* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Immune defence in the lymphatic system of the skin
Survey
Document related concepts
Complement system wikipedia , lookup
DNA vaccination wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Molecular mimicry wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Adaptive immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Transcript
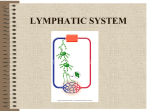
118 Review Article Immune defence in the lymphatic system of the skin K. Schmolke Dept. for lab. medicine (DRK-Kliniken), Berlin, Germany Keywords Schlüsselwörter Epidermis, Langerhans dendritic cells, lymphatic system, antigen-presenting cell Epidermis, Langerhans-Dendriten, Lymphbahn, antigenpräsentierende Zelle Summary Zusammenfassung As the interface organ between the body and the external environment, the skin is predestined to have frequent and intensive contact with pathogens and therefore possesses a particularly well-developed immunological defence. The immune system protects the body’s integrity with innate components such as the skin’s physicochemical barrier function, the phagocytic cells and the complement system. The network of Langerhans dendritic cells in the epidermis allows immediate detection and rapid transport of antigen material to the regional lymph nodes and the triggering of a specific immune response by T and B cells. For immunological processes, the passage through the lymphatic system is decisive, as diverse interactions occur between cells and the lymphatic system. On the one hand, the interaction of dendritic receptors with antigenic structures triggers intracellular signals, allowing migration through the lymphatic system to the lymph node via chemokines and chemokine receptors. On the other hand, the Langerhans dendritic cells alter their own phenotype during migration through the lymphatic system: they lose their ability to phagocytise in favour of the increased synthesis of MHC molecules and become antigen-presenting cells. Als Grenzorgan zwischen Außen und Innen ist die Haut prädestiniert für häufigen und intensiven Kontakt mit Pathogenen und ist daher immunologisch besonders gerüstet. Das Immunsystem schützt die Integrität des Organismus mit angeborenen Komponenten wie der physikalisch-chemischen Barrierefunktion der Haut, den Phagozytosezellen und dem Komplementsystem. Das Netzwerk der Langerhans-Dendriten in der Epidermis ermöglicht sofortiges Aufspüren und zügigen Transport von Antigenmaterial in den regionären Lymphknoten und Auslösung einer spezifischen Immunantwort durch T- und B-Zellen. Für immunologische Vorgänge ist die Passage durch die Lymphbahnen entscheidend, da Zellen und Lymphbahnen vielfältig wechselwirken. Einerseits werden durch die Interaktion von dendritischen Rezeptoren mit antigenen Strukturen intrazelluläre Signale getriggert, die die Wanderung durch die Lymphbahn zum Lymphknoten über Chemokine und Chemokinrezeptoren ermöglichen. Die Langerhans-Dendriten andererseits verändern sich auch selbst phänotypisch während der Wanderung durch die Lymphbahnen: sie verlieren die Phagozytosefähigkeit zugunsten der verstärkten Synthese von MHC-Molekülen und werden zu antigenpräsentierenden Zellen. Correspondence to Dr. med. Kathrin Schmolke Oberärztin der zentralen Abteilung für Labormedizin DRK-Kliniken Berlin, Standort Westend Spandauer Damm 130, D-14050 Berlin, Germany E-mail: [email protected] Immunabwehr im Lymphsystem der Haut Phlebologie 2015; 44: 118–120 DOI: http://dx.doi.org/10.12687/phleb2262-3-2015 Received: March 18, 2015 Accepted: March 19, 2015 Lymphatic system The lymphatic system regulates tissue pressure through the return flow of interstitial fluid into the blood. This fluid, the lymph, is returned to the venous system via the venous angles. In addition to its homoeostatic function in fluid balance, the lymphatic system also performs transport functions in the upper gastrointestinal region for high-molecular, hydrophobic chylomicrons from the digestive tract. The lymphatics are also used by another system for transporting its components: the immune system. Immune cells migrate via the lymphatic vessels from the periphery into the regional lymph nodes. En route to the lymphatic organs, lymphatic vessels and immune cells interact with each other in a variety of ways. Functions of the immune system The function of the immune system is to defend the body against infectious pathogens and to monitor the tissue integrity of the body as a whole. An essential precondition for this is the ability to distinguish between the body’s own components (“self ” = harmless) and non-self components (“foreign” = potentially dangerous). This is enabled via the expression of MHC molecules (MHC – major histocompatibility complex) on the cell surface of nucleated cells, which present cellular peptides externally, thus signalling an intact self to the immune system: they are not attacked. Apoptotic cells and tumour cells are on the border between self and foreign: As originally endogenous cells that have undergone mutagenic changes, tumour cells can potentially present mutagenically altered peptides via their surface MHC, © Schattauer 2015 Phlebologie 3/2015 Downloaded from www.phlebologieonline.de on 2017-06-16 | IP: 88.99.165.207 For personal or educational use only. No other uses without permission. All rights reserved. 