* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download PATHOPHYSIOLOGY OF THE IMMUNE SYSTEM
Survey
Document related concepts
Complement system wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
DNA vaccination wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Adaptive immune system wikipedia , lookup
Innate immune system wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Transcript
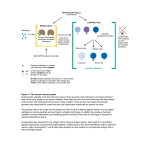
PATHOPHYSIOLOGY OF THE IMMUNE SYSTEM. IMMUNOLOGIC TOLERANCE. RESPONSES TO A FOREIGN ANTIGEN. CONGENITAL AND ACQUIRED IMMUNODEFICIENCIES Definition and notion Allergy is an abnormal form of immunologic reactivity characterized by a specific increase in reactivity (hypersensitivity) to repeatedly administered allergen. It is manifested by more or less pronounced damage to the tissues of the body or serious functional disturbances in various organ systems. Antibodies: Macromolecular serum proteins from the group of the γ-globulins (immunoglobulins) that specifically bond to matching antigen bonding sites (antigenic determinants or epitopes). Antigen: A substance the body recognizes as “foreign” and that triggers a specific immune response (antisomatogen). Autoimmune Disorders: Clinical syndromes that occur in the absence of exogenous influences and are maintained throughout the patient’s life occur by humoral or cell-mediated immune reactions. These reactions are directed at specific endogenous substrates. Autoimmune diseases result from a failure of self-tolerance. CD = cluster of differentiation by which monoclonal antibodies are defined. Cell-mediated immunity is a delayed immune response. Cell-mediated Immune reactions mediated by T lymphocytes This involves the T lymphocytes that have learned to differentiate between autologous material (“self”) and foreign material (“non-self”). Complete antigen: A substance that induces an immune response and that can specifically react with the product of that response (the antibody). Incomplete antigen (hapten): A low-molecular-weight substance (a short peptide or drug) that only acts as an antigen once it binds to macromolecules. Humoral immunity: This involves the B lymphocytes, which create “antidotes” (antibodies) that circulate in body fluids. Humoral immunity is an immediate immune response Hypersensitivity Reactions General definition: Excessive pathogenic reaction of a sensitized body to renewed contact with the sensitizing antigen. Immune-Regulating Antigens Synonyms: major histocompatibility complex (MHC), human leukocyte antigen (HLA), transplantation antigen: Cellular surface antigen that enables the T lymphocytes to identify foreign cells among the body’s own cells and in sodoing to distinguish between “self” and “nonself.” Immune response is the coordinated reaction of these cells and molecules to infectious microbes. Immune system is the collection of cells, tissues, and molecules that mediate resistance to infections Immunity is defined as resistance to disease, specifically infectious disease. Immunologic tolerance is a state is which the individual is incapable of developing an immune response to a specific antigen. Natural killer cells trigger apoptosis in cells without MHC. Self-tolerance refers to lack of responsiveness to an individual's antigens. 1. Physiologic Concepts Immunity - the ability of multi-cellular organisms to maintain a constant internal environment (homeostasis) at macromolecular level. The main functions of the immune system: -inactivation, destruction and elimination of exogenous macromolecules and microorganisms; -destruction of endogenous macromolecules constantly produced in the body, the old, defective and transformed (tumor) cells (ie immune surveillance); 1 -regulation of various body functions by the formation of antibodies to carrier proteins, hormones, receptors and other signaling molecules. Immunity: •Non-specific (hereditary) immunity: a) humoral component - the complement system proteins, interferons; b) the cells - macrophages, neutrophils, natural killer (NK), eosinophils, dendritic cells (DC). •Specific (acquired) immunity: a) humoral factors - immunoglobulins or antibodies; b) cells - T and B lymphocytes. The Specific and Innate Immunity Host defense mechanisms consist of innate immunity, which mediates the initial protection against infections, and adaptive immunity, which develops more slowly and mediates the later, even more effective, defense against infections. The term innate immunity (also called natural or native immunity) refers to the fact that this type of host defense is always present in healthy individuals, prepared to block the entry of microbes and to rapidly eliminate microbes that do succeed in entering host tissues. The first line of defense in innate immunity is provided by epithelial barriers and by specialized cells and natural antibiotics present in epithelia, all of which function to block the entry of microbes. The innate immune response includes the inflammatory responses to infection or injury and the white blood cells that participate in those responses: the neutrophils, the basophils, eosinophils, and monocytes and macrophages. The inflammatory response is stimulated after tissue injury or infection, with the goal of delivering white blood cells and platelets to the tissues to limit damage and promote healing. The inflammatory reactions are not characterized by specificity or memory, but they are fast and effective. Adaptive immunity (also called specific or acquired immunity) is the type of host defense that is stimulated by microbes that invade tissues, that is, it adapts to the presence of microbial invaders. Adaptive immune responses generate mechanisms that are specialized to combat different types of infections and involve activation of the B and T lymphocytes. B and T lymphocytes are capable of responding with specificity and precision to virtually any foreign molecule an individual may encounter in a lifetime. There are two types of adaptive immunity, called humoral immunity and cell-mediated immunity that are mediated by different cells and molecules and are designed to provide defense against extracellular microbes and intracellular microbes, respectively. Humoral immunity is mediated by proteins called antibodies, which are produced by cells called В lymphocytes. Antibodies do not have access to microbes that live and divide inside infected cells. Defense against such intracellular microbes is called cell-mediated immunity because it is mediated by cells called T lymphocytes. Once the original response is made, the B or T cell retains a memory of it. If a second encounter with that molecule occurs, the B- or T-cell response will be faster and more effective than before. There are many linkages among the various layers of host defense. It is important to understand the relationships of components of innate and specific immune system. Tissue of the Immune Response Lymphoid Tissue Lymphoid tissue is the seat of the immune response. Central Lymphoid Tissue The central lymphoid tissue is composed of the thymus and bone marrow, in which primitive lymphoid cells in the fetus develop and are primed. (Priming refers to the early period of lymphocyte development when diversity occurs and tolerance develops. In humans, development of diversity and tolerance is considered essentially complete within a few months after birth.) Peripheral Lymphoid Tissue 2 The peripheral lymphoid tissue is composed of lymph nodes, spleen, Waldeyer's ring (the tonsils) in the oropharynx, and gut-associated lymphoid tissue, in which reside the mature lymphocytes that respond to antigenic stimuli. The peripheral blood also contains lymphocytes. Circulating lymphocytes constitute a pool of cells that is being continuously exchanged with cells of the peripheral lymphoid tissue. Cells of the Immune Response The immune response is under the control of specialized cells, the white blood cells. White blood cells protect the body from infection and cancer and assist in healing. White blood cells include the neutrophils, eosinophils, basophils, monocytes, and macrophages, and the B and T lymphocytes. Platelets are fragments of cells that also play a role in healing. All white blood cells and platelets derive from a