* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 3.3mb
Survey
Document related concepts
Infection control wikipedia , lookup
DNA vaccination wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Molecular mimicry wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immune system wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adaptive immune system wikipedia , lookup
Transcript
October 12, 2004
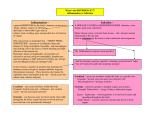
IMMUNITY
ADAPTIVE
INNATE
EFFECTOR SYSTEMS
Fc Receptors
Complement
CELL MEDIATED
HUMORAL
ANTIBODIES
ANTIGENS
RECEPTORS
EFFECTORS
Cells
Molecules
Innate immunity
First response to infection
Adaptive immunity
Triggered by persisting infection
Immunologic memory
Protects against subsequent infection
Functions of innate immunity
Initial response to infection
Frequently is sufficient to eliminate the infection
Effector mechanisms of innate immunity are often
used to eliminate pathogens in adaptive immune
response
Innate immunity stimulates adaptive immune response
and influences the nature of the adaptive response
Receptors recognize pathogen associated
molecular patterns (PAMP)
Nucleic acids unique to microbes (e.g. double stranded
RNA or unmethylated CpG DNA)
Features of proteins found in microbes
(e.g. N-formylmethionine)
Complex lipids and carbohydrates synthesized by
microbes but not mammalian cells
LPS in gram-negative bacteria
Teichoic acids in gram-positive bacteria
Mannose-rich oligosaccharides found in microbial
glycoproteins
Has evolved to recognize microbial proteins often essential
for their survival
c
Receptors of the Innate
immune response
Specificity inherited in genome
Expressed by all cells of a particular typenot clonally distributed
Trigger immediate response
Recognize a broad class of pathogens
Function
Recognize pathogen
Attract effector cells
Induce effector molecules
Contribute to innate immunity
Influence the nature of the subsequent adaptive
immune response
Trigger inflammation
Overview of the events during inflammation
The recruitment of leukocytes and extravasation of several plasma
proteins to a site of infection with activation of the leukocytes and
proteins eliminating the infectious agents
Infection
Epithelium
Barriers to infection
Mechanical
Chemical
Cells
Epithelial barriers to infection
Mechanical: Tight junction of epithelial cells
form a physical barrier
Infection
Epithelium
Epithelial barriers to infection
Chemical
Antibacterial peptides (defensins)
Enzymes (e.g. lysozyme, pepsin)
Low pH
Infection
Epithelium
Epithelial barriers to infection
Cells
Mast cells
Intraepithelial T lymphocyes
B-1 B cells
Infection
Epithelium
CD5 B cell binds capsular polysaccharide
CD 5 cell secretes IgM antipolysaccharide antibody
IgM
Phagocytes
Neutrophils
Produced and lost in large number every day
Abundant in blood
Not present in healthy tissue but recruited to
site of infection
Short-lived (6 hours) and pus contains dead and
dying neutrophils
Contain granules with anti-bacterial proteins and peptides
Can eliminate pathogens by phagocytosis
Phagocytes
Macrophages
Circulating precursors are called monocytes
Can divide at the site of infection
Longer lived than neutrophils
Phagocytes
When pathogens cross the epithelial barrier
they are recognized by phagocytes in the
subepithelial connective tissues
Trapping,engulfment and destruction by phagocytosis
Phagocytes
When pathogens cross the epithelial barrier
they are recognized by phagocytes in the
subepithelial connective tissues
Trapping,engulfment and destruction by phagocytosis
Cytokine secretion by phagocyte
Induction of co-stimulatory molecules
Antigen uptake, processing and presentation
Neutrophils and monocytes are recruited from blood to sites of
infection
Resident tissue macrophages that recognize microbes secrete
cytokines and chemokines that act on endothelial cells to produce
adhesion molecules and attract circulating neutrophils and
macrophages
Neutrophils and macrophages have receptors
that recognize microbes and stimulate their
phagocytosis and killing
Receptors that directly bind microbes
Mannose receptors
Scavenger receptors
Integrins
Pathogen Associated Molecular Patterns
Not clonal
Neutrophils and macrophages have receptors
that recognize microbes and stimulate their
phagocytosis and killing
