* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Protein synthesis and metabolism
Protein–protein interaction wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Western blot wikipedia , lookup
Butyric acid wikipedia , lookup
Two-hybrid screening wikipedia , lookup
Point mutation wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Phosphorylation wikipedia , lookup
Peptide synthesis wikipedia , lookup
Metalloprotein wikipedia , lookup
Protein structure prediction wikipedia , lookup
Genetic code wikipedia , lookup
Citric acid cycle wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Proteolysis wikipedia , lookup
Biosynthesis wikipedia , lookup
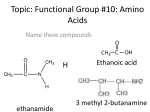
Amino acid synthesis wikipedia , lookup
Liver Functions Harry and Jaz Protein synthesis and metabolism Protein synthesis • Plasma proteins • Clotting factors • Complement factors Protein synthesis • Plasma proteins • Clotting factors • Complement factors Protein synthesis – plasma proteins • Main types: • Albumin • Globulin • Fibrinogen Protein synthesis – plasma proteins • Main types: • Albumin • Globulin • Fibrinogen Protein synthesis – albumin • Most common plasma protein • Functions • Maintenance of colloid osmotic pressure • Binding and transport of large, hydrophobic compounds • Bilirubin, fatty acids, hormones, drugs • Antioxidant (traps free radicals) • Anticoagulant and antithrombotic effects Protein synthesis – albumin • Most common plasma protein • Functions • Maintenance of colloid osmotic pressure • Binding and transport of large, hydrophobic compounds • Bilirubin, fatty acids, hormones, drugs • Antioxidant (traps free radicals) • Anticoagulant and antithrombotic effects Starling forces • Opposing forces act to move fluid across the capillary wall • Net filtration pressure depends upon sum of four variables: Capillary hydrostatic pressure Interstitial hydrostatic pressure Capillary oncotic pressure Interstitial oncotic pressure Interstitial fluid Capillary Capillary oncotic pressure • The pores of capillaries are impermeable to plasma proteins • very low conc. of plasma proteins in interstitial fluid • Higher conc. of plasma proteins in plasma • lower relative water conc. in plasma vs. that in interstitial fluid • net movement of water out of interstitial fluid and into plasma Capillary oncotic pressure – when it goes wrong… • The liver produces albumin… • Liver failure dysfunction in albumin production • Decreased production less albumin in blood (hypoalbuminaemia) • Albumin contributes to capillary oncotic pressure... • Hypoalbuminaemia dec. capillary oncotic pressure • less of a difference in water conc. between plasma and interstitial fluid • accumulation of water in interstitial fluid (oedema) Hypoalbuminaemia oedema Protein synthesis – plasma proteins • Main types: • Albumin • Globulin • Fibrinogen Protein synthesis - globulins • Functions • Antibody functions (most are gamma-globulins – not made by liver) • Blood transport of: • Lipids • Iron • Copper (by lipoproteins) (by transferrin) (by caeruloplasmin) Protein synthesis • Plasma proteins • Clotting factors • Complement factors The liver and clotting • Production of clotting factors • All, except: • Calcium (IV) • von Willebrand factor (VIII) • Production of bile salts • Necessary for intestinal absorption of vitamin K • Vitamin K is required to produce numerous clotting factors Protein synthesis • Plasma proteins • Clotting factors • Complement factors Protein synthesis – complement factors • Function • Important part of the immune response to pathogens Protein metabolism – turnover and degradation • Continuous degradation and re-synthesis of all cellular proteins • 70-80% of liberated amino acids are re-utilised into proteins • Variable rate – reflecting usage and demand • Increase seen in: • Damaged tissue due to trauma • Skeletal tissue during starvation – gluconeogenesis • 2 primary methods: • Lysosomal pathway • Ubiquitin-proteosome pathway Amino acid breakdown • Surplus of amino acids • Degradation • Amino acid catabolism R • Requires removal of alpha-amino group • Produces: • Nitrogen • Incorporated into other compounds • Excreted • Carbon skeleton • Metabolised • Majority released as ammonia • 2 processes: • Transamination • Oxidative deamination +H N 3 CH COO- Amino acid breakdown • Surplus of amino acids • Degradation • Amino acid