01.005 G Model YSMIM-695; No. of Pages 9 ARTICLE IN PRESS E. Wissinger et al. / Seminars in Immunology xxx (2009) xxx–xxx 3 Fig. 1. Schematic representation of the lung innate immune rheostat in homeostasis (A), during inflammation (B) and in the influenza resolved lung (C). In homeostasis CD200 on alveolar macrophages is restrained by epithelial CD200. The levels of CD200R are dictated by the immune suppressive cytokines IL-10 and TGF. Toll-like receptors (TLRs) are present and functional but over-ridden by CD200R and immune suppressive cytokines. The immune rheostat is poised between regulation and inflammation (A). During inflammation (B), CD200, TGF and possibly IL-10 is lost from the epithelium. Macrophages are released to become inflammatory. Furthermore, the immune potentiator OX40L is up-regulated that binds to OX40 on incoming activated T cells. This pushes the innate immune rheostat further towards inflammation. Inflammation thus overrides regulation. During resolution (C), CD200R levels are increased beyond that in homeostasis as are IL-10 levels, TLR responses are blunted and TGF restored. OX40L is still present but OX40+ T cells are absent. Add to this blunted TLR responses and the innate immune rheostat is positioned heavily towards regulation. It is at this stage bacterial pneumonia and subsequent sepsis occurs. this implies a site-specific strategy for limiting immediate inflammation [63], though pathways affecting their localisation are not currently known. TLR expression on airway macrophages is less well understood, parenchymal counterparts appear to respond in a similar manner to those in other “sterile” environments, whereas airway macrophages are altered, in their responsiveness at least, by airway specific factors such as surfactant proteins [19,20] and possibly cell surface receptors such as CD44 that limit responsiveness of murine alveolar macrophages via the intracellular negative regulators IRAK-M, Tollip and A20 [64]. Human alveolar macrophages in homeostasis express TLR2 [65] and though LPS stimulation upand down-regulates a variety of TLRs [66] their expression in homeostasis remains unclear. Quite what causes specific alterations of TLR activity or distribution is currently being investigated but is likely to involve multiple pathways including signalling via CD200R, TGFR and IL-10R. Sitespecific regulation of resident innate immune cells is thus very important for mucosal surfaces and will be dictated by the physiology of each individual tissue [1]. Indeed maturation of even bone marrow derived macrophages using different conditions in vitro alters their responsiveness to bacterial products [67]. As we will allude to later, however, this site-specific regulation is likely to be modified by past infection history and will not necessarily return to its original homeostatic state after inflammatory resolution. 4. Overcoming innate homeostasis and adjusting the innate immune rheostat towards inflammation In both the lung and gut the tight control of innate immunity must be overcome in order for inflammation to proceed. In both sites it is likely that epithelial integrity is paramount and once this is inflamed or breached site-specific homeostasis is lost. Though pattern recognition receptors have an altered distribution and responsiveness in mucosal tissues these too will be adjusted in an inflamed environment or the threshold required to activate cells expressing them exceeded. Signalling via one TLR in alveolar macrophages profoundly changes the pattern of expression of others [66,68]. Exposure of alveolar macrophages to oxidative stress enhances exocytosis and hence surface expression of TLR4, that can be reversed with anti-oxidants [69]. Stimulation of alveolar macrophages through TLR2, TLR4, or TLR9 inhibits IL-10R signal transduction and releases them from the suppression usually mediated by epithelial produced IL-10 [36]. Intestinal epithelial cells are usually refractory to TLR4 signalling that is overcome by exposure to IFN␥ and perhaps signalling via other TLRs [70]. IFN␥ and TNF up-regulate TLR2 in respiratory epithelial cells [71] that is usually suppressed by promoter hypomethylation [72]. The inhibition of T cells responses by alveolar macrophages is overcome by the addition of pro-inflammatory cytokines such as GM-CSF and TNF␣ [73,74]. Once activated alveolar macrophages generally display a greater phagocytic capacity [75] with a higher oxidative burst and pro-inflammatory cytokine production [9], in keeping with their role as a first line of defence in the respiratory tract. A number of pathogens in the lung and gut adhere to, or directly infect, the mucosal epithelium. Lung epithelial cells upregulate Toll-like receptors during respiratory syncytial virus and influenza infection, which may be mediated by the release of IFN by infected macrophages [62,76,77]. This would result in the liberation of inflammatory mediators from a vast surface area. Furthermore, within the first 4 h of Pseudomonas aeruginosa infection NFB activity is mainly detected within the bronchial epithelium [78]. Inflammation and pathogen replication may also result in the breakdown of epithelial integrity. A continuous epithelial barrier is vital to physically exclude exogenous organisms from the body’s interior. Epithelial disruption doesn’t just open the gates to within but also allows organisms access to macrophages and other potent antigen presenting cells that may be much less regulated than luminal counterparts. This is especially true in the respiratory tract. Please cite this article in press as: Wissinger E, et al. Immune homeostasis in the respiratory tract and its impact on heterologous infection. Semin Immunol (2009), doi:10.1016/j.smim.2009.01.005 G Model YSMIM-695; No. of Pages 9 4 ARTICLE IN PRESS E. Wissinger et al. / Seminars in Immunology xxx (2009) xxx–xxx Airway macrophages are suppressed by IL-10, TGF and CD200R (and a plethora of other molecules), whereas tissue macrophages are less so. A sub-mucosal macrophage response to an organism is therefore likely to be qualitatively and quantitatively different. Furthermore, disruption of the epithelium causes the loss of many regulatory pathways. Toll-like receptor signalling causes a down regulation of the ␣v 6 integrin that tethers TGF to the epithelial surface in the lung [34]. Epithelial expression of CD200 is also reduced, releasing the airway macrophage from inhibition via CD200R. A lack of signals through CD200R results in higher inflammatory cytokine, chemokine and reactive metabolite release from macrophages [79]. Blood derived monocytes and also adaptive immune cells entering this site are thus conditioned to be inflammatory as the calming environment has been lost. Inflammation often perpetuates inflammation through autocrine and paracrine pathways. The innate immune rheostat is thus firmly set to the inflammatory position (Fig. 1B). 