Receptors for opsonins
FcgRs
CR1, 3 and 4
(recognize cleavage products of C3)
Triggering these receptors both stimulates
phagocytosis and activates the phagocytes
Neutrophils and macrophages have receptors
Toll-like receptors
TLR-2: zymosan from yeast,bacterial lipoproteins and
lipteichoic acid and peptidoglycan on Gram-positive
bacteria
TLR-4: LPS on Gram-negative bacteria; viral proteins
TLR-5:flagellin
TLR-9: unmethylated CpG
Activation through these receptors triggers cytokine
production and expression of co-stimulatory
molecules
Neutrophils and macrophages have receptors
Seven-transmembrane a-helical or G
protein-coupled receptors
Activation induces migration of cells from blood
through endothelium and production of microbicidal
substances
Receptors of this class recognize
Peptides containing N-formylmethionyl residues
Chemokines such as IL-8
C5a
Neutrophils and macrophages have receptors
for cytokines such as IFN-g, the major
macrophage-activating cytokine
Macrophage Possessses Many
Receptors
Activation
Engulfment
LPS
receptor
(CD14)
Scavenger
receptors
Mannose
receptor
CD11b/
CD18
TLR
TLR
Fc receptors
Cytokine Secretion
Antigen presentation
Products of Macrophages
Monokines
(Cytokines produced primarily by cells of the monocyte-macrophage
lineage)
IL-1: Activates vascular endothelium and lymphocytes; local tissue
destruction increases access of effector cells; fever
IL-6: lymphocyte activation and increased Ab production; fever,
induces acute phase proteins
IL-8: Chemotactic for leukocytes; increases access of effector cells
IL-12: Activates NK cells; induces differentiaton of CD4 T cells
into TH1
TNF-a: Activates vascular endothelium and increases vascular
permeability leading to increased entry of IgG, C’ and cells and
increased fluid drainage to lymph nodes; fever; shock
Nitrous oxide (NO), leukotrienes and platelet-activating factor
(PAF) released by macrophage also contribute to inflammation
Role of inflammation in combating infection
Deliver additional effectors molecules
and cells to site of infection
Provide a physical barrier to prevent the
spread of infection
Promote the repair of injured tissues
Combined local effects increase inflmmatory response
1. Increase in vascular diameter
lead to increased local blood volume--
heat and redness from reduced velocity of blood flow
2. Decreased blood flow
allows leukocytes to better interact with the vascular endothelium
Extravasation:
Selectins recognize certain leukocyte glycoproteins causing
lymphocytes to roll. ICAM-1 on endothelium interacts with
LFA-1 (a.k.a. CD11a;Cd18) and CR3 (Mac-1) so that leukocytes
attach firmly to the endothelium, to cross the vascular
endothelial wall and enter site of infection
3. Increase in vascular permebility
leads to local accumulation of fluid-
swelling and pain-accumulation of Igs, C’ and other blood protein in the tissue.
Combined local effects increase inflmmatory response
4. Mediators induce expression of adhesion molecules on the endothelium
neutrophils and monocytes are recruited to the site
5. Migration of leukocytes through tissues under the influence of
chemoattractant molecules.
Direct migration along a gradient of the chemokine that increases as get
nearer the site of infection.
Chemokines appear to bind to proteoglycan molecules so that they
can remain cell associated to create the gradient.
CC chemokines promote the migration of monocytes:
MCP-1, MIP-1, RANTES
CXC chemokines promote migration of neutrophils:
IL-8
An increase in vascular permeability leads to
local accumulation of fluid
Swelling (edema)
Pain
Accumulation of Igs, complement and other blood
proteins in tissue
Entry of fluid into blood at site of infection
is prevented
TNF-a
Local clots in small vessels are produced.
Fluid in tissue carries pathogen, either directly or
within a phagocytic cell, via lymph to regional lymph
nodes where an adaptive immune response is elicited
Sepsis
Infection spread to the blood stream
TNF-a
s released by macrophages
Vasodilation occurs with increased vascular
permeability leading to shock
Septic shock requires signaling through TLR-4 (recognizes
LPS) and mice (or humans) defective in TLR-4 do not
experience septic shock
Mice defective in TLR-4 are highly sensitive to LPS
containing pathogens.
