* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download PHARMACOLOGY (and other important compounds) Hey, Here is a
Survey
Document related concepts
Peptide synthesis wikipedia , lookup
Human digestive system wikipedia , lookup
Citric acid cycle wikipedia , lookup
Butyric acid wikipedia , lookup
Paracrine signalling wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Biochemistry wikipedia , lookup
Biosynthesis wikipedia , lookup
Metalloprotein wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Transcript
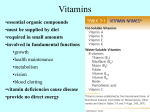
PHARMACOLOGY (and other important compounds) Hey, Here is a list of important drugs and other compounds for exam 3. I tried to bring together some of the compounds that have multiple effects (like all those pesky vitamins and hormones). It’s in alphabetical order, to help with looking things up and to distinguish compounds that have very similar names. Have a great weekend (insert sarcastic sigh here), -Pat Clements Acetaminophen - aka Tylenol, NSAID (non steroidal anti-inflammatory drug) - reversible cyclooxygenase (COX) inhibitor - mechanism unknown! Acutane - aka (13-cis-retinoic acid), a vitamin A derivative - used to treat severe acne - can cause birth defects in pregnant women ADP - released by platelet dense granules - increases platelet aggregation Albumin - Binds hemin (oxidized heme), to bring to liver - also binds bilirubin, for transport to the liver Aldosterone - mineral corticoid - produced by kidneys - increases ion absorption increases blood volume inc BP Angiotensin II - causes vasoconstriction - increased in CHD oxidized LDL activated angiotensin converting enzyme Antabuse - inhibitor of acetaldehyde dehydrogenase -alcohol met., enzyme converts acetaldehyde to AcoA - causes buildup of acetaldehyde – toxic and makes you sick. - used to give alcoholics a negative association with drinking Anti-malarial drugs - i.e. Primquine, Pamaquine - cause oxidative stress in treatment of malaria - can cause crisis for individ. w/ glucose-6-P deficiency Aspirin - NSAID (non steroidal anti-inflammatory drug) - permanent activator of cyclooxygenase I (COX1) inhibits prostaglandin synthesis -COX 1 = good, while COX 2 = bad - also inhibits platelet activity (used in high-risk patients to prevent M.I. or stroke) ATP - involved in hemostasis - ATP leads to anti-aggregation (ATP also involved in a billion other things, just not listed here Avidin - protein found in uncooked egg whites - binds biotin prevents absorption can induce deficiency Bicarbonate - (don’t forget buffer system, CO2 x-port, etc) - required by transferrin for binding Fe3+ Bile acid sequesterants- reduce the recycling of bile acids cholesterol is redirected into bile acid synthesis lowers blood cholesterol Bilirubin Biotin - product of breakdown of heme Hemin biliverdin bilirubin - scavenger of peroxyl radicals - has antioxidant activities (better than vitamin E!) - prevents the toxic effects of iron during hemolytic crisis - insoluble (because H-bonds with itself, instead of outside atoms) - conjugated (direct) = excess in liver disease / biliary obstruction - unconjugated (indirect) = indicated fever or starvation - see near the end, with the B vitamin family 2,3 Bisphosphoglycerate - reduces O2 affinity in RBCs - synthesis through glycolytic intermediates - increases in anemia Calcium - essential factor for clotting (and many other things) Canola oil - contains the least saturated fat - 6% of total fat Carbon monoxide - toxic in large quantities - 85% of CO produced in metabolism comes from the reaction: Hemin Biliverdin (enzyme= heme oxidase) - activates guanylate cyclase (significance? unclear) - possible activity as a neurotransmitter ??? - possible inhibitor of endothelial cell apoptosis ??? - possible inflammation inhibitor ??? Cholecystokinin - hormone - release is stimulated when there is fat in the duodenum - causes contraction of gallbladder, allowing for secretion of