* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download DNA copy number analysis by MAPH: molecular diagnostic
Promoter (genetics) wikipedia , lookup
Gene expression profiling wikipedia , lookup
Exome sequencing wikipedia , lookup
Molecular cloning wikipedia , lookup
Gel electrophoresis wikipedia , lookup
Genomic imprinting wikipedia , lookup
X-inactivation wikipedia , lookup
Silencer (genetics) wikipedia , lookup
Cre-Lox recombination wikipedia , lookup
Agarose gel electrophoresis wikipedia , lookup
Deoxyribozyme wikipedia , lookup
Gel electrophoresis of nucleic acids wikipedia , lookup
Genome evolution wikipedia , lookup
Non-coding DNA wikipedia , lookup
Bisulfite sequencing wikipedia , lookup
Copy-number variation wikipedia , lookup
Point mutation wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Molecular evolution wikipedia , lookup
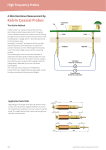
Technology Report DNA copy number analysis by MAPH: molecular diagnostic applications Edward J Hollox, Seyed M Akrami and John AL Armour† CONTENTS How MAPH works Applications of MAPH Translating MAPH from a research to a diagnostic tool DNA copy number variation is an important cause of genetic disease. There are several techniques available to detect copy number changes of various sizes, each with their limitations in resolution and cost. Here we outline the development of multiplex amplifiable probe hybridization (MAPH) into a high-throughput diagnostic technique for detecting copy number variation of almost any size. Its application in testing for genetic mutations causing diseases, such as familial breast cancer, Charcot-Marie-Tooth disease Type 1A, Duchenne/Becker muscular dystrophy and familial colorectal cancer is described, as well as its use in identifying chromosomal changes in some individuals with mental retardation. The analysis of the data produced by MAPH is also considered, along with its potential for automation and development of microarray-based MAPH. Expert Rev. Mol. Diagn. 2(4), (2002) Expert opinion Five-year view KEYWORDS breast cancer, deletion, DNA copy number, DNA microarray, Duchenne muscular dystrophy, fluorescence in situ hybridization, hybridization, subtelomeric DNA Multiplex amplifiable probe hybridization (MAPH) is a method that measures copy number (also described as dosage) in genomic DNA [1]. In humans, every somatic cell has two copies of most genes or other loci, one copy from its mother and one copy from its father. One of the most familiar examples is when one copy of chromosome 21 is inherited from one parent and two copies from the other parent; the result is trisomy 21 and consequently Down syndrome. Trisomy is copy number variation of the human genome at a very large scale (i.e., a whole chromosome) but copy number changes involving small sections of chromosomes, individual genes and even single exons can cause genetic disease. Deletion and complex rearrangements of sections of subtelomeric DNA are associated with mental retardation or other multiple congenital abnormalities [2,3]. These changes may cause the phenotype by altering the gene copy in copy number in that section. As far as is known, the subtelomeric DNA of any chromosome end can be involved in such changes and as these regions are densely packed with genes. The specific gene or genes that are responsible for the clinical phenotypes have not yet been identified. Studies using fluorescent in situ hybridization (FISH) on cohorts of patients with mental retardation suggest that at least 6% have subtelomeric deletions or rearrangements [4]. Whether any of the remaining 94% have smaller changes that cannot be detected by FISH is not known. Rearrangements within chromosomes can cause genetic disease and can be mediated by large low copy number chromosomal repeat elements, or duplicons [5]. For example, Charcot-Marie-Tooth disease Type 1A (CMT1A) is caused by duplication of a 1.4 Mb genomic region containing the PMP22 gene and hereditary neuropathy with liability to pressure palsies (HNPP) is caused by heterozygous deletion of the same region [6]. Pelizaeus-Merzbacher disease is caused by duplication of the PLP1 gene [7] and Williams syndrome, in 95% of cases, by a 1.6 Mb deletion of chromosome 7q11.23 [8]. Copy number changes of one or more exons within specific genes can also cause genetic disease, as an alternative to point mutations creating single amino acid changes or a premature stop codon. A duplication or deletion of an exon can either create a premature stop codon, if the deletion changes the reading frame of the www.future-drugs.com © Future Drugs Ltd. All rights reserved. ISSN 1473-7159 89 Key issues References Affiliations †Author for correspondence, Institute of Genetics, Queen’s Medical Centre, University of Nottingham, NG7 2UH, UK Tel.: +44 115 970 9398 Fax: +44 115 970 9906 [email protected] Hollox, Akrami & Armour mRNA, or can create a misfolded or otherwise nonfunctional protein, if the deletion does not change the reading frame of the mRNA. This can happen to any gene but genes that are large or have introns rich in repeat elements are especially prone to this type of mutation. For example, 65% of mutations at the large DMD gene (causing Duchenne/Becker muscular dystrophy) are deletions or duplications involving one or more exons [9], and one report testing a Dutch cohort of women suggests