5. Return to homeostasis How then does peace return, and does the environment regain its original homeostatic state? It can often take more effort (by the same pathways) to return to homeostasis after inflammation than to maintain it in the first place. Homeostatic pathways prevent inflammation in the first instance, limit its magnitude once initiated and mediate resolution. However, the importance and activity required of homeostatic pathways will vary at each of these stages. For example, CD200R is high on resting alveolar macrophages compared to tissue-resident counterparts. On resolution of influenza induced inflammation however at day 14, CD200R intensity (determined by the geometric mean of fluorescence by flow cytometry) is exponentially higher on airway macrophages, and remains so for some time [79]. It is possible that this represent an overshoot in mechanisms trying to regain control of innate immunity in the airspaces. A similar case could be made for IL-10. In homeostasis IL-10 contributes to maintain a peaceful microenvironment. During influenza infection however, lymphocytes and macrophages are recruited that can also produce IL-10 [80]. CD11c expressing cells capable of producing IL-10 are maintained in the lung and display enhanced antigen presentation long after the resolution of an influenza or RSV primary infection [81,82]. Furthermore DCs that remain in the lung several weeks after infection have a more activated phenotype [81] and may also contribute to prolonged IL-10 concentrations in the airspaces. In influenza recovered mice a 50fold increase in IL-10 is observed that depletion studies suggest is responsible for subsequent susceptibility to secondary bacterial colonisation in the lung [83]. TGF is secreted by virtually all cells as a biologically inactive protein termed latent TGF [84]. As TGF receptors are widely and constitutively expressed, regulation of this pathway is mediated dominantly by the balance between the latent and active form of this cytokine. In vitro studies show that influenza viral neuraminidase (NA) directly activates latent TGF, possibly through cleavage of the sialic acid residues on the amino-terminal latencyassociated peptide (LAP) that remains non-covalently associated with the carboxy-terminal mature TGF molecule [85]. Though influenza infection may increase TGF levels during active infection of the lung resolved homeostatic levels have not yet been ascertained. The up-regulation of IL-10 and CD200R levels alone long after influenza virus has been cleared would reset the innate immune rheostat below its prior homeostatic level. In addition, however, we are also faced with a long term alteration of immune potentiator pathways. Our recent study suggests that TLR responsiveness itself in alveolar macrophages (and possibly respiratory epithelial and dendritic cells) is blunted for long periods of time after influenza has been cleared from the lung [86]. This long term direct or indirect de-sensitisation of lung alveolar macrophages to the TLR ligands Flagellin, LPS and lipoteichoic acid (LTA) culminates in impaired NFkB nuclear translocation, inflammatory cytokine production and cellular recruitment. This phenomenon is not simple TLR crosstolerance, whereby TLR-activated cells are, for a short period of time, refractory to subsequent TLR stimulation [87] as the effect persists for months after the initial infection. Taking into account the slow turn over of airway macrophages [88], it is clear that the innate responsiveness of sentinel cells in the airway is molded by prior infection history. This subtle alteration of responsiveness with time and after each wave of infection is not unique to the lung. In the gut, the microbial flora plays an essential role in mucosal homeostasis by actively inhibiting intestinal innate responses (for example see [89]). Furthermore, responsiveness of intestinal epithelial cells to TLR activation is impaired immediately after birth by exposure to exogenous endotoxin [90]. Inflammatory resolution therefore produces a different type of status quo (see Fig. 1C). In the second half of this review we will examine some of the consequences of altering the innate immune rheostat. 6. The consequences of an altered homeostatic state in the lung after inflammation has subsided It is well established that two infections lead to a different pathological outcome compared to each alone. The lung microenvironment and its homeostatic profile can be altered considerably by prior events that leave behind long term consequences. These prior events may not be infectious. Emphysema, for example, enhances TLR2 and TLR4 leading to enhanced inflammation during Streptococcus pneumoniae pulmonary infection [91], whereas morphine reduces TLR9 induced NFB signalling and impairs S. pneumoniae clearance [92]. Cigarette smoke and COPD decrease TLR2 expression on alveolar macrophages potentially leaving the host susceptible to respiratory bacteria [93,94]. Ethanol and burn injury lead to a marked cellular infiltration in the lung and gut, higher serum inflammatory cytokines and a poor prognosis after pulmonary pseudomonas infection [95]. In the case of burn injury the alterations in a distant organ such as the lung is thought to arise from gut-derived factors carried in the mesenteric lymph that alter lung vascular permeability [96]. Finally, individuals may have underlying genetic alterations [97,98] that affect homeostasis and the ability to limit commensal organisms. C3H/HEj mice, for example, have increased terminal airspaces, three times more alveolar macrophages and enhanced matrix metalloproteinase 12, MCP-1 and KC, but also enhanced recoverable bacteria from the lungs compared to other mouse strains [99]. It is likely that polymorphisms in the regulatory or immune potentiator pathways described previously will also impact on immune homeostasis in the lung leading to altered responsiveness to the same pathogen within a population. In the remainder of this review however, we will focus on how lung infections alter the outcome for subsequent respiratory pathogens. 