bile to help digest fats. Citrate - (dietary) promotes iron uptake, makes complexes Cortisol - a glucocorticoid - inflammatory inhibitor Collagen (role in clotting) Deferoxamine - in the subendothelial cell matrix, exposed when injured - platelets have receptor that binds collagen -aggregation around exposed collagen - collagen is highly thrombogenic - an iron chelating agent - used to remove excess iron from serum treatment for Thalessemia Divalent metals EDTA - form 2+ ions (Ca, Cu, Zn, Cd, Mn, Pb) - inhibit iron uptake - anticoagulant sometimes used for complete blood count (CBC) - sometimes causes platelets to clump not picked up by computer as platelets pseudothrombocytopenia (appears to be low platelet count) Epinephrine - In glycogen metabolism it acts in both the liver and muscle. - triggers cAMP release, activating phorphorylase kinase phos. of phosphorylase (activates) breakdown of glycogen increase in free glucose - Also activates triacylglycerol lipase (phosphorylated = active) Erythropoietin- [EPO], produced by kidney peritubular cells - works using a JAK/STAT signaling mechanism - release stimulated by hypoxia inducible factor-1 (HF-1) - increases in anemia - Stimulates RBC synthesis -suppresses apoptosis -inc synthesis globin precursors - recombinant form of EPO used in medical treatment Estradiol - An estrogen - produced by ovaries - secondary female sex characteristics Ethanol - inhibits gluconeogenesis - depletes NAD levels can’t make glucose, so increased lactate can lead to lactic acidosis (so next time you are at Doc Watson’s, have some of the food along with that pitcher, they have some good stuff!) - also raises HDL cholesterol (horray!) -but increases blood triglyecerides (Liver: ethanol acetate fatty acids triglycerides) Ezetimibe - inhibits the cholesterol transporter therefore, decreases cholesterol absorption into the body Fibrates - class of drugs to treat dyslipidemia - raises HDL, lowers TG - could raise LDL too Fibrin - produced through thrombin cleavage of fibrinogen monomers form cross links, help stabilize clotting Factor 13 also helps out products of split fibrin are anticoagulants Fibrinogen - coded by 3 genes, produced in the liver in megakaryocytes and platelets (inactive form) acute phase reactant (produced by body if injured, or gets sick) cleaved to fibrin by thrombin clot Flaxseed oil - supplement of omega-3 fatty acids - contains 7.3 gm/tablespoon of α-linolenic acid (18:3)[vegetable oil/nuts] - Sidenote: ground flaxseed is also found in Barilla Plus pasta (the yellow box), where 1 cup uncooked gives you 360 mg of omega 3 (28% RDV). The pasta also is a good source of protein (eggs and legume) and fiber. Not to mention it’s delicious! Folate - see near end, vitamin B9 Fructose - (dietary) promotes iron uptake, makes complexes Glucagon - In glycogen metabolism it acts in the liver. - triggers cAMP release, activating phorphorylase kinase phos. of phosphorylase (activates) breakdown of glycogen increase in free glucose -In diabetes, increased levels: increased lipolysis and glycogenolysis - Also inhibits triacylglycerol lipase (dephosphorylated = inactive) Heparin - prevents clotting (anticoagulant) - activates antithrombins Hepcidin - produced in liver, stimulated by IL6 release from inflammatory cells negative regulator of iron release (therefore causes sequestering) overactive in hemochromatosis inhibited in response to erythopoietic conditions (therefore increasing iron available for RBC production) - Inhibited by hypoxia inducible factor-1 (HIF-1) Homocysteine- Hcy not a standard amino acid - levels are indicative of increased CHD risk (homocysteinemia) - also associated with low folate (folate + B vitamins = lower blood hcy) Hypoxia Inducible Factor-1 (HIF-1) - heterodimer, α and βsubunits - normal conditions = hydroxylated/degraded - Hypoxia – dimer forms works as transcription factor - Increases EPO activity - Increases transferrin receptor synthesis - Decreases hepcidin synthesis (therefore, no negative regulation of iron release) iron can be released, to help with new RBC production Ibuprofen - NSAID (non steroidal anti-inflammatory drug) - permanent block of COX 2 (cyclooxygenase) from binding arachidonate decreased prostaglandin synthesis Insulin - Response to high glucose - Increases the synthesis of lipoprotein lipase increased updake of fatty acids into adipose tissue - Also activates triacylglycerol lipase (phosphorylated = active) Lead - Levulose - increases acid production in intestinal bacteria therefore, NH3 excretion in feces as ammonium MCT Oil - (medium chain triacylglyceride oil) - useful for hyperalimentation (tube feeding) - does not require pancreatic or biliary lipases for digestion useful lipid supplement for those with lipase problems poisonous, especially with heme production inactivates ALA dehydratase (so ALA in urine) inhibits ferrochelatase (adding iron to protoporphyrin) also inhibits iron transport into mitochondria Nicotinic Acid- Decrease uptake of VLDL remnants (aka niacin) - Inc LDL receptor synthesis, therefore decreasing blood cholesterol. - dyslipidemia lecture: niacin inhibits lipase of fatty acids - lowers LDL and TG, while increasing HDL - was the first dyslipidemia treatment (1950’s) Nitric Oxide - vasodilator - decreases in atherosclerosis, therefore causes blood vessel constriction (oxidized LDL inhibits nitric oxide synthetase) Omega-3 Fatty Acids - have cardioprotective effects - decreases blood triglycerides - decreases cholesterol (so lower LDL, *but also lower HDL too) - decreased platelet adhesion (prevent clots) - increases NO production (dilates blood vessels) - increases RBC membrane fluidity (prevents clots) - decreases ischemic damage to cardiac tissue Sources: Vegetable oil – oleic acid (18:1), linoleic (18:2), α-linolenic (18:3) Animal tissue – arachidonic acid (20:4) Fish – eicosapentaenoic acid (20:5), docosahexaenoic (22:6) Orlistat - aka Xenical - obesity drug - decreases pancreatic lipase activity leaves 1/3 of triglycerides undigested. (Think: remember those WOW potato chips with that compound, Olean? It was a fat that could not be digested, but people often got diarrhea from their guilty pleasures) - But if too much fat in diet side effect - steatorrhea Oxalic acid - found in rhubarb, inhibits iron uptake -**think of Dr. Dignam’s beefy brother-in-law, who hates rhubarb Phenobarbital- induces UDP-glucuronosyl transferase increased synthesis of conjugated bilirubin (soluble) - also induces secretion of bilirubin into bile - can be used to treat Type II Crigler-Najjar Syndrome Phytosterols - from diet - inhibit cholesterol uptake into micelles therefore, decreases cholesterol absorption into the body Plasma Factor 2 - produced in liver, part of intrinsic pathway - requires vitamin K for synthesis Plasma Factor 7 - Plasma Factor 8 - produced by liver - part of intrinsic clot activating system - triggers fibrinolysis plasminogen activation breaking down clots how the intrinsic pathway triggers common clotting pathway produced in liver requires vitamin K for synthesis exists normally as zymogen (inactive form) requires vitamin K for synthesis Plasma Factor 9 - produced in liver - requires vitamin K for synthesis - how the intrinsic pathway triggers common clotting pathway Plasma Factor 10 - Plasma Factor 11 - produced by liver - part of intrinsic clot activating system - triggers fibrinolysis plasminogen activation breaking down clots Plasma Factor 13 - produced in liver - assists in cross-linking in clot formation (making polymers) - deficiency = delayed bleeding Plasminogens - activated during fibrinolysis plasmins - proteases, break down clots produced in liver requires vitamin K for synthesis involved in the common clotting pathway activates thrombin (which then allows fibrinogen fibrin) Progesterone - a progestagen - made by corpus luteum - prepares uterus for pregnancy Protein C and