that 35% of BRCA1 mutations are deletions or duplications of one or more exons [10]. It is clear that copy number variation is an important cause of genetic disease. However, smaller changes within genes are often missed by conventional mutation detection techniques and larger changes, involving several genes, are either prohibitively slow or prohibitively expensive to test for on a medium to large scale. MAPH has many different advantages over the variety of different methods to detect copy number changes (TABLE 1) and because of its low cost, high multiplicity and flexible resolution, can be regarded as a unifying technology applicable for detecting any copy number change from 100 nucleotides of DNA through to entire chromosomes. How MAPH works MAPH relies on the fact that probes can be quantitatively recovered and amplified after hybridization. A diagram of the experimental procedure is shown in FIGURE 1. The full experimental details have been published [1] with regular updates and practical notes at our laboratory’s website [101]. Briefly, genomic DNA is denatured and attached to a small piece of nylon membrane. Amplifiable probes, corresponding to the loci to be assayed for copy number, are then hybridized in excess to this genomic DNA. Since the probes are in excess, every site that is recognized by the probes in the genomic DNA is occupied, so the amount of bound probe depends on the number of available sites for that probe in the genomic Table 1. Comparison of MAPH with other methods of DNA copy number analysis. Resolution Resolution limited by Starting material Loci per test Major equipment needed PCR across rearranged 2 bp-5 kb region, followed by gel electrophoresis Gel resolution, enzyme extension ability, DNA quality Genomic DNA solution <6 None Real-time PCR >50 bp Amplicon size and spacing Genomic DNA solution <6 Real-time PCR machine Quantitative multiplex PCR >50 bp Amplicon size and spacing Genomic DNA solution <6 Fluorescent gel/ capillary sequencer G-band cytogenetics >2 Mb Chromosome preparation Metaphase chromosomes <1500 Microscope CGH >10 Mb Chromosome preparation Metaphase chromosomes <300 Fluorescence Microscope Array-CGH >30 kb Clone size and spacing Genomic DNA solution ~2400 Fluorescence Microscope Metaphase-FISH >30 kb§ Chromosome preparation Metaphase chromosomes 2-3 Fluorescence Microscope Interphase-FISH >30 kb Microscope resolution/ clone spacing Cells 2-3 Fluorescence Microscope Strand-FISH >10 kb Microscope resolution/ clone spacing Genomic DNA in agarose blocks <6 Fluorescence Microscope Southern Blot 1 kb-2 Mb Restriction fragment length/gel resolution Genomic DNA solution (in agarose blocks for pulse-field gel electrophoresis) 1-2 Phosphoimager if quantitative Genomic DNA solution Up to 61§§ MAPH >100 bp Probe size and spacing None if qualitative Fluorescent gel/ capillary sequencer § The resolution of metaphase FISH depends on the experiment. If a presence/absence of a signal is used to detect copy number change, then the resolution is the same as the size of the probe (usually derived from 30 kb cosmid or 100 kb BAC/PAC). If detecting copy number changes by the distance between two probes, then the resolution of metaphase-FISH is similar to G-band cytogenetics (>2 Mb). §§ The maximum number of loci tested simultaneously in work to date so far is 61, but the upper limit is not known. 90 Expert Rev. Mol. Diagn. 2(4), (2002) MAPH in diagnostics DNA. Following stringent washing of Test DNA the filter to remove the unbound probes, 1 µg of genomic DNA is denatured, the bound probes are released into soludried and crosslinked on to a piece of nylon membrane tion by incubating at 95°C for 5 min. Step 2 An aliquot of this solution, containing Wash off any the released probes, is then amplified in unbound amplifiable probes the quantitative phase of PCR (20–25 Step 3 cycles) and the products run on a polyHeat at 95°c for 5 min to acrylamide gel. Quantification of each 2-3 mm release bound amplifiable band of the gel allows estimation of the probes into solution amount of each probe, relative to the other probes and hence estimation of hybridise Step 1 Analyze Hybridize amplifiable copy number for that locus in the probe peak probes with genomic genomic DNA relative to the known area data DNA on filter copy number of the other loci detected Step 4 by the other probes. Amplifiable probes Amplify released probes These are DNA probes between using a pair of primers, one One of the key features is that all 100 and 600 bp long, with the fluorescently labled and probes in an experiment (together sequences corresponding to the resolve each probe by size on known as the probe set) can be amplidifference loci tested (difference t a fluorescent genotype gel fied simultaneously using one pair of colors) flanked by the same primer-binding sequence primers. This is because every probe is designed to have the same primer sites Figure 1. Principle of multiplex amplifiable probe hybridization (MAPH). Diagram illustrating the important steps in MAPH. Amplifiable probes are shown, representing the different loci tested, with flanking the locus-specific sequence. To each sharing a common primer binding sequence.. enable detection and quantification on an acrylamide gel, one of the primers is labeled either with a radioactive isotope or, more commonly, a Applications of MAPH