7. Innate imprinting and susceptibility to infection The lungs response to infection will depend on each individual’s position on the innate immune rheostat. Infection of the lung in the absence of prior infection will produce a different outcome to the same pathogen infecting a lung with resolved inflammation. This alteration is not restricted to latent or concurrent infections but can also be influenced by acute inflammatory lung disease. Epidemio- Please cite this article in press as: Wissinger E, et al. Immune homeostasis in the respiratory tract and its impact on heterologous infection. Semin Immunol (2009), doi:10.1016/j.smim.2009.01.005 G Model YSMIM-695; No. of Pages 9 ARTICLE IN PRESS E. Wissinger et al. / Seminars in Immunology xxx (2009) xxx–xxx logical and animal model data suggest that influences from prior unrelated pathogens may be long lasting [100–102]. An acute pulmonary influenza infection, for example, alters immunopathology to respiratory syncytial virus and heightened clearance of vaccinia virus is evident in lymphocytic choriomeningitis virus (LCMV) immune mice [102–104]. The outcome however is not always beneficial and may depend on the precise sequence of infection. Though influenza inhibits vaccinia virus replication it enhances the titres of LCMV and MCMV [104]. In addition to the de-sensitisation of the lung microenvironment to TLR ligands by influenza described above [86], some cause a skewing of the final cytokine profile of T cells responding to a second unrelated lung pathogen. For example, lung BCG infection improves the outcome during infection with the fungal pathogen Cryptococcus neoformans. In C57BL/6 mice C. neoformans induces a non-protective Th2 response in the lungs culminating in eosinophilic lung disease and systemic spread of the organism [105]. Prior BCG infection however skews the immune towards a protective Th1 response [106]. This is similar to the influence of Th1 inducing infections or antigens on the development of allergy and the subsequent rise in allergy due to a clean environment—the hygiene hypothesis (reviewed elsewhere [107]). Even the transient immunity evoked by pathogen products can have an impact on heterologous immunity. Microbial products such as CpG DNA or a modified bacterial labile toxin (LTK63) afford protection against a variety of subsequent respiratory pathogens [108,109]; some by altering a Th2 to a Th1 cytokine response [108] and others by maturation of antigen presenting cells in the lung microenvironment [109]. Microarray analysis shows that the modified E. coli endotoxin, LTK63, induces a transient innate and adaptive immune response by itself [110], but long after these effects have subsided it reduces inflammation to a subsequent RSV and influenza pulmonary infection [109]. This alteration does not impact on pathogen clearance, which in the case of influenza is actually improved. This phenomenon in a number of cases does not involve cross-reactive T and B cells and is evident even in LTK63 treated RAG knock out mice. Prior infection or particulate stimulation thus alters the innate immune rheostat making the cells involved behave in a qualitatively and quantitatively different manner. It is likely that other environmental particulates adjust the lung microenvironment in a similar manner as we alluded to above, though studies in this area are only beginning to appear. Even events in the gut impact on lung immunity. Colonic restricted Citrobacter rodentium infection modulates the usual Th2 driven pathology to lung C. neoformans infection by skewing the immune response towards a Th1 cytokine profile [111]. Intraperitoneal injection of LPS into rats that have had their mesenteric lymph duct ligated attenuates lung injury, lung permeability, and PMN CD11b expression [112], suggesting gut-derived soluble factors or migrating cells influence distant organs or that gut/mesenteric lymph derived products (such as lipoproteins) usually blunt pulmonary responses in health [113]. The longer term impact of gut inflammation on lung immune homeostasis and response to infection however has not been studied. The impact on the lung by spill over of inflammatory cells and cytokines from distant sites has been examined with regards to more persistent infection. It is important to note however, that the impact on the lung innate immune rheostat (in the absence of additional lung infection) is not known; i.e. what do chronic infections do to the lung per se? Helminths provide a clear example of a prolonged infection that can alter immune reactivity elsewhere. They generally induce excessive Th2 cytokine dominated immunity that could impact on Th1 associated respiratory infections [114–116]. Similarly, the induction of regulatory T cells to one infection may impact on others in a bystander fashion. Mycobacteria, malaria and parasitic protozoa and helminths induce high levels of immune suppressive cytokines (TGF and IL-10) that could reduce immunity 5 to subsequent or concurrent infection in the respiratory tract. Vaccines proven to be efficient in high income countries might perform less well in low income countries [117] for the very same reasons. Lung infections can also have an impact on other sites. Pulmonary murine gamma herpes virus latency affects peritoneal macrophages for up to 2 months with increased activation and expression of MHC class II. Latent herpes virus infection affords resistance to subsequent intranasal or intraperitoneal infection with Listeria monocytogenes or Yersinia pestis [118] and modulates the host inflammatory responses and susceptibility to mouse adenovirus type 1 [119]. Similar to our observations [86,102] this protection is not due to cross-reactive antigens but involves prolonged production of the anti-viral cytokines, systemic activation of macrophages and an alteration of basal innate immunity. Based on prior events both within and external to the lung we are therefore all unique with respect to responsiveness to respiratory infection [120]. 8. Innate imprinting and secondary bacterial pneumonia Another significant consequence of lung infection, influenza in particular, is the pre-disposition to secondary bacterial pneumonia. This is often regarded as a complication during influenza induced damage. However the influence of respiratory viral infection can actually be long lasting leaving the host susceptible to bacterial pneumonia long after the virus has been cleared [86]. Once again, the outcome of lung bacterial infection will depend on the position of the innate immune rheostat. Influenza causes significant and well publicised mortality as a single infection, but in combination with a secondary bacterial pneumonia is far more severe [121]. With a bacterial co-infection it ranks the 7th leading cause of mortality (5th in children) in the United States alone [122]. Amongst the 40–50 million deaths during the 1918–1919 influenza pandemic a large proportion had co-existing bacterial pneumonia ([123] and references therein). Re-cut autopsy tissue specimens taken from those that died in the 1918–1919, and also the 1957 and 1968, pandemic showed a high frequency of a variety of different secondary bacterial organisms in those infected with influenza, and in some cases multiple bacterial species were present [123]. A wealth of clinical and animal model evidence proves that combined infections are worse than each alone. Fatalities in the 1957 influenza pandemic were higher in those with a co-existing respiratory bacterium [124]. Furthermore, seasonal influenza vaccination reduces mortality to combined bacterial infection [125] and anti-virals that target the viral