basic stem (originator) cell, called the pluripotent stem cell, in the bone marrow. From this cell, succeeding generations of stem cells differentiate and commit to producing one type of cell. We will return to the detailed discussion to major cell types involved in adaptive immune responses (table 1). Tabl. 1 The principal cells of the immune system. The major cell types involved in immune responses, and their functions, are shown. Cell type Principal function(s) Specific recognition of antigens Lymphocytes: В В lymphocytes: mediators of humoral immunity lymphocytes; T lymphocytes; T lymphocytes: mediators of cell-mediated immunity natural killer cells Natural killer cells: cells of innate immunity Capture of antigens for display to lymphocytes: Dendritic ceils: initiation of T cell responses Antigen-presenting cells: Macrophages: initiation and effector phase of cell-mediated dendritic cells; macrophages; immunity follicular dendritic cells Follicular dendritic cells: display of antigens to В lymphocytes in humoral immune responses Elimination of antigens: T lymphocytes: helper T (Synonyms: CD4+ T cells, TH cells) Effector cells: T cells and cytolytic T lymphocytes lymphocytes; macrophages; Macrophages and monocytes: cells of the mononuclear phagocyte granulocytes system Granulocytes: neutrophils, eosinophils Lymphocytes Lymphocytes include the B and T lymphocytes and a type of cell called the natural killer (NK) cell. Lymphocytes are produced in the bone marrow and mature there or in other lymphoid tissues. Lymphocyte proliferation in the fetus is genetically controlled—a small number of stem cells proliferate to produce the numerous T and B lymphocytes populating the lymphoid tissues at birth. Lymphocyte proliferation in postnatal life occurs as part of the immune response—only those lymphocytes capable of recognizing a particular antigen respond to produce effector cells that respond to the given antigen. Although all lymphocytes are morphologically similar and rather unremarkable in for these proteins is the "CD" (cluster of differentiation) numerical designation, which is used to delineate surface proteins that define a particular cell type or stage of cell differentiation and are recognized by a cluster or group of antibodies. The natural killer (NK) cells react to foreign molecules. They do not demonstrate specificity, that is, they may respond to more than one foreign molecule. 3 T lymphocytes develop in the fetal thymus. After maturation, T lymphocytes are distributed by the circulation to the T-cell domains of peripheral lymphoid tissue. T lymphocytes continuously and actively recirculate between the peripheral blood and peripheral lymphoid tissue T Cell Transformation Following stimulation (activation) by specific antigen, T lymphocytes transform into large, actively dividing cells known as transformed T lymphocytes, or T immunoblasts, which then divide to produce effector T cells. Effector T lymphocytes morphologically resemble resting small lymphocytes and are often termed sensitized, cytotoxic, or killer T cells (CTLs). These cells express CD3 and CD8. Cells bearing surface antigens that are recognized by effector T cells are subject to direct cell killing by the T cells (cytotoxic or killer cells). Direct toxicity occurs in immunologic response to antigens on the surface of neoplastic cells, transplanted tissues, and virus-infected cells. Cytotoxic T cells apparently cause lysis by producing holes in the surface membranes of antigen-positive cells. Effector T cells play a crucial role in regulating the immune response by producing soluble proteins (lymphokines) that regulate the functions of certain cells, eg, macrophages and other lymphocytes. Two important subtypes of T lymphocytes are instrumental in regulating the function of the immune response. Helper T cells (TH cells, CD4 antigen-positive) and suppressor T cells. Helper cells express CD3 and CD4. These cells are classified according to their function. — TH1 cells defend against viruses and bacteria. They activate natural killer cells, resulting in release of interferon-c and IL-2. This activates the TH1 cells, which in turn activate macrophages and cytotoxic T cells. TH1 cells are inhibited by IL-4. — TH2 cells defend against worms and other parasites. These invaders release IL-4, which (a) activates B cells, leading to production of IgG and IgE and (b) enlists the aid of eosinophilic mast cells. TH2 cells are inhibited by interferon-c. The antigen receptors of T lymphocytes only recognize peptide fragments of protein antigens that are bound to specialized peptide display molecules called major histocompatibility complex (MHC) molecules, on the surface of specialized cells called antigen-presenting cells (APCs). Suppressor T cells (CD8 antigen-positive) inhibit B cell activation and regulate immunoglobulin synthesis. Suppressor T cells also display similar regulatory effects in cellmediated immunity B lymphocytes (B cells) mature in the bone marrow. After maturation, a B cell circulates in the blood in an inactive state and becomes active only after exposure to a specific molecule, usually a protein or large carbohydrate of foreign origin, to which it has been genetically programmed during fetal development to respond. When activated, the B cell becomes a plasma cell, a specialized cell that mounts an immune response against the molecule that activated it. B lymphocytes comprise the humoral immune system, meaning that they circulate in the blood (the humor). T lymphocytes comprise the cellular immune system. T cell maturation occurs during passage through the thymus gland. Like a B cell, the mature T cell stays inactive until it encounters the specific molecule to which it has been programmed during development to respond; once it does so, it becomes activated and may directly attack and destroy the cell expressing that molecule. The T cell may also release chemicals that alert B cells to the presence of the invader, thereby initiating a humoral response. T cells can stimulate or in some circumstances inhibit the inflammatory responses via the release of pro- or anti-inflammatory peptides known as cytokines. T cells are important for recognizing and destroying parasites and viruses that hide intracellularly, where the B cells are unable to encounter them. В cells express membrane forms of antibodies that serve as the receptors that recognize antigens and initiate the process of activation of the cells. Antigen-Presenting Cells 4 The common portals of entry for microbes, namely, the skin, gastrointestinal tract, and respiratory tract, contain specialized cells located in the epithelium that capture antigens and transport them to peripheral lymphoid tissues. This function of antigen capture is best understood for a cell type called dendritic cells because of their long dendrite-like processes. Dendritic cells capture protein antigens of microbes that enter through the epithelia and transport the antigens to regional lymph nodes. Here the antigen-bearing dendritic cells display portions of the antigens for recognition by T lymphocytes. If a microbe has invaded through the epithelium, it may be phagocytosed by macrophages that live in tissues and in various organs. Macrophages are also capable of displaying protein antigens to T cells. Cells that are specialized to display antigens to T lymphocytes have another important feature that gives them the ability to trigger T cell responses. These specialized cells respond to microbes by producing surface and secreted proteins that activate naive T lymphocytes, thus providing the "second signals" (see bellow) for T cell proliferation and differentiation. Specialized cells that display antigens to T cells and provide second signals are called "professional" APCs. The prototypic professional APCs are dendritic cells, but macrophages and a few other cell types may serve the same function. Much less is known about cells that may capture antigens for display to В lymphocytes, or even if such specialized cells exist. В lymphocytes may directly recognize antigens of microbes, or cells in lymphoid organs may capture antigens and deliver them to В cells. Effector Cells The cells that eliminate microbes are called effector cells and consist of