fluorophore to enable detection by fluorescent-based frag- The applications of MAPH can be classified into two groups ment detection systems. Although gels are routinely used, flu- depending on whether the variation that is being tested is orescent-based fragment detection capillary machines, such as known a priori or not. For example, for PMP22 duplication the ABI 3100, can also be used. and deletion, the region that varies is known and probes correTwo gel lanes from a typical output from an ABI 377 are sponding to that region can be measured relative to reference shown in FIGURE 2. Each MAPH probe that detects a unique probes. This can be regarded as typing known changes. For locus at a chromosome end, is shown as a peak. The first sam- BRCA1 or subtelomeric DNA analysis, however, the exon or ple is a heterozygous deletion of 17q (17q-) and the second is chromosome end that varies, if any, is not known. This can be an unbalanced translocation between chromosomes 16 and 3, regarded as screening for new changes. In the ‘typing’ class, the application of MAPH to type copy resulting in three copies of 16q and one copy of 3p (16q+ 3p-). These rearrangements were confirmed by subtelomeric FISH number at PMP22 has been successful [UNPUBLISHED DATA]. This and the arrows on FIGURE 2 indicate the appropriate probes that probe set consists of 12 reference probes and seven test probes, are at normal diploid dosage in one sample and either deleted whose values are averaged and used to diagnose a duplication (CMT1A) or deletion (HNPP). The PMP22 assay was tested or duplicated in the other. Experimental values are normalized against other probe on 94 unaffected controls, followed by a blind test on 62 samresults to give a normalized ratio, where a value of 1 is ples previously tested by other methods [UNPUBLISHED DATA]. In a expected for normal diploid dosage. A heterozygous deletion study of normal and CMT1A patients, 30 were typed as normal, will result in a value around 0.5 and a heterozygous duplica- 31 typed as duplicate and one was typed as unknown. Sixty of tion will give a value around 1.5. When the measured values the 62 diagnoses agreed with the referral laboratory, with one for a probe for a series of normal diploid samples are plotted discordant result, which had in fact had conflicting diagnoses on a histogram, the resulting distribution is similar to a nor- from different techniques, according to the previously published mal distribution with a mean of 1. The standard deviation of study [11]. Any genetic diseases caused by a large deletion or this distribution (the standard deviation of that probe) duplication can be typed by MAPH analysis. describes how much variation or noise that probe shows in The subtelomeric probe set is in the second ‘screening’ class. MAPH. This allows any observation at the tails of the distri- Following an initial investigation into the applicability of bution, which might be a deletion (near 0.5) or a duplication MAPH in detecting subtelomeric DNA copy number changes (near 1.5), to be tested using standard hypothesis testing of a [12], a subtelomeric probe set consisting of 47 probes has been normal distribution and this feature of MAPH is elaborated constructed [13]. This allowed analysis of negative and positive in a later section of this review. controls, as well as a cohort of patients referred to the clinic with www.future-drugs.com 91 Hollox, Akrami & Armour 120 160 200 240 280 320 360 400 440 480 known 17q- sample 140 16q two copies (normal) 17q one copy 3p two copies (normal) 120 100 80 60 Amplified MAPH probes 40 20 R500 marker 0 120 140 160 200 240 17q two copies (normal) 280 320 360 16q three copies (16q+) 120 400 440 480 known 16q- 3p+ sample 3p one copy (3p-) 100 80 60 40 Amplified MAPH probes 20 0 R500 marker Figure 2. Gel electropherograms of MAPH products. Two example electropherograms produced by GeneScan™ analysis of output from an ABI 377 DNA Analyser. The x-axis shows relative fluorescence units and the y-axis shows size in base pairs. The amplified MAPH probes are shown as blue peaks, with a R500 marker (labeled with ROX dye, Genetix plc) shown as red peaks. Two positive controls are shown, 17q- and 16q+3p-, both initially identified by FISH analysis using subtelomeric probes. The probes that correspond to the chromosome ends under investigation and hence show the changes in copy number, are shown by the arrows.. Fragile X syndrome but negative for the FMR1 repeat. In 83 normal individuals, three putative polymorphic changes were found (a deletion at XpYp and duplications at 1q and XqYq), which shows that MAPH can detect and give accurate estimates for the allele frequency of uncommon variants in the population. The positive controls were correctly identified ‘blind’, demonstrating the reliability of the probe set and six copy number changes were detected in the patient cohort. This last part of the study shows the value of screening for subtelomeric changes in patients that would otherwise not be screened. The higher resolution of MAPH compared with FISH (TABLE 1) allows smaller copy number changes to be detected, especially when a probe set with several probes per chromosome end is available. By distinguishing different sized copy number variant alleles and associating them with different clinical phenotypes, it may be possible to clarify the