S - anticoagulants - vitamin K dependent - trigger Questran - prevents reabsorption of cholesterol from intestines - therefore, more in feces, and lowers cholesterol - promotes bowel movements Reservatol - Found in red wine and red grape juice - decreases platelet adhesion, cardioprotective through clot formation - So if you have to be a wino, be a red wino! Serotonin - released by platelet dense granules - causes local vasoconstriction Sodium Benzoate - makes covalent products with glycine and glutamine increases nitrogen excretion in feces Sodium Phenylbutyrate - makes covalent products with glycine and glutamine increases nitrogen excretion in feces Soluble Fiber - Increase conversion of cholesterol bile acids. - Increase LDL receptor synthesis, therefore decreasing blood cholesterol. decreased LDL-C - SIDENOTE: -Soluble oat fiber can be found in some beer, especially stouts -Not only will it enhance the foamy stability and body of the brew, but it will also lower your LDL slightly less guilt for you! Statins - Inhibit cholesterol synthesis (Think: statins keep cholesterol static) i.e. Atorvasatin competitive inhibitors of HMG- Farnesylation CoA reductase decreased synthesis of isoprene compounds - Inc LDL receptor synthesis, therefore decreasing blood cholesterol. - Don’t use during pregnancy - Main effects of statins on blood vessel wall: - decreased clotting risks - decreased inflammation Sterols/stanolsTamoxifen from plants similar structure to cholesterol therefore compete for emulsification decreased cholesterol absorption fecal excretion lower LDL, while not changing HDL or TG i.e. butter substitutes Benecol and Take Control - breast cancer drug - estrogen receptor antagonist (blocks receptors) -therefore, fights estrogen dependent cancers - also has partial modulation in the uterus (hence side effects) Tannins (polyphenols) - (dietary), inhibit iron uptake - from plant material (like tea) Testosterone - produced by testes - secondary male sex characteristics Tissue Factor - secreted by endothelial cells, induced by cytokines - activates extrinsic clotting pathway (the major “git ‘er done” pathway) Tissue Plasminogen Activator (t-PA) - secreted by extrinsic system cells (endothelial) - triggers fibrinolysis plasminogen activation breaking down clots Thrombin - causes irreversible platelet aggregation clotting - potent in very small amounts (accidentally inject into patient I.V. dead) - activated by common clotting pathway (Factor 10) - catalyzes fibrinogen fibrin reaction Thrombopoeitin - stimulates megakaryocytes to produce platelets - lineage specific (targets megakaryocytes only) - produced in liver (when in doubt, most hemostasis compounds produced in the liver) Tin-protoporphyrin IX Urobilin - found in feces (bile pigment) - from the breakdown of hemoglobin - therefore, after labeling heme will be an increase in urobilin around 120 days (since increased RBC breakdown) UVB light phototherapy Vitamin A - used to treat jaundice - inhibits heme oxygenase less hemin broken down less buildup of bilirubin - used to treat babies with jaundice (buildup of bilirubin) - light used to convert from ZZ form (insoluble) to: EZ, ZE, or EE forms (soluble, can be excreted into bile) - aka retinol/retinaldehye/retinoic acid in animals - aka β-carotene in plants (vitamin A previtamin, antioxidant) though too much could cause lung cancer in smokers - fat soluble - important in retina pigments vision - can be toxic in large doses (birth defects, osteoporosis, bone thickening, enlarged liver) -**If you are ever stranded in the artic, don’t survive solely on polar bear liver. It contains extremely high vitamin A levels that can be toxic! - acutane = (13-cis-retinoic-acid) used to treat severe acne -can cause birth defects if pregnant Vitamin B1 - aka thiamine thiazole ring water soluble involved in oxidative decarboxylation rxns pyruvate dehydrogenase - α-KG dehydrogenase - branched chain keto-acid