119 K. Schmolke: Immune defence in the lymphatic system of the skin Immune System Differentiation Tolerance Self Foreign Self Altered self Intact cell Dead cell Tumour cell Elimination Foreign Pathogen Foreign body Transplant Fig. 1 The task of the immune system is to maintain the integrity of the whole body and all its cells. This requires the ability to distinguish between the body’s own structures (self) and non-self structures (foreign). The immune system must tolerate the body’s own structures and recognise (and eliminate) foreign structures. thus revealing themselves to the immune system. Tumour cells accordingly downregulate MHC on their cell surface (1). This is a specific mechanism, to avoid destruction by the immune system (immune escape). Apoptotic cells, on the other hand, lose MHC during the membrane degradation of induced cell death. Apoptosis is a targeted process and does not trigger any concerted inflammatory reaction (2). The immune system is not alerted, as the cells die according to a plan, disintegrating from the inside, and cell residues are phagocytised. Pathogens, on the other hand, express completely different molecular structures on their surfaces compared with body cells. They are thus clearly recognisable to the immune system and trigger an immune reaction. The picture is similar for allogeneic transplants; although they possess human MHC, it is that of another individual. Both are identified as foreign and are attacked by the immune system (▶Fig. 1). The cellular and particulate components of the immune system are subdivided into innate and adaptive. The innate part reacts rapidly, uniformly and unchangingly to a wide variety of stimuli (non-specific reaction). The carriers of the non-specific immunity are widely disseminated in the body and react conservatively and ubiquitously (“the more the merrier”). In addition to the physicochemical barriers, the innate immune system also includes the phagocytes and the complement system. The adaptive part reacts with a temporal delay and requires highly differentiated stimuli, which are recognised via specialised receptors (specific reaction). The cells of the specific immunity, however, can adapt and remember and they differ from each other. On initial contact with a pathogen, only a few T and B cells react; on second contact, many cells react rapidly and with highly avid receptors. Immunity of the skin As it forms an interface organ, the skin is predestined to have particularly frequent and intensive contact with pathogens. Al- Fig. 2 The lymphatic vessels of the skin form a horizontal, polygonal capillary network below the epidermis. They do not contain smooth-muscle cells but are attached to the surrounding matrix through anchoring filaments. Murine epidermis after fluorescence lymphangiography; © with the kind permission of G. Randolph; reproduced with the permission of Macmillan Publishers Ltd: Nature Reviews Immunology (Randolph et al. 2005) though the epidermis itself is one of the few lymph-free body tissues (3, 4), the borderline between the body and the external environment has a particularly well-developed immunological defence. If pathogens succeed in overcoming the physicochemical barriers, the innate immune defence is initially activated. Controlled by chemokines, neutrophils migrate from the vessels into the tissue, where they phagocytise at the site of the primary reaction. Complement components are activated by binding of C3b to bacterial lipopolysaccharide (LPS) and precipitate a cascade, leading to the formation of pore complexes that destroy the bacterial cell wall. Individual complement components additionally exert an opsonising effect (i.e. marking for phagocytosis). Repetitive molecular surface structures, such as the LPS of the Gramnegative bacterial cell wall, are identified by tissue macrophages via specific receptors. As these structures, which have become highly conserved through evolution, are not expressed on human cells, they allow the macrophages rapid and reliable identification of the invading pathogens. The network of the Langerhans dendritic cells in the skin triggers transfer of the pathogenic structures to the specific immune system. Langerhans cells are dendritic cells of the monocytic line, which branch out between the epidermal cells using their elongated cellular processes. They continuously phagocytise extracellular material in their surroundings. After absorbing pathogenic material, they migrate via the dermal lymphatic system to the nearest locoregional lymph node (5, 6). During their migration through the lymphatic system, the Langerhans dendritic cells undergo phenotypical and functional changes and mature to their actual function as antigen-presenting cells (APC). They lose their ability to phagocytise in favour of greater synthesis of MHC molecules. Via MHC, they present antigenic peptides to T cells in the nodular T-cell regions. If a naive or memory T cell with its T-cell receptor fits exactly to the antigenic peptide presented, this results in the formation of an immunological synapse, leading to the