genotype–phenotype relationship of genes in these subtelomeric regions. MAPH can be used as part of a mutation screen for any gene involved in genetic disease. Our laboratory has developed screens for BRCA1 [UNPUBLISHED DATA] and TBX5 (Holt-Oram syndrome, [14]) and development of screens for the MLH1/ MSH2 genes (involved in hereditary nonpolyposis colorectal 92 cancer) and the DMD gene [102] are underway. More general screening of genomic regions for loss of heterozygosity in cancer cells is possible and probe sets for scanning the whole genome for deletion and duplication are planned. TABLE 2 shows the MAPH probe sets constructed so far and their applications. Translating MAPH from a research to a diagnostic tool Responding to a clinical need In clinical genetics, it is increasingly common to screen PCR products from each exon of the gene for a causative mutation. Knowledge of the causative mutation enables prenatal screening of offspring for the mutation and may, in the future, help with diagnosis and treatment as different classes of mutation are found to associate with different aspects of the disease. Methods used for screening for substitutional mutations, such as denaturing gradient gel electrophoresis, do not detect copy number changes. Screening for copy number changes using MAPH will be an important tool in the mutation detector’s inventory but especially in those genetic diseases where a large proportion of mutations are due to deletions or duplications and are therefore not found using current methods. For example, the breast cancer Expert Rev. Mol. Diagn. 2(4), (2002) MAPH in diagnostics Table 2. Current applications of MAPH to analysis of genetic disease. Disease/ condition OMIM disease reference Gene Nature of mutation Charcot-MarieTooth disease 118220 PMP22 Duplication of gene Hereditary neuropathy with liabilty to pressure palsies 162500 PMP22 Deletion of gene HNPCC 114500 MLH1/ MLH2 Various, including exon deletion or duplication Holt-Oram syndrome 142900 TBX5 Various, including whole gene deletion Breast cancer 113705 BRCA1 Various, including exon deletion and duplication Duchenne/Becker 310200 muscular dystrophy DMD Various, including exon deletion or duplication Mental retardation (subtelomeric DNA) Various, unknown Deletion or unbalanced translocation of subtelomeric DNA Economics gene BRCA1 and the colorectal cancer genes MLH1 and MSH2, for which MAPH probe sets are either currently commercially available (BRCA1) or are likely to be made available in the near future. These are genes involved in the aetiology of two common diseases, where large clinical mutation screening programs are already in place in clinical centers. Diagnosis of deletions or duplications in genes for rarer disorders is likely to remain in a research setting for the foreseeable future. Diagnosis of genetic diseases where the only mutation is a change in copy number, for example PMP22, will be made considerably easier by implementation of MAPH. Using several different probes to detect the mutation results in negligible false-positive and false-negative rates and can clarify uncertain diagnoses made by other methods. It has become increasingly clear that many cases of mental retardation are associated with copy number changes in subtelomeric DNA at the ends of chromosomes. Indeed, it has been suggested that every patient with mental retardation that cannot otherwise be explained should be screened for subtelomeric copy number changes [15]. MAPH is the ideal high-throughput technique for detecting these changes, at the very least prior to detection by FISH and an initial probe set for this task has been made www.future-drugs.com commercially available by Genetix PLC (Hampshire, UK). Since MAPH resolution can be carefully controlled by designing probes at appropriate intervals, it is possible, with probe sets covering subsets of chromosome ends, to map each copy number change at high resolution and identify genes that appear to cause the mental retardation phenotype. Since many different chromosome ends and hence many different genes, are involved, this opens up genotype–phenotype correlation studies and a gateway into understanding how the mutation causes the disease. Where MAPH can be used in high-throughput screening, such as detecting mutations in the BRCA1 gene and screening subtelomeric DNA in mental retardation patients, the cost of the technique must be low enough and its benefits be great enough to justify its use. This is the case in all health service systems whether funded through private insurance or through general taxation. The cost of screening all subtelomeric ends for one sample using FISH is about US$150, whilst the cost of screening all subtelomeric ends by MAPH for one sample is about US$5. This excludes cost of equipment and labor, which in both cases will be substantially less for MAPH due to higher throughput and decreased hands-on time. In situations where the alternative techniques are not directly comparable, such as screening for deletions and duplications in BRCA1 gene, MAPH is much more cost-efficient. The standard methods for copy number variation in BRCA1 are either multiplex quantitative PCR or junction fragment analysis by PCR. Both these methods focus on a small number of exons that are known to be commonly involved in copy number changes. In contrast, MAPH screens