neuraminidase prevent or slow respiratory bacterial infection in influenza infected mice [126,127]. Secondary bacterial complications are not a feature of influenza virus alone. Rhinovirus, respiratory syncytial virus and enteroviruses also induce viral wheezing that is invariably associated with bacterial infection leading to acute otitis media, sinusitis, interstitial pneumonia and, less frequently, alveolar pneumonia [128]. Furthermore, the low risk of concurrent bacterial infection is enhanced in pre-term infants hospitalised with RSV. Co-infection doubles the mean length of stay and bacterial isolates from those in the intensive care unit include S. pneumoniae, C. pneumoniae and a combination of S. pneumoniae with Haemophilus influenzae [129]. Analysis of children admitted to paediatric intensive care for RSV infection during three consecutive seasons reveals that 40% of them have a secondary bacterium in their lower airways [130]. This effect can be reproduced in mice where RSV infection decreases bacterial clearance due to functional alteration of neutrophils [131]. The reasons for enhanced susceptibility to bacterial pneumonia during influenza infection have been studied extensively (see Fig. 2) but the pre-disposition caused by other respiratory infections is less well known. Influenza is a cytopathic (lytic) virus Please cite this article in press as: Wissinger E, et al. Immune homeostasis in the respiratory tract and its impact on heterologous infection. Semin Immunol (2009), doi:10.1016/j.smim.2009.01.005 G Model YSMIM-695; 6 No. of Pages 9 ARTICLE IN PRESS E. Wissinger et al. / Seminars in Immunology xxx (2009) xxx–xxx Fig. 2. The consequences of influenza infection that lead to secondary bacterial pneumonia. The airways in homeostasis are dominated by airway macrophages that are suppressed by site-specific regulatory pathways (A). Influenza can pre-dispose to other infections by causing apoptosis of airway epithelial cells. Opportunistic bacteria then gain entry to the body’s interior (barrier breakdown, B). Influenza, and the inflammatory environment it induces, causes the up-regulation of bacterial adhesins making the lung stickier for other organisms (C). In addition to the lysis of respiratory epithelial cells, influenza is reported to induce apoptosis of neutrophils and macrophages that are crucial for bacterial clearance (immune subversion, D). Finally, influenza induces a long term state of responsiveness to subsequent TLR signalling and so bacteria go unrecognised for longer (TLR de-sensitisation, E). that causes epithelial barrier disruption. An increase in bacterial adhesion molecules and apoptosis of anti-bacterial immune cells such as alveolar macrophages and neutrophils [126,132,133] is also apparent. Furthermore, IFN␥ production during influenza infection decreases the phagocytic and anti-bacterial, capacity of alveolar macrophages [134]. The influenza encoded neuraminidase also contributes significantly to a localised immune suppression within the lung microenvironment, by cleaving sialic acid residues from IgA and ␥␦ T cells; in the case of the latter, this may alter their potential to home to mucosal tissues [135]. However, considering the position of our innate immune rheostat in resolution it is likely that a de-sensitisation or blunting of alveolar macrophage responses to bacterial danger signals (Toll-like receptor ligands) [86] and an increase in CD200R [79] also contribute to this susceptible state. Influenza therefore raises the threshold for myeloid cell recognition of bacteria. We are not implying that the innate immune rheostat during resolution occurs in everyone infected with influenza. Some succumb to influenza infection, others do not. In a proportion of those that succumb a secondary infection with a bacterium may occur or not. Even in that event, some will handle the combined infection. However, a significant proportion will not and it is in those an adjustment of the innate immune rheostat may be beneficial. To support this, as we alluded to earlier, lung IL-10 production is enhanced and sustained after a secondary pneumococcal or meningococcal challenge in mice that have experienced an influenza infection, which in turn impairs the neutrophils ability to clear bacteria [136,137]. 9. Concluding remarks In inflammatory disease we often refer to a return to homeostasis. This implies that regulatory and inflammatory signalling pathways, Toll-like receptor expression, negative regulatory receptors, and even connective and neuronal support networks return to an original starting point. Mouse simulations of respiratory disease and clinical and epidemiological data clearly suggest this is not the case. This is not some form of “innate memory” as we do not believe individual innate cells are adjusted in isolation. Rather it is more likely that a combination of subtle alterations (in multiple pathways) leads to an alteration in the particular cells analysed. For example, alveolar macrophages have higher levels of CD200R long after resolution of inflammation because other cells (most likely epithelial cells) secrete higher levels of IL-10 and possibly TGF. The higher secretion of these cytokines is in turn likely to be a result of altered epithelial cell homeostasis that is dictated by other stromal elements or even altered innervation in the resolved lung. These modifications over time do make evolutionary sense as in some instances it provides a beneficial environment equipped to handle the next infection more professionally. In a proportion, however, a particular sequence of events, or the same events on a different genetic background, in different environmental conditions, may lead to a worse outcome including the development of fatal secondary bacterial pneumonia described above. The status of the innate immune rheostat in the lung may also explain the difficulty in generating efficacy to aerosolised vaccines. The Please cite this article in press as: Wissinger E, et al. Immune homeostasis in the respiratory tract and its impact on heterologous infection. Semin Immunol (2009), doi:10.1016/j.smim.2009.01.005 G Model YSMIM-695; No. of Pages 9 ARTICLE IN PRESS E. Wissinger et al. / Seminars in Immunology xxx (2009) xxx–xxx lung and gut possess a variety of overlapping strategies to prevent inflammation where possible. This anti-inflammatory environment will alter with time and those alterations may raise the threshold required for innate activation. We are only beginning to understand regulatory networks in the lung environment. It is clear the epithelium has a much bigger role to play than providing a (semi)-impermeable barrier. It is also clear that maintenance of homeostasis, even the altered homeostasis in inflammatory resolution, is an adaptable, active process. There are extensive gaps in our knowledge on the signalling events downstream of many receptors on