lymphocytes and other leukocytes. We have earlier referred to the effector cells of the В and T lymphocyte lineages. The elimination of microbes often requires the participation of other, nonlymphoid leukocytes, such as granulocytes and macrophages. These leukocytes may function as effector cells in both innate immunity and adaptive immunity. In innate immunity, macrophages and some granulocytes directly recognize microbes and eliminate them. In adaptive immunity, the products of В and T lymphocytes call in other leukocytes and activate the leukocytes to kill microbes. Self-Antigens Each individual possesses cell surface antigens that are unique to that individual. These antigens, the MHC proteins, serve as a sort of cellular fingerprint. In humans, these proteins are sometimes called histocompatibility antigens. Human MHC proteins are also called human leukocyte antigens (HLA), because these proteins were discovered as antigens of leukocytes that could be identified with specific antibodies. There are two groups of MHC proteins: MHC I and MHC II. The MHC I proteins are found on nearly all cells of the body except the red blood cells. The MHC II proteins are found only on the surface of macrophages and B cells. MHC proteins have two functions: (1) they present self-antigens to T cells, and (2) they bind foreign antigens and present these to T cells. The MHC I molecules bind and present antigens only to cytotoxic T cells. The MHC II molecules bind and present antigens only to helper T cells (both TH1 and TH2 types). The Role of the MHC Proteins in Controlling Immunity After a foreign or unknown cell has been phagocytized by a macrophage or has become bound to a B cell, antigens from the cell are expressed on the macrophage or B cell adjacent to host MHC II antigens. The foreign antigens and the MHC II antigens are presented together to passing helper T (CD4) cells. Each passing helper T cell compares the foreign or unknown antigen to the host's MHC II antigens. If in comparing the unknown antigen to the MHC II antigens, a helper T cell recognizes the antigen as foreign, the helper T cell will secrete cytokines that activate the B cell to become an antibody-secreting plasma cell. If the antigen presented is seen by helper T cells as too similar to the MHC II proteins on the B cell or macrophage, the helper T cells will not become activated, or perhaps may become T regulatory cells, and the antigen will not be attacked. To activate cytotoxic (CD8) cells, MHC I proteins must be presented in association with the unknown or foreign antigen. All cells express MHC I proteins; therefore, any cell can present 5 foreign antigens to CD8 cells for comparison. Cells infected with a virus make abnormal proteins, as do cancerous cells. These abnormal proteins are recognized as antigens and presented to CD8 cells along with host MHC I proteins. When cytotoxic T cells encounter abnormal proteins compared to the MHC I proteins, they are stimulated to initiate killing of the cells. Antigens Antigens are molecules that evoke an immune response when introduced into a host that recognizes them as foreign, or nonself. They are relatively large rigid molecules (typically proteins or polysaccharides) with a molecular weight in excess of 5000. Smaller molecules called haptens— including some lipids, carbohydrates, oligopeptides, nucleic acids, and various drugs that are not large enough to alone act as antigens—may become antigenic when combined with largermolecular-weight carriers. The exact part of the antigen or hapten that reacts with the immune system is called the antigenic determinant, or epitope. It is usually a small portion of the molecule and is frequently composed of only a few (four to eight) amino acids or sugar residues. A single antigenic molecule may bear several different epitopes. These different antigenic determinants are recognized separately by the immune system, and antibodies are produced that provide a reciprocal fit (ie, they show specificity;. Antigens that can bind to a T or B lymphocyte include those present on the cell wall of bacteria or mycoplasmas, the coat of a virus, or on certain pollens, dusts, or foods. Every cell of a person has surface proteins that would be recognized as foreign antigens by B or T lymphocytes from another person. If an antigen causes either the B or T lymphocyte to become activated and to multiply or differentiate further, it is an immunogenic antigen. Immunoglobulins/Antibodies Antibodies are proteins called immunoglobulins. Immunoglobulins (fig 3) are synthesized by plasma cells that differentiate from transformed, antigen-stimulated B lymphocytes (B immunoblasts). The immunoglobulin molecule consists of four polypeptide chains: two heavy (H) and two light (L) chains held together by disulfide bonds. The H chain has one variable (V) and at least three constant (C) regions. The L chain has one V and one C region. Together, the V regions form a pocket known as the antigen-binding site. This site is located within the antigen-binding fragment (Fab) region of the molecule. Part of the C region of the H chains forms the crystallizable fragment (Fc) region of the molecule. This region mediates effector mechanisms, such as complement activation, and is the portion of the immunoglobulin molecule bound by Fc receptors on phagocytic cells, mast cells, and basophils. Each immunoglobulin molecule also has two antibody-combining sites (except for the immunoglobulin M [IgM] molecule, which has ten, and IgA, which may have two or more). Fig 1 The immunoglobulin molecule 6 There are five known classes of immunoglobulins: IgG, IgM, IgA, IgE, and IgD (see the table 15). They are distinguished by the constant portions of their heavy chains. However, each class has a kappa or lambda light chain, which gives rise to many subtypes and provides almost limitless combinations of light and heavy chains that give immunoglobulins their specificity. A clone of B cells is specific for only one antigen, and the V regions of its Ig light chains determine that specificity. However, the class of immunoglobulin can change if the association between the cell's V region genes and heavy chain C region genes changes through a process known as isotype switching. For example, a clone of B cells genetically programmed to recognize tetanus toxoid will first make an IgM antibody against tetanus toxoid and later an IgG or other antibody against it. shows the five classes of immunoglobulins. Tabl 2. Classification of immunoglobulins Class IgA IgD IgE IgG IgM Description Secretory immunoglobulin (monomer in serum, dimer in secretory form) Found in colostrum, saliva, tears, nasal fluids, and respiratory, GI, and genitourinary secretions IgA acts locally rather than through the systemic circulation. Accounts for 20% of total serum immunoglobulins Important role in preventing antigenic agents from attaching to epithelial surfaces Maternal IgA passes to an infant during breastfeeding (as do IgG and IgM to a lesser extent). Minute amounts found in serum (monomer) Predominant on surface of B lymphocytes primarily an antigen receptor Its role in the immune response is not completely clear, although it appears to be important for the maturation and differentiation of all B cells. Involved in release of vasoactive amines stored in basophils and tissue mast cell granules that cause the allergic effects It is also the antibody most stimulated during a parasitic infection. Smallest immunoglobulin (monomer) Found in all body fluids The most common immunoglobulin and represents approximately 80% of all circulating antibodies. Main antibody that crosses the placenta from the mother to the fetus during pregnancy Produced mainly in secondary immune response. The levels of IgG increase slowly during the primary (first) exposure to an antigen, but increase immediately and to a much greater extent with a second exposure Classic antibody reactions, including precipitation, agglutination, neutralization, and complement fixation Major antibacterial and antiviral antibody Largest immunoglobulin (pentamer) Usually found only in the vascular system Cannot readily cross membrane barriers because of its size Accounts for 5% of total serum immunoglobulins Dominant activity in primary or