all exons and can detect all copy number changes, with a similar throughput level to PCR. The cost advantages outlined above are given even greater weight when the prevalence of the mutations is accounted for and therefore, the proportion of the total population that may have use for genetic diagnostics using MAPH. Automation Allied to the economic considerations of MAPH is the potential for automation. The less labor and time required per test, the less expensive the test. In its current research setting, MAPH involves considerably less hands-on time than other techniques. It has the advantage that the software required for analysis is standard fragment analysis software (such as GeneScan) and statistical analysis of results is carried out using standard spreadsheets with custom designed macros. Further customization of this analysis frontend will shorten hands-on time even more. The most labourintensive and rate-limiting steps are preparation of filters and washing of these filters following hybridization. It is probably possible to modify existing technology to allow these steps to be automated. For example, DNA could be spotted onto precut filters by a robot and washing could be done by using a pump cycling wash solution with the filters. Transfer of filters to individual tubes to allow release of bound probes into PCR buffer would be more of a technical challenge. 93 Hollox, Akrami & Armour Nevertheless, the high-throughput nature of the technique, even with minimal automation, means that the absence of this additional technology will not prevent its effective use in clinical genetic diagnosis. Multiplicity A key advantage of MAPH is the large number of loci that can be analyzed at once and the number of loci is determined by the number of probes in the probe set. The subtelomeric probe set has 47 probes and we have had success with a probe set of 61 probes. However, using gel electrophoretic analysis, each probe has to be resolved satisfactorily on a gel and is hence the number of probes in a probe set is limited by gel resolution. A lower limit on probe size is 100 bp, since hybridization efficiency falls below this point and the PCR places a practical upper limit of around 600 bp, so that allows for around 100 probes spaced at 5 bp intervals. Detection of MAPH products by rehybridization to arrayed probes would overcome this limitation. In this method, MAPH is performed as normal. However, when the probes are recovered after hybridization, instead of separation and quantification of the probes by gel electrophoresis, they are rehybridized back to a large excess of probe attached to an array. Due to the large excess of probe on the array, rehybridization will proceed to near-completion and the amount of probe bound to the array can be quantified. Microarray MAPH will allow detection and quantification based on sequence, not size and is limited only by the number of probes attached to the array and the number of arrays that can be tested (FIGURE 3). For example, if one array has 400 different probes immobilized to it, then 400 probes can be included in the probe set for the initial hybridization to genomic DNA and hence 400 separate loci can be tested. If hybridization to multiple arrays can be performed, then the number of loci is, theoretically, the number of arrays x400. However, there is likely to be an upper limit to the number of probes included in the probe set due to possible interference between probes and hybridization kinetics of the initial hybridization steps. Microarray-based MAPH is currently being developed by two groups. One group is using standard microarray technology with oligonucleotide probes arrayed on a glass slide. In our laboratory, however, the oligonucleotide probes are arrayed on a porous aluminium oxide substrate which not only allows faster and more specific hybridization times but continuous monitoring of the hybridization kinetics (Pamgene BV, The Netherlands [103]). This type of microarray technology is more suited to a high-throughput diagnostic situation. Statistics Gel electrophoretic analysis of MAPH products Recovered MAPH probes amplified with one unlabeled primer and one fluorescently labeled primer Run amplified products on electrophoresis gel with fluorescent-based fragment detection (e.g., ABI 377). Number of probes that can be resolved depends on gel resolution – no more than approximately 100 Quantify area under each band (peak) using standard fragment analysis software (e.g., Genescan and Genotyper) Microarray analysis of MAPH products Recovered MAPH probes amplified using unlabeled primers and fluorescently label after amplification Hybridize amplified products back to excess of MAPH probe immobilized in arrays on a solid support. Number of probes that can be resolved depends on number of spots on array (400) and number of arrays (theoretically limitless) Quantify signal on each array spot using packaged array analysis software Figure 3. Gel-based and microarray-based analysis of MAPH products. Figure illustrating the principal differences between the two methods for analysis of MAPH products. Both methods begin with the recovered MAPH probes after hybridization to genomic DNA immobilized on a nylon filter. In the gel electrophoresis method, the products are labeled during amplification by a fluorescent primer, then visualized and quantified on a standard electrophoretic gel with fluorescence detection. In the microarray method, the products are rehybridized back to an excess of probe spotted on the array. The amount of hybridization on each spot corresponds to the amount of probe in the solution and hence the dosage: white, no hybridization, no probe in solution, dosage of zero; dark gray, full hybridization, probe in solution, dosage of two; pale gray, full hybridization but half the amount of probe, dosage of one (hemizygosity). 