* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Survey
Document related concepts
Transcript
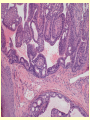
The clinical and phatologycal features of the naevus syringocystadenomatosus Floarea Sărac, Corina Bud, Simona Frăţilă University of Oradea, Faculty of Medicine and Pharmacy, Dermatology Department, Romania Case report • We describe a 38 - year-old man with syringocystadenoma papilliferum developing within a nevus sebaceus with sebaceous differentiation in an intradermal tubular apocrine component of the syringocystadenoma papilliferumThe patient reported a tumoral lesion with a history of 1 month developing in a preexisting scalp lesion that had been present from birth. The patient had no previous personal and family history of malignancy. • Local examination revealed a well delimited pink-brownish alopecic plaque measuring 2cm, in the occipital area, with a papilomatous surface. For a month a firm, hemispheric ulcerated nodular tumor of 0.5 cm diameter. General clinical examination was negative and biologic investigations were within normal values. The clinical examination suggests a neoplastic tumor (basal or squamous cell carcinoma) arising on a sebaceous nevus Jadassohn (Fig.1) • Histopathological examination confirms the diagnosis of sebaceous nevus, showing papillomatosis and important dermal sebaceous hyperplasia. One or several cystic invaginations extend downward from the epidermis. Cystic changes of the sweat glands can be observed, i.e. dilated glands and ducts with numerous villus papillary projections are lined by a glandular epithelium consisting of two rows of cells: an outer layer of small cuboidal cells with strongly basophilic nuclei Discussion • • • • • Syringocystadenoma papilliferum (SP) is a skin hamartoma, which is believed to derived from apocrine sweat glands or, less often, from eccrine sweat glands. It is an exceedingly rare neoplasm, appearing at birth or arising during infancy, around the time of puberty, or later in life. Three clinical types have been described : The linear type is usually seen on the neck or face. Lesions consist of multiple pink to red to brown, firm papules or nodules, 1-10 mm of diameter, that occur in groups. The solitary nodular form shows predilection for the trunk, especially for the shoulders, axillae and the genital area The plaque type most often presents as a hairless area in the scalp. At puberty it may become larger, nodular, verrucous or crusted, resembling nevus sebaceous. Such a lesion often develops in association with a sebaceous nevus of Jadassohn or may appear de novo without preexisting lesion. Association with hamartomas of follicular or sebaceous gland is common. In about one-third of cases, SP is associated with a nevus sebaceous. Basal cell carcinoma development has been reported in up to 10% of the cases. Squamous cell, verrucous or ductal carcinoma may also develop, but much less frequently. The diagnosis is clinically suspected and histologically confirmed. Due to the risk of malignant degeneration, prophylactic surgical excision is advisable, wherever possible. Complete surgical excision followed by detailed histological examination is the treatment of choice. Conclusions • • • • Syringocystadenoma papilliferum is a rare benign adnexal skin tumor of apocrine or eccrine glands. Syringocystadenoma papilliferum is commonly located on the head (scalp or face ) and neck region. It is frequently seen in association with other benign adnexal lesions. Transition of SP to basal cell carcinoma and, rarely, to metastatic adenocarcinoma may occur.. Our observation of syringocystadenoma arising within sebaceous nevus is important because its rarity