initial immune response. IgM antibody is produced first and in highest concentration during the primary exposure to an antigen. Characteristics of the Immune Response The immune response is characterized by (1) specificity (ie, reactivity is directed toward and restricted to the inducing agent, termed the antigen); (2) amplification (the ability to develop an enhanced response on repeated exposure to the same antigen); and (3) memory (the ability to recognize and mount an enhanced response against the same antigen on subsequent exposure even if the first and subsequent exposures are widely separated in time). These features distinguish the 7 immune response from other nonspecific host responses such as acute inflammation and nonimmune phagocytosis. Tolerance to Self Antigens Immunologic tolerance is specific unresponsiveness to an antigen induced by exposure of lymphocytes to that antigen. The concepts of self and nonself (foreignness) are central to immunologic reactivity. Many molecules in a host individual are antigenic (ie, they induce an immune response) if introduced into another individual but are not recognized as antigens by the host. This failure to respond to self antigens is natural tolerance, and it prevents the immune system from destroying the host's own tissues. Tolerance to self antigens is induced during embryonic development, and it also demonstrates specificity and memory. The mechanisms of natural tolerance are not fully understood, and two principal theories have been proposed to account for it. Clonal Deletion Some immunologists feel that tolerance is due to prenatal deletion of those clones of lymphocytes capable of recognizing self antigens, so that the capacity for self-recognition is in effect destroyed. Suppressor Cells Others feel that natural tolerance results from the production of specific suppressor cells (lymphocytes) that inhibit an immune response to self antigens. Specificity and Memory The specificity of the immune response is dependent on the ability of the immune system to produce an almost unlimited number of antibodies of differing specificity plus an almost equally diverse repertoire of T lymphocytes bearing specific antigen receptors on their surfaces. An antigen evokes a response from a specific B or T lymphocyte that is preprogrammed to react against it (ie, the lymphocyte bears receptors with appropriate specificity for the antigen). This receptor function is performed by immunoglobulin on B cells and by an immunoglobulin-like molecule on T cells. When challenged by an antigen, the specific lymphocyte (B or T) selectively multiplies into a clone of sensitized effector cells that can mount a highly specific response against that antigen: from B cells, plasma cells that in turn produce immunoglobulin; from T cells, cytotoxic T lymphocytes. This specific response usually has a net protective effect (immunity); occasionally, adverse reactions develop that causes tissue injury (hypersensitivity). Memory is an essential component of the immune response because it facilitates an enhanced, more effective response upon second and subsequent exposures to a particular antigen. Based on whether the immune system has been previously exposed to the antigen or not, two types of immune response can be recognized. Types of Immune Response The Primary Immune Response The primary immune response follows the first exposure to a particular antigen. Although antigen is recognized almost as soon as it is introduced into the body, several days elapse before enough immunoglobulin is produced to be detected as an increase in serum immunoglobulin levels. During this lag period, the B cells with receptors for that specific antigen undergo six to eight successive division cycles to produce a large enough clone of antibody-secreting plasma cells. IgM is the first immunoglobulin produced during the primary response; IgG production follows. The change from IgM production to formation of IgG or other immunoglobulins occurs as a normal event in B cell activation and involves switching of the heavy chain genes. Immunoglobulin levels typically peak and then decline over several days. The Secondary Immune Response 8 The secondary response follows repeat exposure to an antigen. Recognition again occurs immediately, but production of a detectable increase in serum immunoglobulins occurs much more rapidly (2–3 days) than in the primary response. IgG is the principal immunoglobulin secreted during the secondary response. In addition, peak levels are higher and the decline occurs much more slowly than in the primary response. The ability to mount a specific secondary response is a function of immunologic memory. Phases of Immune Responses Immune responses consist of sequential phases: antigen recognition, activation of lymphocytes, elimination of antigen, decline, and memory. Each phase corresponds to particular reactions of lymphocytes and other components of the immune system (see table 3). The phases Antigen recognition Tabl 3. The phases of immune responses. The effects Naive specific lymphocytes locate and recognize the antigens of microbes The lymphocyte clones that have encountered antigens undergo rapid cell division, Activation generating a large number of progeny; this process is called clonal expansion. There of are clones of effector T lymphocytes, T lymphocytes that kill infected host cells, В lymphocytes lymphocytes that secrete antibodies, Effector The effector cells and their products eliminate the microbe, often with the help of phase components of innate immunity; Most of the cells that were activated by the antigens die (apoptosis) and the dead Decline cells are rapidly cleared by phagocytes without eliciting a harmful reaction. Memory The cells that remain are memory lymphocytes Cell-Mediated Immune Response Initial Immune Response A foreign antigen penetrating the body is intercepted by antigen-presenting cells of the T-cell zone in the lymph nodes and by the Langerhans cells of the skin. It is then processed and presented to the T cells (T Helper Cells) with the aid of HLA (MHC). The HLA class II structures present only the immunogenic peptide fragment of the foreign antigen digested by the antigen-presenting cells to the T cells. The T Helper cells respond to this. The subsequent activation of the lymphocytes requires at least two types of signals. Antigen binding to the antigen receptors of lymphocytes (known as signal 1) is required to initiate all immune responses. In addition, other signals (collectively termed signal 2 or costimulator), which are provided by microbes and by innate immune responses to microbes, are needed for the activation of lymphocytes in primary immune responses. The best defined costimulators for T cells are two related proteins called B7-1 (CD80) and B7-2 (CD86), both of which are expressed on professional APCs. This requirement for microbe-induced second signals ensures that adaptive immune responses are elicited by microbes and not by harmless noninfectious antigens. The foreign antigen then binds to the lymphocyte with the appropriate receptor, emitting a mitosis signal (signal 1) for a specific family of leukocytes (clone selection). At the same time as the T cells are seeing antigen, they receive additional signals. In response to this combination of stimuli, the T helper begins to secrete cytokines. Some cytokines stimulate the proliferation of the antigen-specific T cells. Thus, the principal action of IL-2 is to stimulate proliferation of T cells; for this reason IL-2 is also called T cell growth factor. IL-2 stimulates T cells to enter the cell cycle and begin to divide. The result of this proliferation is a rapid increase in the number of antigen-specific lymphocytes, the process is called clonal expansion. A fraction of these activated lymphocytes undergo the process of differentiation, which results in the conversion of naive T cells, whose function is to recognize microbial antigens, 9 into a population of effector T cells, whose function is to eliminate microbes. Some effector T cells may remain in the lymph node and function to eradicate infected cells in the lymph node or to provide signals to В cells that promote antibody responses against the microbes. Effector Mechanisms Some