94 The quantitative nature of MAPH as opposed to the qualitative nature of techniques, such as cytogenetics or FISH, enables statistical analysis of the resulting data. Indeed, the amount of data produced by MAPH requires statistical analysis to interpret the results correctly and to gauge the rate of false-positives and false-negatives. For certain applications this is straightforward. If the probe set consists of several test probes, that show dosage change and several reference probes, that do not show dosage change, then each test probe can be tested individually at a certain significance level. An alternative approach would be to derive a value (such as the mean or median) taken from the test probes and plot that value for each sample so that samples with the same dosage cluster together and can be distinguished from clusters of samples of other dosage. Discriminant analysis statistics may also help diagnosis in clinical diagnostic situations. However, in the screening cases, such as the subtelomeric probe set, there is no a priori knowledge of which probes will show dosage changes and which probes will not. Therefore, each data point must be tested to determine whether it shows a Expert Rev. Mol. Diagn. 2(4), (2002) MAPH in diagnostics significant change from normal diploid dosage and because of the large number of observations simultaneously generated by MAPH, statistical analysis problems due to multiple testing may occur. For example, a single gel’s worth of results from the current subtelomeric probe set will produce 2115 data points (45 samples x 47 tests per sample) and assuming a normal distribution, standard hypothesis testing using a 5% significance level would produce over 100 apparent positives purely by chance. This does provide a valuable level of screening, reducing the target sample from a size impractical to screen by FISH to something more manageable. Using standard corrections for multiple testing, such as the Bonferroni correction, will result in fewer positive calls but risks missing a fair number of truepositives due to an increase in the false-negative rate. The balance between keeping retests/confirmations to a minimum by a low false-positive rate (high specificity) and ensuring a low false-negative rate (high sensitivity) is important. In a screening situation, a reasonable rate of false-positives may be acceptable if the false-negative rate is kept to an absolute minimum. Where the cost of any confirmatory technique is expensive, such as FISH, the MAPH false-positive threshold can be set so that the number of FISH tests can be within budget. FIGURE 4 shows the different possible consequences of changing the false-positive and false-negative rates for one probe. FIGURE 4A shows a normal distribution (approximately a mean of 1) of samples with normal diploid dosage and a normal distribution (approximately 0.5) of samples with haploid dosage – one copy is deleted. The threshold is arbitrarily set at 0.75 (corresponding to a significance level of p = 0.006 when the standard deviation (noise) of the probe is 10%) and the shaded areas correspond to the false-negative samples (grey) and the false-positive samples (black). FIGURE 4B shows that the simplest way to reduce the falsenegative rate is to increase the threshold, for example, up to 0.8 (significance level p = 0.022 when the standard deviation of the probe is 10%). However, this has the effect of increasing the false-positive rate. Similarly, reducing the threshold to 0.6 would decrease the false-positive rate yet increase the false-negative rate. The most satisfactory method of reducing false calls is to improve the technology so that probe noise (standard deviation) is reduced. Even a small reduction in probe noise can have large effects on the rate of false-positive and false-negative calls (FIGURE 4C). For example, with a false-positive rate of 1%, a reduction of the standard deviation of a probe from 10 to 9% reduces the false-negative rate six times. We are beginning to understand the origins of measurement error in MAPH and why some probes are ‘noisier’ than others and this understanding will be essential for further development of the technique. With the current state of the technology, repeat testing is the best method to reduce false calls and distinguish signal from noise. The low cost and high-throughput nature of MAPH makes duplicate and triplicate testing practical in a diagnostic situation. Duplicate testing of every sample, followed by calculating the mean of the two independent duplicate results should produce a distribution curve with a standard deviation of σ/ 2, www.future-drugs.com Distribution of probes Distribution of probes for deleted loci for normal diploid loci a 0.50 0.75 1.00 b 0.50 0.80 1.00 c 0.50 0.75 1.00 False-negative False-positive Figure 4. Effect of varying threshold or standard