catabolism R • Requires removal of alpha-amino group • Produces: • Nitrogen • Incorporated into other compounds • Excreted • Carbon skeleton • Metabolised • Majority released as ammonia • 2 processes: • Transamination • Oxidative deamination +H N 3 CH COO- Amino acid breakdown - transamination • Transfer of alpha-amino group from amino acid to alpha-ketoglutarate • Formation • An alpha-keto acid (e.g. pyruvate) – Krebs’ • Glutamate • Oxidative deamination • Amino group donor (synthesis of non-essential amino acids) • Catalyst • Aminotransferase enzymes • Readily reversible process • Amino acid degradation (after protein-rich meal) • Amino acid synthesis (dietary supply cellular demand) Amino acid breakdown - transamination +H N 3 R R aminotransferase -OOC – CO – C – C – COO- Alpha-ketoglutarate + +H N 3 CH L-amino acid COO- -OOC – C – C – C – COO- L-glutamate + CO COO- Alpha-keto acid Amino acid breakdown • Surplus of amino acids • Degradation • Amino acid catabolism R • Requires removal of alpha-amino group • Produces: • Nitrogen • Incorporated into other compounds • Excreted • Carbon skeleton • Metabolised • Majority released as ammonia • 2 processes: • Transamination • Oxidative deamination +H N 3 CH COO- Amino acid breakdown – oxidative deamination • Results in the liberation of amino group as free ammonia • Formation • An alpha-keto acid (e.g. pyruvate) • Ammonia Krebs’ Urea cycle • Catalyst • Glutamate dehydrogenase • Co-enzymes (NAD+/NADPH) • Readily reversible process • Dependent upon relative concentrations of: • Glutamate, alpha-ketoglutarate, ammonia • After protein rich-meal, glutamate concentration is high • Reaction degrades amino acid glutamate ammonia formation Nitrogen balance A measure of the equilibrium of protein turnover; • Anabolic – positive balance • Catabolic – negative balance Daily nitrogen intake 0.8g/Kg body weight 1.3g/Kg body weight 2.4g/Kg body weight Glucose/Alanine Cycle Glucose/Alanine Cycle Input of amine groups (NH2) comes from; • Dietary amino acids (9 cannot be synthesized by the human body) • Alanine and glutamine from muscles Glucose/Alanine Cycle Excess amino acids are metabolised. They are not stored for use as potential energy as this can be done more efficiently by other sources. α-keto acid Fed into the Krebs cycle to be incorporated into glucose production Ammonia Mainly excreted, although some is used in the biosynthesis of amine containing substances e.g. amino acids, nucleotides Urea Cycle Enzymes responsible are found in mitochondria and cytosol. Urea Cycle One turn of the cycle consumes; • 3 ATP equivalents • 4 high energy nucleotides Deficiencies in any of the enzymes involved is associated with higher levels of ammonia in the blood. - absence of the enzymes is not compatible with life High levels of ammonia (neurotoxicity) Increased ammonia crosses the BBB readily; • Converted to glutamate (glutamate dehydrogenase) • Decrease in α-ketoglutarate in brain • Decrease in oxaloacetate • Krebs cycle stops This leads to irreparable cell damage and neural cell death Glucose regulation Absorptive and post-absorptive state • Absorptive state • Ingested nutrients are absorbed from the GI tract into the blood • A proportion of nutrients are catabolised and used • The remainder are converted and stored for future use • Post-absorptive state • Nutrients are no longer absorbed from the GI tract • Nutrient stores must supply the energy requirements of the body Glucose regulation – post-absorptive state • Glucose is no longer being absorbed from the GI tract *Note • Essential to maintain the plasma glucose concentration Enzyme required to form glucose from glucose 6phosphate formed in glycogenolysis is not present in skeletal muscle • Almost always fuels the CNS (except in prolonged starvation) • Sources of blood glucose • Glycogenolysis (hrs) • Hydrolysis of glycogen stores in liver (and skeletal muscle*) • Lipolysis • Glycerol released is enzymatically converted to glucose in the liver • Proteolysis (>hrs) Instead, glucose 6-phosphate formed in muscle undergoes glycolysis, yielding: • • • ATP Pyruvate Lactate Lactate is taken up by the liver and converted to glucose • Amino acids taken up by the liver and converted to glucose • Synthesis of glucose from above precursors (glycerol, amino acids) = gluconeogenesis Gluconeogenesis • The process of generating new molecules of