initiation of a specific immune response (7) with destruction of the antigen. Phlebologie 3/2015 © Schattauer 2015 Downloaded from www.phlebologieonline.de on 2017-06-16 | IP: 88.99.165.207 For personal or educational use only. No other uses without permission. All rights reserved. K. Schmolke: Immune defence in the lymphatic system of the skin The functions of the lymphatic system of the skin As a transport network, the lymphatic system forms part of the immune system. It forms a network in the skin that lies parallel to the avascular epidermis in the cutis (▶Fig. 2). Lymph flow is unidirectional from the periphery to the centre and is secured by means of valvular structures. The confluence of the thoracic duct and the vena cava in the venous angle unites the lymph and blood flow. As T cells can circulate between the blood and the lymph and dendritic cells from the periphery migrate to the lymph nodes, the likelihood of them meeting in the lymph node is particularly high (▶Fig. 3). The dendritic cells form an interface between the innate and the specific immune system and process a broad spectrum of antigens from dermatological pathogens. Immature dendrites in the surface epithelia phagocytise antigens similar to macrophages. They can absorb extracellular material (e.g. from bacteria, fungi and parasites) or are directly infected by viruses and absorb intracellular viral proteins. The interaction of dendritic receptors with antigenic structures triggers intracellular signals, allowing migration through the lymphatic system to the lymph node via chemokines and chemokine receptors. The interplay of CCR7 (chemokine receptor type 7) on the dendrites and the corresponding ligands CCL19 (chemokine ligand 19) in the lymphatic system appears to allow migration to the lymph node along a directional gradient (8). CCL19-deficient mice show a marked defect in dendritic cell migration to the lymph nodes (9, 10). Concurrently, more MHC is expressed, leading to an increased antigen presentation, further reinforced by inflammatory mediators (leukotrienes, prostaglandins). During its passage through the lymphatic system, therefore, the Langerhans dendritic Tissue cell Interstitium Lymphocapillary vessel Fig. 3 T cells migrate back and forth between the blood and lymphatic system. (Image source: National Cancer Institute website http://www.cancer.gov) Tissue fluid Arterioles cell changes from a sedentary phagocyte into a migratory cell, which effectively presents its absorbed antigen load to the corresponding immune cell partner at the correct location. In skin sections experimentally separated from the lymph, no specific immune response can be precipitated, despite the fact that the blood flow continues to function without interruption (7), as T cells can never be sensitised to antigenic material directly in the tissue. Passage of the epidermal dendrites through the lymphatic system is essential in order to trigger an adaptive immune response. Moreover, a destroyed lymphatic system can no longer perform this task. Risk factors are infections, particularly by staphylococci and streptococci (erysipelas), but also parasitic disease, trauma, irradiation or chemotherapy drugs. This leads to oedema with atrophy of the lymph nodes above areas of prolonged stagnation (11). Treatment approaches such as the manual lymphatic drainage restore the dendritic cell transport by reactivating the lymph flow. This promotes the antigen presentation in the lymph node and therefore the innitiation of an immune response. Venule Lymphatic system Literatur 1. Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity 2004; 137–148. 2. Bossi G et al. The secretory synapse: the secrets of a serial killer. Immunol Rev 2002; 189:152–160. 3. Mumprecht V, Detmar M. Lymphangiogenesis and cancer metastasis. J Cell Mol Med 2009; 1405–1416. 4. Cueni LN, Detmar M. The lymphatic system in health and disease. Lymphat Res Biol 2008; 6: 109–122. 5. Randolph GJ, Angeli V, Swartz MA. Dendritic-cell trafficking to lymph nodes through lymphatic vessels. Nature Immunology 2005; 5: 617–628. 6. Mártin-Fontecha A et al. Regulation of Dendritic Cell Migration to the Draining Lymph Node: Impact on T Lymphocyte Traffic and Priming. J Exp Med 2003; 198(4): 615–621. 7. Murphy KP, Walport M. Janeway Immunology. Spektrum Verlag Heidelberg 2009. 8. Förster R et al. CCR7 coordinates the primary immune response by establishing functional microenvironments in secondary lymphoid organs. Cell 1999; 99: 23–33. 9. Gunn MD et al. Mice lacking expression of secondary lymphoid organ chemokine have defects in lymphocyte homing and dendritic cell localization. J Exp Med 1999; 189: 451–460. 10. Luther SA et al. Coexpression of the chemokines ELC and SLC by T zone stromal cells and deletion of the ELC gene in the plt/plt mouse. Proc Natl Acad Sci 2000; 97: 12694–12699. 11. Olszewski WL et al. Topography of Accumulation of Stagnant Lymph and Tissue Fluid in Soft Tissues of Human Lymphedematous Lower Limbs. Lymphat Res Biol 2009; 4: 239–245. © Schattauer 2015 Phlebologie 3/2015 Downloaded from www.phlebologieonline.de on 2017-06-16 | IP: 88.99.165.207 For personal or educational use only. No other uses without permission. All rights reserved. 120