deviation on error rates. Diagram illustrating how false-positive or false-negative rates can be altered by understanding the properties of the Gaussian normal distribution curve. In each case, a normal distribution about 1.0 (for samples showing normal diploid dosage) and a normal distribution about 0.5 (for samples showing heterozygous deletions) is shown. The area under the curve corresponding to the false-negative rate is shown in light gray and the area under the curve corresponding to the false-positive rate is shown in black. False-positive and negative rates using a threshold of 0.75. Effect on false-positive and -negative rates by altering the threshold to 0.8. Effect on false-positive and -negative rates by lowering the probe standard deviation (noise). where σ is the standard deviation of the curve produced by testing the samples once. Similarly, triplicate testing will result in a standard deviation of σ/ 3. Unfortunately, taking the mean value of multiple results is at best an approximation and may introduce systematic bias into the data analysis. This is because multiple results from some probes are not independent – they are correlated [13]. To account for this correlation, a multivariate analysis approach is needed to analyze the data. A bivariate approach was used to analyze duplicate data from the subtelomeric probe set and we are developing these methods so that future multiple data can be analyzed in a straightforward manner. 95 Hollox, Akrami & Armour Patent issues MAPH is patented by the University of Nottingham WO0053804 (2001) and limited licenses have been granted to Genetix, PLC for commercialization of probe sets for research [103] and to PamGene BV for microarray diagnostic analysis [104]. The technique can be used for academic and research purposes freely but for commercial diagnostic applications the Research Business Unit at the University of Nottingham must be contacted [105]. Expert opinion In its current state of development, MAPH is ideal for comprehensively screening disease genes, such as BRCA1 for copy number variation in exons and for genotyping known copy number variations, such as at the PMP22 gene for CMT1A and HNPP. Applying these tests in diagnosis should be very straightforward. We would also recommend MAPH analysis of patients where the gene causing the disease is known but standard mutation detection techniques have found no causative change. Heterozygous deletions and duplications are a significant proportion of genetic mutations and PCR-based detection methods, such as DHPLC or DGGE will not detect these mutations. Screening subtelomeric DNA for copy number changes in patients with mental retardation has a huge potential for routine diagnostic use instead of occasional research use but more development is needed both in understanding and improving the technique and in applying statistics and new software to cope with the large amount of data it can produce. The current rate of 6% false-positives with 2% false-negative rate by testing in duplicate [13] is not quite sufficient to replace FISH testing, although it is ideally suited for a screening role. When compared with a clinical checklist as a screen, where a 5% false-positive rate generates a 81% false-negative rate and even a 73% false-positive rate generates an 11% false-negative rate [16], the usefulness of MAPH analysis over symptom-based classification systems is evident. Five-year view Developments in technology The ability to perform MAPH analysis on very small amounts of DNA will open a wide variety of applications, including prenatal diagnosis and analysis of paraffin-embedded specimens. At present, 0.5 µg is the minimum amount of DNA for a reliable MAPH analysis but our laboratory is currently developing methods to extend MAPH to nanogram amounts of DNA. Development of MAPH on array systems has been described above and this undoubtedly will become the standard platform for some MAPH analyses in the future. We must also remember that MAPH is fundamentally a lowtech method that can be aided with high-tech equipment. Since at its simplest level, it only requires the equipment and consumables available in any molecular biology laboratory, it is an ideal method for laboratories where funds for research and clinical diagnostics are limited. MAPH is an extremely accessible 96 technology and developments to maintain and implement MAPH in a low-tech setting will be needed over the next few years. Developments in applications At the time of writing, there are currently two MAPH probe sets commercially available, BRCA1 and subtelomeric DNA, both marketed by Genetix Ltd. [104]. The range of ‘off-theshelf ’ probe sets for use by other laboratories will undoubtedly increase, so that within 5-years a variety of applications, for example typing the PMP22 gene and screening the MLH1/ MSH2 genes, will each be covered by a probe set. A new subtelomeric probe set, with more than one probe covering each chromosome end, is a priority. As well as being a routine part of mutation screening procedures and subtelomeric analysis, development of a MAPH probe set for whole genome scanning, coupled with array-based MAPH will be of enormous benefit, especially for cancer genetics. At 1 Mb resolution, 3000 probes will be needed and at 200 kb resolution 15,000 probes will be needed. Although perfectly possible, this