effector T cells leave the lymphoid organs where they differentiated from naive T cells, enter the circulation, and migrate to any site of infection, where they can eradicate the infection. Other progeny of the T cells that have proliferated in response to antigen develop into memory T cells, which are long lived, functionally inactive, and circulate for months or years ready to rapidly respond to repeat exposures to the same microbe. As effector T cells eliminate the infectious agent, the stimuli that triggered T cell expansion and differentiation are also eliminated. As a result, the greatly expanded clone of antigen-specific lymphocytes dies (apoptosis;), thus returning the system to its basal resting state. This sequence of events is common to CD4+ T lymphocytes and CD8+ T lymphocytes. Secondary Immune Response The initial wave of proliferation also produces lymphocytes with high longevity, which as stationary stem cells have formed antigen-specific receptors on their surfaces. These are the memory cells, and they are responsible for the secondary immune response. Humoral Immunity Antibody-mediated responses are important for defense against bacteria and circulating viruses and against toxins released from bacteria. The B lymphocytes have large quantities of surface immunoglobulins. After contact with antigens (polysaccharides, drugs, pathogen toxins, or cell antigens), they transform themselves into antibody-secreting plasma cells via a series of intermediate proliferation and maturation phases. There are two types of antibody-mediated responses: T-dependent or T-independent. Antibody responses to different antigens are classified as T-dependent or T-independent, based В lymphocytes recognize and are activated by a wide variety of antigens, including proteins, polysaccharides, lipids, and small chemicals. Protein antigens are processed in antigen-presenting cells and recognized by helper T lymphocytes, which play an important role in В cell activation and are powerful inducers of heavy chain class switching and affinity maturation. (The term helper T lymphocytes came from the discovery that some T cells stimulate, or help, В lymphocytes to produce antibodies.) In the absence of T cell help, protein antigens elicit weak or no antibody responses. Therefore, protein antigens, and the antibody responses to these antigens, are called "Tdependent." Polysaccharides, lipids, and other nonprotein antigens stimulate antibody production without the involvement of helper T cells. Therefore, these nonprotein antigens, and the antibody responses to them, are called "T-independent." Initial Immune Response When an antigen enters the body, it is either transported to a lymph node or via the bloodstream to the spleen, where there are many B lymphocytes. They all can have the appropriate antibodies for a certain antigen as receptors on their surface, and after contact with the antigen they can synthesize the appropriate antibodies. B cells are excellent synthesizers of anti-protein antibodies. The recognition of antigen triggers signaling pathways that initiate В cell activation. As for T lymphocytes, В cell activation also requires second signals, many of which are produced during innate immune reactions to microbes. However, they are usually only able to do so after having enlisted the aid of T-helper cells. The intensity of the immune response hinges on how the antigens are presented. This role is assumed by antigen-presenting macrophages such as the marginal macrophages and follicular dendritic cells. They engulf the antigen, break it down by proteolysis, and present it to the T-helper cells. B lymphocytes can do the same thing. In this manner, B cells and T cells cooperate. The B 10 cells are stimulated both by the contact with the antigen and by the T-cell lymphokines, and they are either transformed into immunoblasts or form germinal centers. Formation of antibodies Initial contact with an antigen induces the B cells to form IgM, which they later carry on their surface as an antigen receptor. Later, T-cell cytokines influence the B cells. When the antibody pattern is copied, the code for the type c chain is replicated in place of the code for the heavy type l chain. This results in formation of IgG antibodies. Following this isotype switch, the antibodies are then released into the serum with bonding specificity for the original antigen. Effector Mechanisms Antibody Destruction of a Microorganism Antibodies cause the destruction of bound antigen by a variety of mechanisms. Usually, the antibody does not kill the cell, but instead coordinates the attack by turning on NK cells, activating complement, and enhancing phagocytosis. Under some circumstances, an antibody may directly inactivate an antigen. NK cell activation occurs when binding of the antigen to the Fab (specific) portion of the antibody allows an NK cell to establish connections with the Fc (nonspecific) portion, thus linking up the NK cell with the antigen. The NK cell then releases toxic chemicals that directly kill the antigen target. Complement activation. Complement is a series of molecules that, when activated, leads to the initiation of an inflammatory response and the killing of the antigen-bearing cell. Like NK cell activation, binding of the antigen to the Fab portion of the antibody allows the first molecule in the complement chain (C1) to bind nonspecifically to the Fc portion. Such binding hooks up the antigen-bearing cell with complement, ultimately leading to the destruction of the antigen-bearing cell. Phagocytic stimulation occurs similarly; when the antigen binds to the Fab portion of the antibody, this allows a phagocytic cell (usually a macrophage or neutrophil) to bind to the nonspecific Fc portion, stimulating phagocytosis of the linked antigen and the cell that bears it. Direct effects of an antibody may occur if, for example, an antibody binds to a virus at the same site the virus uses to bind to and enter a susceptible cell. This would inactivate the virus. Similarly, the antibody may bind to a bacterial toxin at the same site that the toxin would use to interact with susceptible cells. This would eliminate the effect of the toxin. Opsonization Binding of an antibody to an antigen on a bacterium causes opsonization, a change in the bacterial cell wall that renders otherwise impenetrable bacteria susceptible to phagocytosis. Complement also serves as an opsonin (an agent that may cause opsonization). Memory Cells and Secondary Immune Response Some B lymphocytes do not become antibody-secreting plasma cells after antigenic stimulation, but rather become memory cells. Memory cells circulate indefinitely in the blood and become active immediately upon repeat exposure to the antigen (a “anamnestic”response). The first time a B lymphocyte is exposed to its antigen (the primary exposure), production of antibodies against the antigen can take 2 weeks to more than 1 year, although normally antibodies to an antigen are detectable in the blood within 3 to 6 months. Because of memory cells, the next time the antigen is encountered, the antibody response occurs almost immediately. Immunoblasts form plasma cells that produce IgG. Forms of immunogenic reactivity of the organism •The immune response to the antigen is adequate (no injury) → immunity. • The immune response to the antigen is absent: - immune system is untenable due to its violation (hereditary, acquired) or exhaustion → immunodeficiency; 11 -immune system is changed after the initial exposure of antigen (decreases sensitivity to antigen) → immune tolerance; antigen is not available to the immune system → immune tolerance. •The immune response to the antigen is excessive (with signs of tissue damage): -immune system is changed after the initial exposure of antigen (increases sensitivity to antigen) → allergy, autoallergy; -amount of antigen is too much → allergy, autoallergy; -immune system suffers from a lack of time for the formation of an adequate response→ allergy, autoallergy; -immune system is made a mistake because of its defectiveness (mutations, disturbances in the system "idiotype-anti-idiotype", apoptosis defect) → autoimmune pathology; -immune system is made a mistake because the antigenic identity "foreign" and "own"→ autoimmune pathology; -immune system is made a mistake because of the disruption of immune tolerance to certain tissues"→ autoimmune pathology. Clinical Evaluation of Immune Status Major immune-mediated disorders include: 1. Immunodeficiency syndromes 2. Hypersensitivity Reactions 3. Autoimmune diseases 4. Immunologic complications of organ transplantation 5. Pathological tolerance Immune-mediated disorders may be systemic or localized to a particular organ. Suspicion of an immune disorder should trigger testing of immune function. For example, patients with chronic, recurrent, or unusual infections, may have an immune deficiency. Alternatively, persons who consistently present with localized edema and itching following contact with an object in their environment may be suspected of having a hypersensitivity response to an antigen associated with that object. Immunodeficiencies Immunodeficienсies - conditions are characterized a decrease of immunological reactivity as a result of hereditary or acquired defect of the effector mechanisms of immunity. Defects in the development and functions of the immune system result in increased susceptibility to infections and in an increased incidence of certain cancers. Immunodeficiency diseases are classified according to two characteristics: whether the defect is congenital (primary) or acquired (secondary), and the host defense system that is defective. Classification of immunodeficiencies 1. Depending on the defect of effector mechanism: - nonspecific (A dependent); - specific (B- and T-dependent). 2. By origin: -primary (hereditary); -secondary (acquired). 3. Depending on the primary lesion of cells of the immune system: -B-dependent (B-cell, humoral); -T-dependent (T-cell); -A-dependent (A-cell, phagocytic); -mixed (combined). Defects of nonspecific defense are disorders 12 complement system NK cells phagocytosis – decrease of cell number (leukopenia; agranulocytosis) and disorders of function (leukocyte adhesion defect, lazy leukocyte syn- syndrome, chronic or septic granulomatosis, Chediak–Higashi syndrome). Disturbances of acquired immune defense: Disorders of maturation Defects in both the В cell and T cell - Severe combined immunodeficiency (SCID) Block in В cell is X-linked agammaglobulinemia Block in T cell maturation -DiGeorge syndrome Defects in Lymphocyte Activation and Function Defective В lymphocytes - the X-linked hyper-IgM syndrome, common variable immunodeficiency Defective activation of T lymphocytes - Defective class II MHC expression: The bare lymphocyte syndrome Some of these diseases may result from genetic abnormalities in one or more components of the immune system; these are called congenital (or primary) immunodeficiencies. Other defects in the immune system may result from infections, nutritional abnormalities, or treatments that cause loss or inadequate function of various components of the immune system; these are called acquired (or secondary) immunodeficiencies. In this chapter we will describe the causes and pathogenesis of congenital and acquired immunodeficiencies. Among the acquired diseases, this chapter emphasizes the acquired immunodeficiency syndrome (AIDS), the disease that results from infection by the human immunodeficiency virus (HIV) and that is one of the most devastating health problems worldwide. Congenital (Primary) Immunodeficiencies Congenital immunodeficiencies are caused by genetic defects that lead to blocks in the maturation or functions of different components of the immune system. It is estimated that as many as 1 in 500 individuals in the United States and Europe suffer from congenital immune deficiencies of varying severity. All congenital immunodeficiencies share several features, their hallmark being infectious complications. However, different congenital immunodeficiency diseases may differ considerably in clinical and pathologic manifestations. Some of these disorders result in greatly increased susceptibility to infections that may be manifested early after birth and may be fatal unless the immunologic defects are corrected. Other congenital immunodeficiencies lead to mild infections and may be detected in adult life. In the following discussion, the pathogenesis of selected immunodeficiencies is summarized, several of which were mentioned in earlier chapters to illustrate the physiologic importance of various components of the immune system. Defects in Innate Immunity Abnormalities in two components of innate immunity, phagocytes and the complement system, are important causes of immunodeficiency. Chronic granulomatous disease is caused by mutations in the enzyme phagocyte oxidase, which catalyzes the production of microbicidal reactive oxygen intermediates in lysosomes. As a result, neutrophils and macrophages that phagocytose microbes are unable to kill the microbes. The immune system tries to compensate for this defective microbial killing by calling in more and more macrophages, and by activating T cells, which stimulate recruitment and activation of even more phagocytes. Therefore, collections of phagocytes accumulate around infections by intracellular microbes but the microbes cannot be destroyed effectively. These collections resemble granulomas, giving rise to the name of this disease. 13 Leukocyte adhesion deficiency is caused by mutations in genes encoding integrins or in enzymes required for the expression of ligands for selectins. Integrins and selectin ligands are involved in the adhesion of leukocytes to other cells. As a result of these mutations, blood leukocytes do not bind firmly to vascular endothelium and are not recruited normally to sites of infection. The Chediak' Higashi syndrome is an immunodeficiency disease in which the lysosomal granules of leukocytes do not function normally. The immune defect is thought to affect phagocytes and natural killer (NK) cells and is manifested by increased susceptibility to bacterial infections. Deficiencies of complement protein. C3 deficiency results in severe infections and is usually fatal. Deficiencies of C2 and C4, two components of the classical pathway of complement activation, result not in immunodeficiency but in immune complex—mediated diseases resembling lupus. A likely explanation for this association between complement deficiencies and lupus-like disease is that the classical complement pathway is involved in eliminating immune complexes that are constantly being formed during humoral immune responses. Failure to clear these immune complexes results in their deposition in tissues and immune complex disease. The observation that C2 and C4 deficiencies do not make individuals susceptible to infection suggests that the alternative pathway may be adequate for host defense. Deficiencies of complement regulatory proteins lead to excessive complement activation and not to immunodeficiencies. Defects in Lymphocyte Maturation Many congenital immunodeficiencies are the result of genetic abnormalities that cause blocks in the maturation of В lymphocytes, T lymphocytes, or both. Disorders manifesting as defects in both the В cell and T cell arms of the adaptive immune system are classified as severe combined immunodeficiency (SCID). Several different genetic abnormalities cause severe combined immunodeficiencies. About half of these cases are X-linked, affecting only male children. About 50% of cases of X-linked SCID are caused by mutations in a signaling subunit of a receptor for cytokines. This subunit is called the common γ chain (γc), because it is a component of the receptors for numerous cytokines, including interleukin (IL)-2, IL4, IL-7, IL-9, and IL-15. When the γc chain is not functional, immature lymphocytes at the pro-T cell and pro-B cell stages cannot proliferate in response to the major growth factor for these cells, namely, IL-7. Defective responses to IL-7 result in reduced survival and maturation of lymphocyte precursors. In humans, the defect affects mainly T cell maturation. The consequence of this block is a profound decrease in the numbers of mature T cells, deficient cell-mediated immunity, and defective humoral immunity because of absent T cell help (even though В cells may mature almost normally). About half the cases of autosomal SCID are caused by