alveolar macrophages and particularly the interplay between immune potentiators and regulators. A thorough understanding of these concepts will help explain the variability of infectious disease in man, provide possibilities for therapeutic intervention during inflammatory lung disease and may assist in the design of vaccine strategies that can bypass stringent immune regulation in mucosal tissues. Acknowledgements This work was supported by the Medical Research Council (G0400795) and the National Institute of Health (AI070232-10). References [1] Raz E. Organ-specific regulation of innate immunity. Nat Immunol 2007;8(1):3–4. [2] Matzinger P. Friendly and dangerous signals: is the tissue in control? Nat Immunol 2007;8(1):11–3. [3] Bingisser RM, Holt PG. Immunomodulating mechanisms in the lower respiratory tract: nitric oxide mediated interactions between alveolar macrophages, epithelial cells, and T-cells. Swiss Med Wkly 2001;131(13–14):171–9. [4] Munger JS, Huang X, Kawakatsu H, Griffiths MJ, Dalton SL, Wu J, et al. The integrin alpha v beta 6 binds and activates latent TGF beta 1: a mechanism for regulating pulmonary inflammation and fibrosis. Cell 1999;96(3):319–28. [5] Kuolee R, Chen W. M cell-targeted delivery of vaccines and therapeutics. Expert Opin Drug Deliv 2008;5(6):693–702. [6] Kraehenbuhl JP, Neutra MR. Epithelial M cells: differentiation and function. Annu Rev Cell Dev Biol 2000;16:301–32. [7] Jahnsen FL, Strickland DH, Thomas JA, Tobagus IT, Napoli S, Zosky GR, et al. Accelerated antigen sampling and transport by airway mucosal dendritic cells following inhalation of a bacterial stimulus. J Immunol 2006;177(9):5861–7. [8] Chieppa M, Rescigno M, Huang AY, Germain RN. Dynamic imaging of dendritic cell extension into the small bowel lumen in response to epithelial cell TLR engagement. J Exp Med 2006;203(13):2841–52. [9] Steinmuller C, Franke-Ullmann G, Lohmann-Matthes ML, Emmendorffer A. Local activation of nonspecific defense against a respiratory model infection by application of interferon-gamma: comparison between rat alveolar and interstitial lung macrophages. Am J Respir Cell Mol Biol 2000;22(4):481–90. [10] Thepen T, Kraal G, Holt PG. The role of alveolar macrophages in regulation of lung inflammation. Ann NY Acad Sci 1994;725:200–6. [11] Lipscomb MF, Pollard AM, Yates JL. A role for TGF-beta in the suppression by murine bronchoalveolar cells of lung dendritic cell initiated immune responses. Reg Immunol 1993;5(3–4):151–7. [12] Janssen WJ, McPhillips KA, Dickinson MG, Linderman DJ, Morimoto K, Xiao YQ, et al. Surfactant proteins A and D suppress alveolar macrophage phagocytosis via interaction with SIRP alpha. Am J Respir Crit Care Med 2008;178(2):158–67. [13] Roth MD, Golub SH. Human pulmonary macrophages utilize prostaglandins and transforming growth factor beta 1 to suppress lymphocyte activation. J Leukoc Biol 1993;53(4):366–71. [14] Chelen CJ, Fang Y, Freeman GJ, Secrist H, Marshall JD, Hwang PT, et al. Human alveolar macrophages present antigen ineffectively due to defective expression of B7 costimulatory cell surface molecules. J Clin Invest 1995;95:1415–21. [15] Balbo P, Silvestri M, Rossi GA, Crimi E, Burastero SE. Differential role of CD80 and CD86 on alveolar macrophages in the presentation of allergen to T lymphocytes in asthma. Clin Exp Allergy 2001;31(4):625–36. [16] Holt PG, Oliver J, Bilyk N, McMenamin C, McMenamin PG, Kraal G, et al. Downregulation of the antigen presenting cell function(s) of pulmonary dendritic cells in vivo by resident alveolar macrophages. J Exp Med 1993;177(2):397–407. [17] Akbari O, DeKruyff RH, Umetsu DT. Pulmonary dendritic cells producing IL-10 mediate tolerance induced by respiratory exposure to antigen. Nat Immunol 2001;2(8):725–31. [18] Wright JR. Immunoregulatory functions of surfactant proteins. Nat Rev Immunol 2005;5(1):58–68. [19] Henning LN, Azad AK, Parsa KV, Crowther JE, Tridandapani S, Schlesinger LS. Pulmonary surfactant protein A regulates TLR expression and activity in human macrophages. J Immunol 2008;180(12):7847–58. 7 [20] Yamada C, Sano H, Shimizu T, Mitsuzawa H, Nishitani C, Himi T, et al. Surfactant protein A directly interacts with TLR4 and MD-2 and regulates inflammatory cellular response. Importance of supratrimeric oligomerization. J Biol Chem 2006;281(31):21771–80. [21] Ueno K, Koga T, Kato K, Golenbock DT, Gendler SJ, Kai H, et al. MUC1 mucin is a negative regulator of toll-like receptor signaling. Am J Respir Cell Mol Biol 2008;38(3):263–8. [22] Wright GJ, Puklavec MJ, Willis AC, Hoek RM, Sedgwick JD, Brown MH, et al. Lymphoid/neuronal cell surface OX2 glycoprotein recognizes a novel receptor on macrophages implicated in the control of their function. Immunity 2000;13(2):233–42. [23] Wright GJ, Cherwinski H, Foster-Cuevas M, Brooke G, Puklavec MJ, Bigler M, et al. Characterization of the CD200 receptor family in mice and humans and their interactions with CD200. J Immunol 2003;171(6):3034–46. [24] Zhang S, Cherwinski H, Sedgwick JD, Phillips JH. Molecular mechanisms of CD200 inhibition of mast cell activation. J Immunol 2004;173(11):6786–93. [25] Cherwinski HM, Murphy CA, Joyce BL, Bigler ME, Song YS, Zurawski SM, et al. The CD200 receptor is a novel and potent regulator of murine and human mast cell function. J Immunol 2005;174(3):1348–56. [26] Shiratori I, Yamaguchi M, Suzukawa M, Yamamoto K, Lanier LL, Saito T, et al. Down-regulation of basophil function by human CD200 and human herpesvirus-8 CD200. J Immunol 2005;175(7):4441–9. [27] Barclay AN, Ward HA. Purification and chemical characterisation of membrane glycoproteins from rat thymocytes and brain, recognised by monoclonal antibody MRC OX 2. Eur J Biochem 1982;129(2):447–58. [28] Hoek RM, Ruuls SR, Murphy CA, Wright GJ, Goddard R, Zurawski SM, et al. Down-regulation of the macrophage lineage through interaction with OX2 (CD200). Science 2000;290(5497):1768–71. [29] Wright GJ, Jones M, Puklavec MJ, Brown MH, Barclay AN. The unusual distribution of the neuronal/lymphoid cell surface CD200 (OX2) glycoprotein is conserved in humans. Immunology 2001;102(2):173–9. [30] Webb M, Barclay AN. Localisation of the MRC OX-2 glycoprotein on the surfaces of neurones. J Neurochem 1984;43(4):1061–7. [31] Dick AD, Broderick C, Forrester JV, Wright GJ. Distribution of OX2 antigen and OX2 receptor within retina. Invest Ophthalmol Vis Sci 2001;42(1): 170–6. [32] Bukovsky A, Presl J, Zidovsky J. Association of some cell surface antigens of lymphoid cells and cell surface differentiation antigens with early rat pregnancy. Immunology 1984;52(4):631–40. [33] Nathan C, Muller WA. Putting the brakes on innate immunity: a regulatory role for CD200? Nat Immunol 2001;2(1):17–9. [34] Takabayshi K, Corr M, Hayashi T, Redecke V, Beck L, Guiney D, et al. Induction of a homeostatic circuit in lung tissue by microbial compounds. Immunity 2006;24(4):475–87. [35] Morris DG, Huang X, Kaminski