will require a large amount of work with commensurate funding, probably out of the academic sector. In practice, a whole genome scanning kit will probably consist of several probe sets, although it may not be too much of a technical challenge to screen the whole genome at 200 kb resolution (15,000 loci/probes) in one test. Acknowledgements EJ Hollox is supported by The Wellcome Trust grant number 060578 and SMA is supported by the Ministry of Health of the Islamic Republic of Iran. Key issues • Multiplex amplifiable probe hybridization (MAPH) is a highthroughput technique for identifying and typing copy number variation in DNA, such as deletions and duplications and costs an order of magnitude less than fluorescent in situ hybridization. • MAPH has been applied to screen BRCA1, PMP22 gene (for Charcot-Marie-Tooth Type 1A and hereditary neuropathy with pressure palsies), DMD (for Duchenne Muscular Dystrophy), MLH1/MSH2 (for hereditary nonpolyposis colorectal cancer) and subtelomeric DNA for copy number variation. • MAPH is currently being developed from a research tool into a high-throughput diagnostic tool. • MAPH provides quantitative data amenable to statistical analysis, that can produce results on which clinical decisions can be based. Suitable thresholds can be used so that clinical decisions can be taken in the context of patient need and economic restrictions. • MAPH has the potential to be used to scan the whole genome at very high resolution. Expert Rev. Mol. Diagn. 2(4), (2002) MAPH in diagnostics References Papers of special note have been highlighted as: • of interest •• of considerable interest Armour JA, Sismani C, Patsalis PC, Cross 1 G. Measurement of locus copy number by hybridization with amplifiable probes. Nucleic Acids Res. 28(2), 605–609 (2000). •• This is the ‘proof of principle’ paper describing MAPH, patented by the University of Nottingham WO0053804 (2001). 2 3 4 5 • 6 Knight SJ, Flint J. Perfect endings: a review of subtelomeric probes and their use in clinical diagnosis. J. Med. Genet. 37(6), 401–409 (2000). Flint J, Wilkie AO, Buckle VJ et al. The detection of subtelomeric chromosomal rearrangements in idiopathic mental retardation. Nature Genet. 9(2), 132–140 (1995). Knight SJL, CM Lese, KS Precht et al., An optimized set of human telomere clones for studying telomere integrity and architecture. Am. J. Hum. Genet. 67(2), 320–332 (2000). Ji Y, Eichler EE, Schwartz S, Nicholls RD. Structure of chromosomal duplicons and their role in mediating human genomic disorders. Genome Res. 10(5), 597–610 (2000). Demonstrates the importance of low copy number chromosomal repeats in causing large deletions and duplications, which may lead to genetic disease. Lupski JR, Chance PF, Garcia CA. Inherited primary peripheral neuropathies. Molecular genetics and clinical implications of CMT1A and HNPP. JAMA 270(19), 2326–2330 (1993). www.future-drugs.com 7 Woodward K, Kendall E, Vetrie D, Malcolm S. Pelizaeus-Merzbacher disease: identification of Xq22 proteolipidprotein duplications and characterization of breakpoints by interphase FISH. Am. J. Hum. Genet. 63(1), 207–217 (1998). 8 Francke U. Williams-Beuren syndrome: genes and mechanisms. Hum. Mol. Genet. 8(10), 1947–1954 (1999). 9 den Dunnen JT, Bakker E, van Ommen GJ, Pearson PL. The DMD gene analysed by field inversion gel electrophoresis. Br. Med. Bull. 45(3), 644–658 (1989). Petrij-Bosch A, Peelen T, van Vliet M et al. BRCA1 genomic deletions are major founder mutations in Dutch breast cancer patients. Nature Genet. 17(3), 341–345 (1997). •• Demonstrates the importance of detecting deletions and duplications in mutation screening of genes. 11 Rowland JS, Barton DE, Taylor GR. A comparison of methods for gene dosage analysis in HMSN Type 1. J. Med. Genet. 38(2), 90–95 (2001). 10 12 Sismani C, Armour JA, Flint J et al. Screening for subtelomeric chromosome abnormalities in children with idiopathic mental retardation using multiprobe telomeric FISH and the new MAPH telomeric assay. Eur. J. Hum. Genet. 9(7), 527–532 (2001). 13 Hollox EJ, Atia T, Parkin T, Armour JAL. (Submitted). 14 Akrami SM, Winter RM, Brook JD, Armour JA. Detection of a large TBX5 deletion in a family with Holt-Oram syndrome. J. Med. Genet. 38(12), E44 (2001). • 15 16 Shows how MAPH was used to detect an almost whole gene deletion as a cause of a genetic disease in a family, which had been previously missed using other mutation detection techniques. Zackai EH, Krantz ID, Ming JE et al. Subtelomeric testing: don’t leave clinic without it. Am. J. Hum. Genet. 69(4), S326 (2001). de Vries BB, White SM, Knight SJ et al. Clinical studies on submicroscopic subtelomeric rearrangements: a checklist. J. Med. Genet. 38(3), 145–150 (2001). Websites 101 MAPH home page www.nottingham.ac.uk/~pdzjala/maph/ maph.html 102 Leiden University Medical School Duchenne Muscular Dystrophy pages www.dmd.nl/ 103 Pamgene BV homepage www.pamgene.com/ 104 Genetix Ltd homepage www.genetix.com/ 105 University of Nottingham Research Business Unit www.nottingham.ac.uk/rbu/ Affiliations • Edward J Hollox, PhD Postdoctoral Research Associate, • Seyed M Akrami, MD Postgraduate Research Student, • John AL Armour, BM, BCh, PhD Reader in Genetics, [email protected] • Institute of Genetics, Queen’s Medical Centre, University of Nottingham, NG7 2UH, UK Tel.: +44 115 970 9398 Fax: +44 115 970 9906 97