mutations in an enzyme called adenosine deaminase (ADA), which is involved in the breakdown of purines. Deficiency of ADA leads to the accumulation of toxic purine metabolites in cells that are actively synthesizing DNA, namely, proliferating cells. Lymphocytes, which actively proliferate during their maturation, are injured by these accumulating toxic metabolites. ADA deficiency results in a block in T cell maturation more than in В cell maturation; defective humoral immunity is largely a consequence of the lack of T cell helper function. Another important cause of autosomal SCID is mutations in an enzyme that is involved in signaling by the cytokine receptor chain. These mutations result in the same abnormalities as Xlinked SCID due to mutations, described previously. SCID is fatal in early life unless the patient's immune system is reconstituted. The most widely used treatment is bone marrow transplantation, with careful matching of donor and recipient to avoid potentially serious graft-versus-host disease. Block in В cell maturation 14 The most common clinical syndrome caused by a block in В cell maturation is X-linked agammaglobulinemia. In this disorder, В cells in the bone marrow fail to mature beyond the pre-B cell stage, resulting in a severe decrease or absence of mature В lymphocytes and serum immunoglobulins. The disease is caused by mutations in the gene encoding a kinase called the В cell tyrosine kinase (Btk), resulting in defective production or function of the enzyme. The exact role of Btk in В cell maturation is not known. The enzyme is activated by the pre-B cell receptor expressed in pre-B cells, and it is believed to participate in delivering biochemical signals that promote maturation of these cells. The gene for this enzyme is located on the X chromosome. Therefore, women who carry a mutant allele of the Btk gene on one of their X chromosomes are carriers of the disease, and male offspring who inherit the abnormal X chromosome are affected. Paradoxically, about a fourth of patients with X- linked agammaglobulinemia develop autoimmune diseases, notably arthritis. Why an immune deficiency should lead to a reaction typical of excessive or uncontrolled immune responses is not known. Block in T cell maturation Selective defects in T cell maturation are quite rare. The most frequent of these is the DiGeorge syndrome, which results from incomplete development of the thymus (and the parathyroid glands) and a failure of T cell maturation. Patients with this disease tend to improve with age, probably because the small amount of thymic tissue that does develop is able to support some T cell maturation. For selective В cell defects, patients may be given antibodies isolated from healthy donors to provide passive immunity. Immunoglobulin replacement therapy has had enormous benefit in Xlinked agammaglobulinemia. The ideal treatment for all congenital immunodeficiencies is replacement gene therapy. This treatment, however, remains a distant goal for most diseases. The most impressive results of successful gene therapy have been reported in patients with X-linked SCID, but so far very few patients have been treated, and the long-term effectiveness of the therapy is unknown. In all patients with these diseases, infections are treated with antibiotics as needed. Defects in Lymphocyte Activation and Function As understanding of the molecules involved in lymphocyte activation and function has improved, mutations and other abnormalities in these molecules that result in immunodeficiency disorders have also begun to be recognized. Many such disorders are now known. The following section describes some of the diseases in which lymphocytes mature normally but the activation and effector functions of the cells are defective. The X-linked hyper-IgM syndrome is characterized by defective В cell heavy chain class (isotype) switching, resulting in IgM being the major serum antibody, and severe deficiency of cellmediated immunity against intracellular microbes. Genetic deficiencies in the production of selected Ig isotypes are quite common; IgA deficiency is believed to affect as many as 1 in 700 individuals, but in most of these persons it causes no clinical problems. The defect causing these deficiencies is not known in the majority of cases; rarely, the deficiencies may be caused by mutations of Ig heavy chain constant region genes. Common variable immunodeficiency is a heterogeneous group of disorders that comprise the most common form of primary immunodeficiency. These disorders are characterized by poor antibody responses to infections and reduced serum levels of IgM, IgA, and often IgM. The underlying causes of common variable disease are poorly understood but include defects in В call maturation and activation as well as defects in helper T cell function. Patients suffer from recurrent infections, autoimmune disease, and lymphomas. Defective activation of T lymphocytes may result from deficient expression of major histocompatibility complex (MHC) molecules. The bare lymphocyte syndrome is a disease caused by a failure to express class II MHC molecules, as a result of mutations in the transcription factors that normally induce class II MHC expression. Recall that class II MHC molecules display peptide 15 antigens for recognition by CD4+ T cells and that this recognition is critical for maturation and activation of the T cells. The disease is manifested by a profound decrease in CD4+ T cells, because of defective maturation of these cells in the thymus and defective activation in peripheral lymphoid organs. Occasional patients have been described in whom immunodeficiency is caused by mutations in T cell signal transducing molecules, cytokines, and various receptors. Lymphocyte Abnormalities associated with Other Diseases Some systemic diseases that involve multiple organ systems, and whose major manifestations are not immunologic, may have a component of immunodeficiency. The Wiskott-Aldrich syndrome is characterized by eczema, reduced blood platelets, and immunodeficiency. It is an X-linked disease, caused by a mutation in a gene that encodes a protein that binds to various adapter molecules and cytoskeletal components in hematopoietic cells. It is believed that because of the absence of this protein, platelets and leukocytes are small, do not develop normally, and fail to migrate normally. Ataxia-telangiectasia is a disease characterized by gait abnormalities (ataxia), vascular malformations (telangiectasia), and immunodeficiency. The disease is caused by mutations in a gene whose product may be involved in DNA repair. Defects in this protein may lead to abnormal DNA repair (e.g., during recombination of antigen receptor gene segments), resulting in defective lymphocyte maturation. Acquired (Secondary) Immunodeficiencies Deficiencies of the immune system often develop because of abnormalities that are not genetic but are acquired during life. Immunoparesis of varying degree is fairly common. It occurs most often as a phenomenon in various diseases and is rarely disease (table 4). Table 4. Acquired Immunodeficiency. Mechanism The disease Rare; usually manifested as hypogammaglobulinemia in adults. Due to increased numbers of suppressor T cells. Secondary to other diseases Protein-calorie malnutrition Hypogammaglobulinemia. Iron deficiency Impaired T cell function Postinfectious (measles, leprosy) Often lymphopenia; usually transient Hodgkin's disease Impaired T cell function. Multiple myeloma Impaired immunoglobulin production Lymphoma or lymphocytic leukemia Decreased number of normal lymphocytes Advanced cancer Depressed T cell function, other unknown mechanisms Thymic neoplasms Hypogammaglobulinemia Chronic renal failure Unknown. Diabetes mellitus Unknown. Aging Decreased number of T cells in some people. Drug-induced immunodeficiency Common; caused by corticosteroids, anticancer drugs, radiotherapy, or deliberately induced immunosuppression in transplant patients. Human immunodeficiency virus (HIV) infection Reduced number of T cells, mainly helper T (AIDS) cells. Protein-calorie malnutrition results in deficiencies of virtually all components of the immune system and is a common cause of immunodeficiency in underdeveloped countries. Cancer