* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download GRANULOMATOUS DISEASE & INTERSTITIAL LUNG DISEASE
West Nile fever wikipedia , lookup
Meningococcal disease wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Brucellosis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Trichinosis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Marburg virus disease wikipedia , lookup
Hepatitis C wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Chagas disease wikipedia , lookup
Onchocerciasis wikipedia , lookup
Sarcocystis wikipedia , lookup
Neonatal infection wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Mycobacterium tuberculosis wikipedia , lookup
Hepatitis B wikipedia , lookup
Leptospirosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Fasciolosis wikipedia , lookup
Schistosomiasis wikipedia , lookup
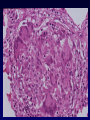
GRANULOMATOUS LUNG DISEASE & INTERSTITIAL LUNG DISEASE GRANULOMATOUS DISEASE Necrotizing vs non-necrotizing • Most necrotizing granulomatous disease is infectious • Responsible organism usually demonstrable in tissue • All specimens should be cultured • Non-infectious granulomatous inflammation – sarcoidosis, Wegener’s granulomatosis & other angiitides TUBERCULOSIS (Robert Koch – 1882) The mycobacteria that cause TB in man: • Mycobacterium Tuberculosis – droplet infection = inhalation of infective droplets coughed or sneezed by a patient with TB • Mycobacterium Bovis – drinking milk from infected cows – intestinal and tonsillar lesions • M. Avium & M. Intracellulare (MAC complex) cause opportunistic infection in IC TUBERCULOSIS • Mycobacteria are Aerobic organisms Difficult to stain - waxy cell wall - scanty in tissue - slow growth in culture - PCR Difficult to kill They have no toxins or histolytic enzymes they inhibit phagosome-lysosome fusion and killing by macrophages they induce delayed hypersensitivity TUBERCULOSIS - Epidemiology • Developed countries – considerable fall in incidence and mortality in 20th century • A disease of the elderly – recrudescence of quiescent infection acquired in youth • Recent resurgence – AIDS, urban deprivation, immigrant & refugee populations TUBERCULOSIS - Epidemiology • 1/3 world population infected (1700 million) • 8 million new cases every year - 95% in developing countries • 3 million deaths every year - largest cause of a death from a single pathogen • TB kills twice as many adults as AIDS, malaria and other parasitic diseases combined • > 80% of TB toll in developing countries is in the economically most productive age-group (15-60 years) TUBERCULOSIS – The impact of HIV infection • Alarming resurgence, poorer communities, drug abuse • Multidrug resistant strains have emerged • 6 million people world-wide have dual infection, majority in sub-Saharan Africa • HIV infection – particularly aggressive TB – widespread dissem. & poor host response • HIV infection promotes infection with opportunistic mycobacteria TUBERCULOSIS Primary TB • First time infection • Formerly found mainly in children, now encountered in adults Postprimary TB • Adult type • Previously sensitized fresh infection or reactivation of a dormant primary lesion PRIMARY TB - Ghon Focus • Inhaled tubercle bacilli ingested by alveolar macrophages • Macrophages with bacilli aggregate, forming microscopic nodules that deform architecture • Development of T-cell mediated immunity CD4 (helper) & CD8 (cytotoxic) • CD4 – interferon – secretory changes in macrophages – epithelioid histiocytes • CD8 – kill macrophages – resulting in caseous necrosis • Fusion of macrophages to form Langerhan’s type giant cells • Mantle of B lymphocytes GHON COMPLEX (1) Parenchymal subpleural lesion at the subpleural fissure between upper and lower lobes & (2) the enlarged hilar / mediastinal caseous lymph nodes draining the parenchymal focus PRIMARY TB – Possible outcomes • Resolution – development of a fibrous capsule - eventually calcified scar • Progression- erosion into bronchus – cavitation – dissemination within bronchial tree (galloping consumption!) • Pleural spread – effusion, TB empyema • Compression by caseous nodes of bronchus or trachea – collapse, compression, stridor • Haematogenous dissemination = Miliary TB cervical lymph nodes (scrofula), meninges (tuberculous meningitis), kidneys, adrenals, bones (tuberculous osteomyelitis) [veterbral TB = Pott’s disease], fallopian tubes, epididymis POSTPRIMARY TB Endogenous vs Exogenous Associations - alcoholism, diabetes, silicosis, immunosuppression Pulmonary Apical disease Caseous pneumonia in lower lobes Cavities – ca, colonization, bronchiectasis Pleural & pulmonary fibrosis Obliterative endarteritis of pulmonary & bronchial aa – but “Rasmussen’s aneurysm” Extrapulmonary complications – amyloid Tuberculosis in the elderly & immunocompromised TB in the elderly Disseminated miliary TB – (non-reactive TB) little granulomatous response, necrosis, DAD TB in AIDS 1. conventional morphology 2. granulomas poorly formed 3. opportunistic MAC from environment, spindle cell pseudotumours TB – Skin tests & vaccinations • Old tuberculin – now purified protein derivative (ppd) • Intradermal injection – Mantoux • Multi-pronged devices – Heaf test • Positive reaction indicates that a person has been infected by tubercle bacillus • Prophyllactic immunization with strain of low virulence – Bacillus Calmette Guerin (BCG) Necrotizing Granulomas other infectious causes • Brucellosis • Fungi – Histoplasma, Coccidioides Cryptococcus, Blastomyces • Dirofilaria SARCOIDOSIS • A disease of unknown cause characterized by noncaseating granulomas in many tissues & organs • Lungs, lymph nodes, spleen, liver, bone marrow, skin, eye, salivary glands and less frequently – heart, kidneys, CNS, endocrine glands – pituitary • Occurs worldwide, more prevalent at higher latitudes – Scandinavia, northern Europe and North America • B>W, F>M, but rare in American Indians, Eskimos • Communicable agent suspected but as yet undiscovered SARCOIDOSIS • Enhanced cellular hypersensitivity at involved sites – but depressed elsewhere • Increased CD4 lymphocytes in the lung • Clinical: mild non-specific chest complaints, cough, dyspnoea 1/3 – Erythema nodosum Increased serum Ca, ACE, gammaglobulins • Radiographic Staging: I Hilar adenopathy alone (best) II Hilar adenopathy & parenchymal infiltrates III Parenchymal infiltrates alone (worst) SARCOIDOSIS in the lung Non-caseating granulomas • Tight clusters of epithelioid histiocytes and occassional MNGCs • Tight rim of concentric fibroblasts , scattered lymphocytes (naked granulomas) • Laminated concretions – Schaumann Bodies • Stellate inclusions – Asteroid Bodies Distribution – along lymphatics (TBBx) • Granulomatous vasculitis DDx – infection, berylliosis, HP, IVDA, adjacent to tumour / lymphoma INTERSTITIAL LUNG DISEASE • A heterogeneous group of non-neoplastic disorders resulting from damage to the lung parenchyma by varying patterns of inflammation and fibrosis • Interstitium (space between the epithelial and endothelial BM) - primary site of injury • These disorders frequently also affect the airspaces, airways and vessels • Clinical – Radiology – Pathology correlation NB • Aetiology / associations: idiopathic, collagen vascular disease, drugs & toxins, environmental INTERSTITIAL LUNG DISEASE • Usual interstitial pneumonia (UIP) aka Cryptogenic fibrosing alveolitis (CFA) aka Idiopathic pulmonary fibrosis (IPF) Vs. The others: Non-specific interstitial pneumonia (NSIP) Organizing pneumonia (OP) Respiratory bronchiolitis (RB) Desquamative interstitial pneumonitis (DIP) Lymphocytic interstitial pneumonitis (LIP) Usual Interstitial Pneumonia • Patchy lung involvement – worst at bases, subpleural & paraseptal distribution • Dense fibrosis – remodelling of lung architecture – “honeycombing” • Fibroblast foci • Gradual onset of symptoms: dyspnea, non-prod cough • Median survival 2.5 – 3.5 years