dehydrogenase ~ maple syrup disease - deficiency: Beriberi Wernicke’s encephalopathy – related to alcoholism Korsakoff’s psychosis – related to alcoholism Vitamin B2 - aka Riboflavin - water soluble - in flavin coenzymes: FMN (flavin mononucleotide) FAD (flavin adenine dinucleotide) - deficiency (rare) = oral lesions Vitamin B3 - aka niacin water soluble found as nicotinic acid/nicotinamide can be synthesized from tryptophan conenzymes: NADH (e- carrier, [O] to form ATP) NADPH (biosynthetic rxns) - deficiency: Pellegra and Hartnup’s disease - too much = liver toxicity Vitamin B5 - Vitamin B6 - aka pantothenic acid (think panto= penta= 5) water soluble part of coenzyme A (acyl x-fer rxns in TCA cycle) part of acyl carrier protein [ACP] (fatty acid synthesis) deficiency unknown (found in food, produced by some intestin bacteria) aka pyroxidine water soluble has multiple interconverted forms coenzyme: pyridoxal phosphate important in amino acid metabolism (i.e. transamination and decarboxylation rxns) - deficiency is rare (found in most foods) - too much = peripheral neuropathy Biotin - part of B vitamin family water soluble *know structure for Dr. Manning! cofactor in CO2 transfer and carboxylation reactions dietary deficiency unknown but…uncooked egg whites contain avidin -binds biotin prevents absorption induce deficiency Vitamin B9 - aka Folic acid - associated with CHD risk and elevated homocysteine (hcy) levels Folate + B6 + B12 = lower blood hcy levels - too much = will mask B12 deficiency Vitamin B12 - aka cobalamin - water soluble - similar to heme, except has central cobalt instead of iron - is a cofactor for methione synthase reaction - homocystein + 5-CH2-THF methionine + THF - methylmalonyl-CoA mutase also dependent on B12 Vitamin C - aka ascorbic acid water soluble cofactor in hydroxylases (i.e. prolyl hydroxylase) antioxidant reduces vitamin E helps protect RBC’s from oxidative damage (reducing ferric ferrous) - Also, vitamin C cannot be produced in humans via uronic acid pathway -we lack the enzyme - Also, (dietary) promotes iron uptake, makes complexes - AND…let’s not forget how it helps our pirate friends with scurvy! Vitamin D - aka calcidrol (active form) fat soluble can be synthesized in body with 7-dehydrocholesterol + sunlight acts as hormone, binding to nuclear receptor (since fat soluble) regulates calcium homeostasis increases intestinal absorption decreases kidney excretion mobilizes bone calcium - vitamin D is found in fotified milk, or naturally produced in sunlight - deficiencies: Rickets and osteomalacia - too much = retards growth, calcification of heart and kidney Vitamin E - aka α-tocopherol (most active and most abundant) - fat soluble, found in oil fraction of plant foods - antioxidant, cardioprotective -prevents peroxidation of polyunsaturated fatty acids converted to (peroxy-vitamin E) reduced by vitamin C - deficiency is not common Vitamin K - - found in green leafy vegetables / produced by intestinal bacteria fat soluble vitamin K quinol is active form dietary comes in the quinine form Epoxide cycle: regenerates active quinol form epoxide form -regeneration blocked by warfarin Vitamin K is a cofactor in carboxylation rxns i.e. carboxylation of prothrombin clotting reaction required for the synthesis of plasma factors 2, 7, 9, 10 (mnemonic 1972) (2 and 9 for intrinsic pathway) ( factor 7 for extrinsic) (factor 10 for common pathway) also required for synthesis of coagulation inhibitors Protein C and S vitamin K should be supplemented if bleeding or antibiotic use (however, fiddling with K could cause bleeding or clotting!) Von Willebrand Factor Warfarin - secreted by endothelial cells, at site of injury (clot) - “superglue” for platelets, help adhere to collagen at site - only clotting protein that is not produced in the liver! - anticoagulant - blocks the regeneration of active vitamin K quinol from epoxide form - no vitamin K can’t carboxylate prothrombin no clotting