TNF-a, IL-1 and IL-6 are endogenous pyrogens which
elicit acute-phase proteins
virus
IFN- a, IFN-
In hibi t pro tein synth esis and DNA
rep licatio n in virus-i nfected ce lls
In crea se MHC cl ass I expre ssio n
an d an tige n pre sentatio n in all ce lls
Activate NK cells to kil l virus -infe cte d cells
Natural Killer Cells
Function against intracellular pathogens such
as viruses
Tumor immunity
Activated by IFN-a, IFN- or IL-12
Must be able to distinguish infected from
uninfected cells
Summary - Features of Innate Immunity
Triggered by germline encoded receptors of limited diversity
No lasting immunity or memory
Elicit cytokine release by phagocytes
Induced production of acute-phase proteins
Elevate body temperature
Induce inflammation
NK cells are able to recognize infected or altered cells
B-1 B cells provide pathogen specific Abs of limited
diversity in the absence of T-cell help
Properties of substances that elicit an
adaptive immune response
Immunogen: Substance
which is capable of eliciting a
humoral or cell mediated
immune response
B cells + antigen --> effector B cells
(plasma cells) + memory B cells; Abs
produced
T cells + antigen --> effector T cells
(e.g. CTLs) + memory T cells
Antigen : a substance which
reacts with an antibody or Tcell receptor
All immunogens are
antigens but not all
antigens are immunogens
Haptens: small molecules that
are antigens (that is can react
with Ab or TcR) but which
cannot by themselves elicit an
immune response
Haptens must be linked to a carrier to elicit an immune response. Abs
are formed to both the hapten and carrier.
Small ligands often bind in a deep Ab pocket.
There is a tight fit so Ab binding can distinguish structurally
related but different haptens.
Epitope or antigenic
determinant is the part
of the immunogen that binds
Ab or the TCR
B-cell epitopes
Abs are designed to interact with the
surface of soluble antigens.
Essentially the whole surface of a globular
protein can antigenic
May be amino acids located next to each other
in sequence (sequential determinant)
Or may be amino acids that are not next to each
other in linear sequence but fold into proximity
(non-sequential or conformational)
antiserum
antiantiantianti-
inject
antibodies of different
specificity
affinity
heterogeneity
isotype
{
T-Cell Epitopes
T cells do not recognize soluble native Ag but instead recognize Ag that has been
processed and is presented in association with MHC molecules
Cross reactivity
Reaction with other than immunizing Ag
1. shared epitopes
e.g.DNP BSA and DNP- g globulin
2. structurally similar epitopes
e.g. BSA and HSA
Antigenic determinants on Abs
1. isotypic
constant region determinants that distinguish each
H and L chain class and subclass
2. allotypic
structurally different alleles of the same gene
3. idiotypic
structures unique to a variable region; may be
associated with Ag binding site
For Abs there is allelic exclusion: the products of only
one allele are present within one antibody
Isotype: separate constant region
gene. Everyone (who is normal)
has all of the genes for the
different isotypes
Allotype : multiple alleles exist in
the population for a particular
gene.
What determines if something is effective in
eliciting an immune response?
Foreignness
Must be recognized as "non-self" by
the immune system
In general the greater the degree of
foreignness, the stronger the response
Size
Best immunogens usually at least
100,000 daltons
Most (but not all) substances smaller than
5000-10000 Da are poor immunogens
What determines if something is effective in
eliciting an immune response?
Composition and Heterogeneity
Are processed and presented
Both the humoral and the cell-mediated immune response
are aided by interaction w ith T cells. Antigen presenting
cells present processed Ag in the context of MHC
molecules to activate T cells
Molecules that cannot be degraded (e.g. D-amino
acids) are poor immunogens
Treatment to increase uptake by antigen presenting
cells improves immunogenicity
cross-linking
aggregation
attachment to insoluble matrices
What determines if something is effective in
eliciting an immune response?
Genotype
MHC molecules which function in Ag presentation
B-cell and T-cell receptor genes
Genes that encode proteins involved in immune regulation
Route of injection and dose
Too little or too much can induce "tolerance"
Boosters further expand B and T cells (memory)
Administration route determines which immune organs and
cell populations will respond
Intravenous--> spleen
Subcutaneous--> lymph nodes
Adjuvants
Enhance immunogenicity of Ag
Prolong Ag persistence
Enhance co-stimulatory signal
Induce granuloma formation
Nonspecifically stimulate lymphocyte
proliferation
Granuloma: Nodule of inflammatory tissue composed of clusters of
Activated macrophages and T lymphocytes often with associated
Necrosis and fibrosis.
Alum
Aluminum potassium sulfate
Causes precipitation
Results in Ag persistance
Increased size improves phagocytosis
Local chronic inflammatory response
(granuloma -macrophage rich mass of cells)
Freund's Adjuvant
Incomplete: Ag in aqueous solution, mineral oil, and emulsifying agent
Ag is slowly released
Complete: also contains heat-killed Mycobacteria
a muramyl dipeptide of the mycobacterial
cell wall activates M
Both result in granuloma formation