treatment 16 with chemotherapeutic drugs and irradiation may damage proliferating cells, including bone marrow precursors and mature lymphocytes, resulting in immunodeficiency. Other treatments (e.g., to prevent graft rejection) are designed to suppress immune responses. Therefore, immunodeficiency is a frequent complication of such therapies. Acquired Immunodeficiency Syndrome (AIDS) It is a remarkable and tragic fact that although AIDS was recognized as a distinct disease entity as recently as the 1980s, in this brief period it has become one of the most devastating afflictions in the history of mankind. AIDS is caused by infection with the human immunodeficiency virus (HIV). It is estimated that there are more than 42 million HIV-infected individuals in the world, more than 21 million deaths attributable to this disease, and more than 3 million deaths annually. The infection continues to spread, especially in Africa and Asia; in some countries in Africa, more than 30% of the population has been infected with HIV. The following section describes the important features of HIV, how it infects humans, and the disease it causes. Etiology and Pathogenesis AIDS is caused by an ribonucleic acid (RNA) retrovirus called human immunodeficiency virus (HIV)—previously called human T cell lymphotropic virus type III (human T cell lymphotropic virus (HTLV III) and lymphadenopathy-associated virus (LAV). Different strains of HIV are beginning to appear. Most cases of AIDS are caused by HIV-1. A related virus, HIV-2, causes some cases of the disease. HIV-2 virus has recently been described in Africa with cases also reported elsewhere. HIV-2 produces a very similar disease. Individuals at High Risk for HIV Infection HIV infection is acquired by sexual intercourse, contaminated needles used by intravenous drug users, transplacental transfer, or transfusion of infected blood or blood products. Thus HIV infection occurs in several high-risk groups: (1) Male homosexuals and bisexuals. (2) Intravenous drug abusers account for about 15% of cases. (3) Heterosexual female contacts of male. (4) Patients transfused with blood products. The primary targets of viral attack are helper (CD4-positive) T lymphocytes. The virus uses the cell surface CD4 receptor molecules for its entry. Therefore, the major cell type that may be infected by HIV is the CD4+ T lymphocyte (T-helper), but macrophages and dendritic cells are also infected by the virus. The entry of HIV into T lymphocytes may result in (1) acute destruction of the cell, which contributes to a progressive depletion of CD4 cells; or (2) latent infection, with insertion of the proviral genome into the host DNA. Infection of humans with HIV is almost invariably associated with the appearance of anti-HIV antibodies in the serum, usually within 6 months after infection. These antibodies are not protective, and HIV viremia persists despite their presence. Detection of anti-HIV antibodies and viral isolation from the blood or infected cells are important diagnostic tools. Incubation Period The incubation period between infection and the development of AIDS has been calculated in patients infected by blood transfusion—a documented date of inoculation—to be a median of about 41/2 years. In sexually transmitted disease, it appears to be longer, ie, 8–10 years. The incubation period is shorter in young children than in adults. During the incubation period, individuals are positive for HIV antibody and may show changes in the peripheral blood lymphocytes, but they are asymptomatic. The percentage of asymptomatic HIV-positive individuals who go on to develop AIDS is unknown, but it is thought to be high. Changes in the Immune System After binding to cellular receptors, the viral membrane fuses with the host cell membrane and the virus enters the cell's cytoplasm. Here the virus is uncoated by viral protease and its RNA is released. A DNA copy of the viral RNA is synthesized by the virus's reverse transcriptase enzyme (a process that is characteristic of all retroviruses), and the DNA integrates into the host cell's DNA. 17 The integrated viral DNA is called a provirus. If the infected T cell, macrophage, or dendritic cell is activated by some extrinsic stimulus, such as another infectious microbe, the cell responds by turning on the transcription of many of its own genes and often by producing cytokines. An unfortunate consequence of this normal response is that the cytokines, and the process of cellular activation itself, may also activate the provirus, leading to production of viral RNAs and then proteins. The virus is now able to form a core structure, which migrates to the cell membrane, acquires a lipid envelope from the host, and is shed as an infectious viral particle, ready to infect another cell. It is possible that the integrated HIV provirus remains latent within infected cells for months or years, hidden from the patient's immune system and even from antiviral therapies. HIV infection leads to a decrease in the number of helper/inducer (CD4-positive) T cells in the peripheral blood. This may be accompanied by an increase in the number of suppressor/cytotoxic (CD8-positive) T cells, resulting in a decreased CD4 : CD8 ratio. These changes in the immune system lead to functional immunodeficiency. The decreased CD4:CD8 ratio is not diagnostic of HIV infection and may occur in several other immunodeficiency states. AIDS-Related Complex (ARC) Patients with ARC are HIV-positive and symptomatic but have none of the indicator diseases that are used to define AIDS. ARC patients complain of fatigue, weight loss, night sweats, and diarrhea and have superficial fungal infections of the mouth, fingernails, and toenails. The beststudied components of ARC are the lymph node abnormalities. In the early stages, infected lymph nodes show marked reactive follicular hyperplasia with characteristic histologic features - a condition called persistent generalized lymphadenopathy (PGL). HIV can be isolated from the lymph nodes of patients with PGL. At a later stage, lymph nodes show lymphocyte depletion. AIDS is the final phase of HIV infection in which the patient develops one of many opportunistic infections or neoplasms that define the disease. Among the opportunistic infections, the following are the most common: P carinii pneumonia, esophageal candidiasis, cytomegalovirus infections, atypical mycobacterial infections, toxoplasmosis of the brain, cryptosporidiosis of the intestine, herpes simplex infections, and papovavirus infection of the brain (progressive multifocal leukoencephalopathy). Kaposi's sarcoma is a malignant vascular cancer that affects the skin and many internal organs. It is the cancer whose suddenly increased incidence and appearance in a much younger age group caused AIDS to be first recognized in 1981. Since that year, these patients have been shown also to have an increased incidence of high-grade non-Hodgkin's malignant B cell lymphomas, particularly of the central nervous system. The Prospects for Prevention The main method of prevention of AIDS currently available is public education about the methods of transmission of HIV. The use of condoms and safe sex practices have been recommended as ways to decrease the risk of infection. Screening of blood donors for HIV antibody has markedly decreased the incidence of AIDS transmitted by transfusion of blood products. Health care workers, policemen, and firemen routinely take precautions to decrease the risk of becoming infected. The use of gloves, fluid-proof gowns, masks, and safe needle disposal methods should be routine safety precautions for health care workers and others at risk. The two main directions of research in AIDS are aimed at developing a vaccine that will prevent infection or a drug that will be effective in treatment. Both a vaccine and an effective drug are not apparently in the immediate future. Course and Treatment of AIDS AIDS is a disease that relentlessly and invariably progresses to death. Almost all patients are dead 5 years after diagnosis, but many die much sooner. Treated patients continue to develop additional opportunistic infections. Combination therapy with reverse transcriptase inhibitors and protease inhibitors has shown improved survival. 18