N, Wang Y, Shapiro SD, Dolganov G, et al. Loss of integrin alpha(v)beta6-mediated TGF-beta activation causes Mmp12dependent emphysema. Nature (London) 2003;422(6928):169–73. [36] Fernandez S, Jose P, Avdiushko MG, Kaplan AM, Cohen DA. Inhibition of IL10 receptor function in alveolar macrophages by Toll-like receptor agonists. J Immunol 2004;172(4):2613–20. [37] Hirotani T, Lee PY, Kuwata H, Yamamoto M, Matsumoto M, Kawase I, et al. The nuclear IkappaB protein IkappaBNS selectively inhibits lipopolysaccharideinduced IL-6 production in macrophages of the colonic lamina propria. J Immunol 2005;174(6):3650–7. [38] Kamada N, Hisamatsu T, Okamoto S, Sato T, Matsuoka K, Arai K, et al. Abnormally differentiated subsets of intestinal macrophage play a key role in Th1-dominant chronic colitis through excess production of IL-12 and IL-23 in response to bacteria. J Immunol 2005;175(10):6900–8. [39] Asseman C, Mauze S, Leach MW, Coffman RL, Powrie F. An essential role for interleukin 10 in the function of regulatory T cells that inhibit intestinal inflammation. J Exp Med 1999;190(7):995–1004. [40] Avery A, Paraskeva C, Hall P, Flanders KC, Sporn M, Moorghen M. TGF-beta expression in the human colon: differential immunostaining along crypt epithelium. Br J Cancer 1993;68(1):137–9. [41] Platt AM, Mowat AM. Mucosal macrophages and the regulation of immune responses in the intestine. Immunol Lett 2008;119(1–2):22–31. [42] Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell 2006;124(4):783–801. [43] Kelly D, Conway S. Bacterial modulation of mucosal innate immunity. Mol Immunol 2005;42(8):895–901. [44] Mayer AK, Dalpke AH. Regulation of local immunity by airway epithelial cells. Arch Immunol Ther Exp (Warsz) 2007;55(6):353–62. [45] Abreu MT, Vora P, Faure E, Thomas LS, Arnold ET, Arditi M. Decreased expression of Toll-like receptor-4 and MD-2 correlates with intestinal epithelial cell protection against dysregulated proinflammatory gene expression in response to bacterial lipopolysaccharide. J Immunol 2001;167(3):1609–16. [46] Melmed G, Thomas LS, Lee N, Tesfay SY, Lukasek K, Michelsen KS, et al. Human intestinal epithelial cells are broadly unresponsive to Toll-like receptor 2dependent bacterial ligands: implications for host-microbial interactions in the gut. J Immunol 2003;170(3):1406–15. [47] Mayer AK, Muehmer M, Mages J, Gueinzius K, Hess C, Heeg K, et al. Differential recognition of TLR-dependent microbial ligands in human bronchial epithelial cells. J Immunol 2007;178(5):3134–42. [48] Jin J, Zeng H, Schmid KW, Toetsch M, Uhlig S, Moroy T. The zinc finger protein Gfi1 acts upstream of TNF to attenuate endotoxin-mediated inflammatory responses in the lung. Eur J Immunol 2006;36(2):421–30. Please cite this article in press as: Wissinger E, et al. Immune homeostasis in the respiratory tract and its impact on heterologous infection. Semin Immunol (2009), doi:10.1016/j.smim.2009.01.005 G Model YSMIM-695; 8 No. of Pages 9 ARTICLE IN PRESS E. Wissinger et al. / Seminars in Immunology xxx (2009) xxx–xxx [49] Punturieri A, Alviani RS, Polak T, Copper P, Sonstein J, Curtis JL. Specific engagement of TLR4 or TLR3 does not lead to IFN-beta-mediated innate signal amplification and STAT1 phosphorylation in resident murine alveolar macrophages. J Immunol 2004;173(2):1033–42. [50] Suzuki K, Suda T, Naito T, Ide K, Chida K, Nakamura H. Impaired toll-like receptor 9 expression in alveolar macrophages with no sensitivity to CpG DNA. Am J Respir Crit Care Med 2005;171(7):707–13. [51] Hornef MW, Normark BH, Vandewalle A, Normark S. Intracellular recognition of lipopolysaccharide by toll-like receptor 4 in intestinal epithelial cells. J Exp Med 2003;198(8):1225–35. [52] Gewirtz AT, Navas TA, Lyons S, Godowski PJ, Madara JL. Cutting edge: bacterial flagellin activates basolaterally expressed TLR5 to induce epithelial proinflammatory gene expression. J Immunol 2001;167(4):1882–5. [53] Vijay-Kumar M, Gewirtz AT. Guardians of the gut: newly appreciated role of epithelial toll-like receptors in protecting the intestine. Gastroenterology 2008;135(2):351–4. [54] Cario E, Gerken G, Podolsky DK. Toll-like receptor 2 controls mucosal inflammation by regulating epithelial barrier function. Gastroenterology 2007;132(4):1359–74. [55] Shang L, Fukata M, Thirunarayanan N, Martin AP, Arnaboldi P, Maussang D, et al. Toll-like receptor signaling in small intestinal epithelium promotes B-cell recruitment and IgA production in lamina propria. Gastroenterology 2008;135(2):529–38. [56] Kobayashi K, Hernandez LD, Galan JE, Janeway Jr CA, Medzhitov R, Flavell RA. IRAK-M is a negative regulator of Toll-like receptor signalling. Cell 2002;110(2):191–202. [57] Xiao H, Gulen MF, Qin J, Yao J, Bulek K, Kish D, et al. The Toll-interleukin-1 receptor member SIGIRR regulates colonic epithelial homeostasis, inflammation, and tumorigenesis. Immunity 2007;26(4):461–75. [58] Zhang G, Ghosh S. Negative regulation of toll-like receptor-mediated signaling by Tollip. J Biol Chem 2002;277(9):7059–65. [59] Platz J, Beisswenger C, Dalpke A, Koczulla R, Pinkenburg O, Vogelmeier C, et al. Microbial DNA induces a host defense reaction of human respiratory epithelial cells. J Immunol 2004;173(2):1219–23. [60] Greene CM, McElvaney NG. Toll-like receptor expression and function in airway epithelial cells. Arch Immunol Ther Exp (Warsz) 2005;53(5):418–27. [61] Hippenstiel S, Opitz B, Schmeck B, Suttorp N. Lung epithelium as a sentinel and effector system in pneumonia–molecular mechanisms of pathogen recognition and signal transduction. Respir Res 2006;7:97. [62] Groskreutz DJ, Monick MM, Powers LS, Yarovinsky TO, Look DC, Hunninghake GW. Respiratory syncytial virus induces TLR3 protein and protein kinase R, leading to increased double-stranded RNA responsiveness in airway epithelial cells. J Immunol 2006;176(3):1733–40. [63] Guillot L, Medjane S, Le-Barillec K, Balloy V, Danel C, Chignard M, et al. Response of human pulmonary epithelial cells to lipopolysaccharide involves Toll-like receptor 4 (TLR4)-dependent signaling pathways: evidence for an intracellular compartmentalization of TLR4. J Biol Chem 2004;279(4):2712–8. [64] Liang J, Jiang D, Griffith J, Yu S, Fan J, Zhao X, et al. CD44 is a negative regulator of acute pulmonary inflammation and lipopolysaccharide-TLR signaling in mouse macrophages. J Immunol 2007;178(4):2469–75. [65] Droemann D, Goldmann T, Branscheid D, Clark R, Dalhoff K, Zabel P, et al. Tolllike receptor 2 is expressed by alveolar epithelial cells type II and macrophages in the human lung. Histochem Cell Biol 2003;119(2):103–8. [66] Maris NA, Dessing MC, de Vos AF, Bresser P, Van der Zee JS, Jansen HM, et al. Toll-like receptor mRNA levels in alveolar macrophages after inhalation of endotoxin. Eur Respir J 2006;28(3):622–6. [67] Gersuk GM, Razai LW, Marr KA. Methods of in vitro macrophage maturation confer variable inflammatory responses in association with