glucose from noncarbohydrate precursors • Substrates • Pyruvate = major substrate • Formed from lactate and other amino acids • Glycerol (formed through triglyceride hydrolysis) • 6 ATP molecules are consumed per molecule of glucose formed Storage Liver storage • Iron • Fat soluble vitamins • Glycogen • Minerals Liver storage • Iron • Fat soluble vitamins • Glycogen • Minerals Iron • Distribution • Utilised by: • Haemoglobin • Myoglobin • Bone marrow • Stored in: • Liver • Reticulo-endothelial macrophages Duodenum Primary location of iron absorption • Absorption • Transferrin • Transports iron in the plasma to the bone marrow – iron incorporated into new RBC • Ferritin • Storage form of iron • Main source is found in the liver Liver storage • Iron • Fat soluble vitamins • Glycogen • Minerals Fat soluble vitamins - ADEK •A • Stored in Ito cells (in space of Disse) • High levels stored in liver – prevent deficiency for 10 months • Function • Vision (retinal pigments) • Healthy skin • Growth and reproduction •D • Liver storage prevents deficiency for 3-4 months • Function • Increases calcium reabsorption from intestinal tract • Promotes intestinal phosphate reabsorption Fat soluble vitamins - ADEK •E • Function • Antioxidant •K • Function • Necessary for production of clotting factors • B12 • Liver stores prevent deficiency for >1yr • Function • Promotes growth and RBC formation + maturation • Intrinsic factor • Produced by parietal cells of stomach • Required for absorption of B12 – deficiency pernicious anaemia B12 is absorbed in the terminal ileum Liver storage • Iron • Fat soluble vitamins • Glycogen • Minerals Glycogen • Sites of storage • Liver (~10% mass of liver) • Skeletal muscle (~2% mass of skeletal muscle) • Function • Readily mobilised storage form of glucose • Maintain blood glucose levels Overall storage is larger in skeletal muscle as its mass is far greater Glycogen is the secondary energy reservoir – with lipids being the primary source Liver storage • Iron • Fat soluble vitamins • Glycogen • Minerals Minerals • Iron • Stored as ferritin • Copper Fat metabolism Body Energy Reserve Number of kcal Length of effect Blood glucose 40 A few minutes Glycogen 600 Day Muscle 25,000 7-10 days Lipid reserve 100,000 30-40 days Most of the body’s fat is stored in adipocytes which form tissues called adipose tissue. Some is stored in hepatocytes. Triglycerides Triglycerides (TGs, TAGs) consist of 3 fatty acids bound to a glycerol molecule. It accounts for 78% of energy stored in body – proteins (21%) and carbohydrates (1%). Lipoproteins HDL – formed in the liver LDL – formed in plasma VLDL – synthesized in hepatocytes Also IDL. They are used to transport cholesterol through the blood. Lipids Lipids are esters of fatty acids and certain alcohol compounds. They have several functions; • Energy reserves • Structural – part of cell membrane • Hormone metabolism Digestion and absorption 1. Bile salts and phospholipids emulsify dietary fats in the small intestine forming mixed micelles 2. Intestinal lipases degrade TGs 3. Fatty acids and other breakdown products are taken up into intestinal mucosa and converted into triacyglycerols 4. Triacyglycerols are incorporated with cholesterol and apolipoproyeins into chylomicrons 5. Chylomicrons move through the lymphatic system and bloodstream into the tissues 6. Lipoprotein lipase converts triacyglycerols to fatty acids and glycerol 7. Fatty acids enter cells 8. Fatty acids are oxidised as fuel or re-esterified for storage Fat Catabolism – breaking down into smaller units 1. Molecule of coenzyme A links to carboxyl at the end of a fatty acid 2. Breakdown of ATP > AMP + 2Pi 3. Coenzyme A derivative of fatty acid proceeds through beta-oxidation reactions 4. Molecule of acetyl coenzyme A is split off from fatty acid and 2H+ transferred to coenzymes 5. Hydrogen atoms from coenzymes enter the oxidative phosphorylation pathway to form ATP 6. Another coenzyme A attaches to fatty acid and the cycle is repeated 7. Coenzyme – 2H molecules lead to the production of CO2 and ATP via the Krebs cycle and oxidative phosphorylation Hepatic metabolism of lipids Lipoprotein lipase - Hydrolyses TGs in lipoproteins (chylomicrons, VLDLs) into 2 free fatty acids and 1 glycerol molecule Hepatic lipase - Expressed in the liver and adrenal glands, it converts IDL into LDL LIVER FUNCTIONS DONE!