altered expression of cell surface dectin-1. J Immunol Methods 2008;329(1–2):157–66. [68] Oshikawa K, Sugiyama Y. Regulation of toll-like receptor 2 and 4 gene expression in murine alveolar macrophages. Exp Lung Res 2003;29(6):401–12. [69] Powers KA, Szaszi K, Khadaroo RG, Tawadros PS, Marshall JC, Kapus A, et al. Oxidative stress generated by hemorrhagic shock recruits Toll-like receptor 4 to the plasma membrane in macrophages. J Exp Med 2006;203(8):1951–61. [70] Abreu MT, Arnold ET, Thomas LS, Gonsky R, Zhou Y, Hu B, et al. TLR4 and MD2 expression is regulated by immune-mediated signals in human intestinal epithelial cells. J Biol Chem 2002;277(23):20431–7. [71] Homma T, Kato A, Hashimoto N, Batchelor J, Yoshikawa M, Imai S, et al. Corticosteroid and cytokines synergistically enhance toll-like receptor 2 expression in respiratory epithelial cells. Am J Respir Cell Mol Biol 2004;31(4):463–9. [72] Furuta T, Shuto T, Shimasaki S, Ohira Y, Suico MA, Gruenert DC, Kai H. DNA demethylation-dependent enhancement of toll-like receptor-2 gene expression in cystic fibrosis epithelial cells involves SP1-activated transcription. BMC Mol Biol 2008;9:39. [73] Bilyk N, Holt PG. Inhibition of the immunosuppressive activity of resident pulmonary alveolar macrophages by granulocyte/macrophage colonystimulating factor. J Exp Med 1993;177(6):1773–7. [74] Bilyk N, Holt PG. Cytokine modulation of the immunosuppressive phenotype of pulmonary alveolar macrophage populations. Immunology 1995;86(2):231–7. [75] Lohmann-Matthes ML, Steinmuller C, Franke-Ullmann G. Pulmonary macrophages. Eur Respir J 1994;7(9):1678–89. [76] Guillot L, Le Goffic R, Bloch S, Escriou N, Akira S, Chignard M, et al. Involvement of toll-like receptor 3 in the immune response of lung epithelial cells to double-stranded RNA and influenza A virus. J Biol Chem 2005;280(7):5571–80. [77] Miettinen M, Sareneva T, Julkunen I, Matikainen S. IFNs activate toll-like receptor gene expression in viral infections. Genes Immun 2001;2(6):349–55. [78] Sadikot RT, Zeng H, Joo M, Everhart MB, Sherrill TP, Li B, et al. Targeted immunomodulation of the NF-kappaB pathway in airway epithelium impacts host defense against Pseudomonas aeruginosa. J Immunol 2006;176(8):4923–30. [79] Snelgrove RJ, Goulding J, Didierlaurent AM, Lyonga D, Vekaria S, Edwards L, et al. A critical function for CD200 in lung immune homeostasis and the severity of influenza infection. Nat Immunol 2008;9(9):1074–83. [80] Moore KW, de Waal MR, Coffman RL, O’Garra A. Interleukin-10 and the interleukin-10 receptor. Annu Rev Immunol 2001;19:683–765. [81] Dahl ME, Dabbagh K, Liggitt D, Kim S, Lewis DB. Viral-induced T helper type 1 responses enhance allergic disease by effects on lung dendritic cells. Nat Immunol 2004;5(3):337–43. [82] Beyer M, Bartz H, Horner K, Doths S, Koerner-Rettberg C, Schwarze J. Sustained increases in numbers of pulmonary dendritic cells after respiratory syncytial virus infection. J Allergy Clin Immunol 2004;113(1):127–33. [83] van der Sluijs KF, van Elden LJ, Nijhuis M, Schuurman R, Pater JM, Florquin S, et al. IL-10 is an important mediator of the enhanced susceptibility to pneumococcal pneumonia after influenza infection. J Immunol 2004;172(12):7603–9. [84] Massague J, Cheifetz S, Laiho M, Ralph DA, Weis FM, Zentella A. Transforming growth factor-beta. Cancer Surv 1992;12:81–103. [85] Schultz-Cherry S, Hinshaw VS. Influenza virus neuraminidase activates latent transforming growth factor beta. J Virol 1996;70(12):8624–9. [86] Didierlaurent A, Goulding J, Patel S, Snelgrove R, Low L, Bebien M, et al. Sustained desensitization to bacterial Toll-like receptor ligands after resolution of respiratory influenza infection. J Exp Med 2008;205(2):323–9. [87] Dobrovolskaia MA, Medvedev AE, Thomas KE, Cuesta N, Toshchakov V, Ren T, et al. Induction of in vitro reprogramming by Toll-like receptor (TLR)2 and TLR4 agonists in murine macrophages: effects of TLR “homotolerance” versus “heterotolerance” on NF-kappa B signaling pathway components. J Immunol 2003;170(1):508–19. [88] Landsman L, Jung S. Lung macrophages serve as obligatory intermediate between blood monocytes and alveolar macrophages. J Immunol 2007;179(6):3488–94. [89] Neish AS, Gewirtz AT, Zeng H, Young AN, Hobert ME, Karmali V, et al. Prokaryotic regulation of epithelial responses by inhibition of IkappaB-alpha ubiquitination. Science 2000;289(5484):1560–3. [90] Lotz M, Gutle D, Walther S, Menard S, Bogdan C, Hornef MW. Postnatal acquisition of endotoxin tolerance in intestinal epithelial cells. J Exp Med 2006;203(4):973–84. [91] Tokairin Y, Shibata Y, Sata M, Abe S, Takabatake N, Igarashi A, et al. Enhanced immediate inflammatory response to Streptococcus pneumoniae in the lungs of mice with pulmonary emphysema. Respirology 2008;13(3):324–32. [92] Wang J, Barke RA, Charboneau R, Schwendener R, Roy S. Morphine induces defects in early response of alveolar macrophages to Streptococcus pneumoniae by modulating TLR9-NF-kappa B signaling. J Immunol 2008;180(5): 3594–600. [93] Droemann D, Goldmann T, Tiedje T, Zabel P, Dalhoff K, Schaaf B. Toll-like receptor 2 expression is decreased on alveolar macrophages in cigarette smokers and COPD patients. Respir Res 2005;6:68. [94] Prescott SL. Effects of early cigarette smoke exposure on early immune development and respiratory disease. Paediatr Respir Rev 2008;9(1):3–9. [95] Bird MD, Kovacs EJ. Organ-specific inflammation following acute ethanol and burn injury. J Leukoc Biol 2008;84(3):607–13. [96] Magnotti LJ, Xu DZ, Lu Q, Deitch EA. Gut-derived mesenteric lymph: a link between burn and lung injury. Arch Surg 1999;134(12):1333–40. [97] Maloney JP. Genetic factors impacting therapy in acute lung injury/acute respiratory distress syndrome. J Investig Med 2008. Published ahead of print, PMID: 18827716. [98] Trammell RA, Toth LA. Genetic susceptibility and resistance to influenza infection and disease in humans and mice. Expert Rev Mol Diagn 2008;8(4): 515–29. [99] Sampath V, Davis K, Senft AP, Richardson TR, Kitzmiller JA, Berclaz PY, et al. Altered postnatal lung development in C3H/HeJ mice. Pediatr Res 2006;60(6):663–8. [100] Selin LK, Brehm MA, Naumov YN, Cornberg M, Kim SK, Clute SC, et al. Memory of mice and men: CD8+ T-cell cross-reactivity and heterologous immunity. Immunol Rev 2006;211:164–81. [101] Kamradt T, Goggel R, Erb KJ. Induction, exacerbation and inhibition of allergic and autoimmune diseases by infection. Trends Immunol 2005;26(5):260–7. [102] Walzl G, Tafuro S, Moss P, Openshaw PJ, Hussell T. Influenza virus lung infection protects from respiratory syncytial virus-induced immunopathology. J Exp Med 2000;192(9):1317–26. [103] Chen HD, Fraire AE, Joris I, Brehm MA, Welsh RM, Selin LK. Memory CD8+ T cells in heterologous antiviral immunity and immunopathology in the lung. Nat Immunol 2001;2(11):1067–76. [104] Chen HD, Fraire AE, Joris I, Welsh RM, Selin LK. Specific history of heterologous virus infections determines anti-viral immunity and immunopathology in the lung. Am J Pathol 2003;163(4):1341–55. [105] Huffnagle GB, Boyd MB, Street NE, Lipscomb MF. IL-5 is required for eosinophil recruitment, crystal deposition, and mononuclear cell recruitment during a pulmonary Cryptococcus neoformans infection in genetically susceptible mice (C57BL/6). J Immunol 1998;160(5):2393–400. [106] Walzl G, Humphreys IR, Marshall BG, Edwards L, Openshaw PJ, Shaw RJ, et al. Prior exposure to live Mycobacterium bovis BCG decreases Cryptococ- Please cite this article in press as: Wissinger E, et al. Immune homeostasis in the respiratory tract and its impact on heterologous infection. Semin Immunol (2009), doi:10.1016/j.smim.2009.01.005 G Model YSMIM-695; No. of Pages 9 ARTICLE IN PRESS E. Wissinger et al. / Seminars in Immunology xxx (2009) xxx–xxx [107] [108] [109] [110] [111] [112] [113] [114] [115] [116] [117] [118] [119] [120] [121] cus neoformans-induced lung eosinophilia in a gamma interferon-dependent manner. Infect Immun 2003;71(6):3384–91. Yoo J, Tcheurekdjian H, Lynch SV, Cabana M, Boushey HA. Microbial manipulation of immune function for asthma prevention: inferences from clinical trials. Proc Am Thorac Soc 2007;4(3):277–82. Edwards L, Williams AE, Krieg AM, Rae AJ, Snelgrove RJ, Hussell T. Stimulation via Toll-like receptor 9 reduces Cryptococcus neoformans-induced pulmonary inflammation in an IL-12-dependent manner. Eur J Immunol 2005;35(1):273–81. Williams AE, Edwards L, Humphreys IR, Snelgrove R, Rae A, Rappuoli R, et al. Innate imprinting by the modified heat-labile toxin of Escherichia coli (LTK63) provides generic protection against lung infectious disease. J Immunol 2004;173(12):7435–43. Tritto E, Muzzi A, Pesce I, Monaci E, Nuti S, Galli G, et al. The acquired immune response to the mucosal adjuvant LTK63 imprints the mouse lung with a protective signature. J Immunol 2007;179(8):5346–57. Williams AE, Edwards L, Hussell T. Colonic bacterial infection abrogates eosinophilic pulmonary disease. J Infect Dis 2006;193(2):223–30. Watkins AC, Caputo FJ, Badami C, Barlos D, Xu dZ, Lu Q, et al. Mesenteric lymph duct ligation attenuates lung injury and neutrophil activation after intraperitoneal injection of endotoxin in rats. J Trauma 2008;64(1):126–30. Cheng AM, Moore EE, Masuno T, Escobar GA, Sarin EL, Johnson JL, et al. Normal mesenteric lymph blunts the pulmonary inflammatory response to endotoxin. J Surg Res 2006;136(2):166–71. Maizels RM. Infections and allergy—helminths, hygiene and host immune regulation. Curr Opin Immunol 2005;17(6):656–61. Furze RC, Hussell T, Selkirk ME. Amelioration of influenza-induced pathology in mice by coinfection with Trichinella spiralis. Infect Immun 2006;74(3):1924–32. Borkow G, Weisman Z, Leng Q, Stein M, Kalinkovich A, Wolday D, et al. Helminths, human immunodeficiency virus and tuberculosis. Scand J Infect Dis 2001;33(8):568–71. Rook GA, Dheda K, Zumla A. Immune systems in developed and developing countries; implications for the design of vaccines that will work where BCG does not. Tuberculosis (Edinb) 2006;86(3–4):152–62. Barton ES, White DW, Cathelyn JS, Brett-McClellan KA, Engle M, Diamond MS, et al. Herpesvirus latency confers symbiotic protection from bacterial infection. Nature (London) 2007;447(7142):326–9. Nguyen Y, McGuffie BA, Anderson VE, Weinberg JB. Gammaherpesvirus modulation of mouse adenovirus type 1 pathogenesis. Virology 2008;380(2):182–90. Goulding J, Snelgrove R, Saldana J, Didierlaurent A, Cavanagh M, Gwyer E, et al. Respiratory infections: do we ever recover? Proc Am Thorac Soc 2007;4(8):618–25. Brundage JF. Interactions between influenza and bacterial respiratory pathogens: implications for pandemic preparedness. Lancet Infect Dis 2006;6(5):303–12. 9 [122] Minino AM, Heron MP, Murphy SL, Kochanek KD. Deaths: final data for 2004. Natl Vital Stat Rep 2007;55(19):1–119. [123] Morens DM, Fauci AS. The 1918 influenza pandemic: insights for the 21st century. J Infect Dis 2007;195(7):1018–28. [124] Louria D, Blumenfeld H, Ellis J, Kilborne ED, Rogers D. Studies on influenza in the pandemic of 1957–58. II. Pulmonary complications of influenza. J Clin Invest 1959;38:213–65. [125] Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community-dwelling elderly. N Engl J Med 2007;357(14):1373–81. [126] McCullers JA. Effect of antiviral treatment on the outcome of secondary bacterial pneumonia after influenza. J Infect Dis 2004;190(3):519–26. [127] McCullers JA, Bartmess KC. Role of neuraminidase in lethal synergism between influenza virus and Streptococcus pneumoniae. J Infect Dis 2003;187(6):1000–9. [128] Lehtinen P, Jartti T, Virkki R, Vuorinen T, Leinonen M, Peltola V, et al. Bacterial coinfections in children with viral wheezing. Eur J Clin Microbiol Infect Dis 2006;25(7):463–9. [129] Resch B, Gusenleitner W, Mueller WD. Risk of concurrent bacterial infection in preterm infants hospitalized due to respiratory syncytial virus infection. Acta Paediatr 2007;96(4):495–8. [130] Thorburn K, Harigopal S, Reddy V, Taylor N, van Saene HK. High incidence of pulmonary bacterial co-infection in children with severe respiratory syncytial virus (RSV) bronchiolitis. Thorax 2006;61(7):611–5. [131] Stark JM, Stark MA, Colasurdo GN, LeVine AM. Decreased bacterial clearance from the lungs of mice following primary respiratory syncytial virus infection. J Med Virol 2006;78(6):829–38. [132] Navarini AA, Recher M, Lang KS, Georgiev P, Meury S, Bergthaler A, et al. Increased susceptibility to bacterial superinfection as a consequence of innate antiviral responses. Proc Natl Acad Sci USA 2006;103(42):15535–9. [133] McAuley JL, Hornung F, Boyd KL, Smith AM, McKeon R, Bennink J, et al. Expression of the 1918 influenza A virus PB1-F2 enhances the pathogenesis of viral and secondary bacterial pneumonia. Cell Host Microbe 2007;2(4):240–9. [134] Sun K, Metzger DW. Inhibition of pulmonary antibacterial defense by interferon-gamma during recovery from influenza infection. Nat Med 2008;14(5):558–64. [135] Bhatia A, Kast RE. How influenza’s neuraminidase promotes virulence and creates localized lung mucosa immunodeficiency. Cell Mol Biol Lett 2007;12(1):111–9. [136] Alonso JM, Guiyoule A, Zarantonelli ML, Ramisse F, Pires R, Antignac A, et al. A model of meningococcal bacteremia after respiratory superinfection in influenza A virus-infected mice. FEMS Microbiol Lett 2003;222(1): 99–106. [137] van der Sluijs KF, Nijhuis M, Levels JH, Florquin S, Mellor AL, Jansen HM, et al. Influenza-induced expression of indoleamine 2,3-dioxygenase enhances interleukin-10 production and bacterial outgrowth during secondary pneumococcal pneumonia. J Infect Dis 2006;193(2):214–22. Please cite this article in press as: Wissinger E, et al. Immune homeostasis in the respiratory tract and its impact on heterologous infection. Semin Immunol (2009), doi:10.1016/j.smim.2009.01.005