* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Alzheimer_Disease
Microevolution wikipedia , lookup
Gene expression profiling wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Epigenetics of human development wikipedia , lookup
Protein moonlighting wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Public health genomics wikipedia , lookup
Designer baby wikipedia , lookup
Point mutation wikipedia , lookup
Genome (book) wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
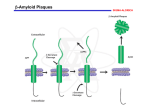
Alzheimer Disease Dr. Hazar 322-PHL 2011- 1432 The year 2006 is the centenary of the famous presentation of Alois Alzheimer which first described the neuropathology of Alzheimer’s disease (AD). Alois Alzheimer (b. 1864–d. 1915) Alzheimer described the results of his postmortem studies on a 51-year-oldfemale patient known as Auguste D., who had suffered from a progressive presenile dementia Described a relatively young patient who had developed a rapid loss of memory and had become disoriented in time and space. Alois Alzheimer As the illness progressed, she became bedridden and incontinent. She died four and a half years after the onset of illness. Post-mortem examination revealed an evenly atrophic brain with striking neurofibrillary pathology. Alzheimer also described the presence of unusual deposits in the cortex that were refractory to staining. His famous paper (Alzheimer 1907) Alzheimer’s Disease Alzheimer’s disease is the most common form of dementia. accounting for 50–60% of all cases. Dementia is a syndrome that exhibits impaired short-term and long term memory as its most prominent feature. Forgetfulness is the primary complaints of patients. Cholinergic hypothesis The cholinergic hypothesis in Alzheimer’s disease states that degeneration of cholinergic neurons in the basal forebrain nuclei causes disturbances in presynaptic cholinergic terminals in the hippocampus and neocortex, which is important for memory disturbances and other cognitive symptoms. Potentation of the activity of the central cholinergic pathway is one strategy for the symptomatic treatment of cognitive dysfunction in AD. Acetylcholinesterase inhibitors Tacrine Tacrine, the first agent approved for symptomatic treatment of mild to moderate AD Inhibit both acetylcholineesterase and butyrylcholineesterase (BuCHE) Low bioavailability, short half-life (multiple doses) Tacrine Side effect: Nausea, vomiting , diarrhea, abdominal pain. Elevation of alanine aminotransferase (ALT) levels Donepezil Second generation cholinesterase inhibitors Selective Acetylcholinestearse than (BuCHE) Completely bioavailability, once daily Side effect: cholinergic activity (nausea, diarrhea, headache) Rivastigmine Inhibit activity of both AChE and BuChE by binding to esteratic site of both enzymes and slowly dissociates. Called Pseudo-irreversible Twice daily Galantamine Inhibit AChE. allosteric modulation of nicotinic acetylcholine receptors It stimulates nicotinic receptors at a site distinct from that stimulated by acetylcholine action that does not rely on the presence of Ach Metabolized by CYP2D6 Glutamate theory Glutamate is the major excitatory neurotransmitter in the central nervous system. An over activation of glutamate receptors, and particularly of N-methyl-D-aspartate (NMDA) receptors, leads to an immediate rise in calcium ions (cell death) Memantine blocks glutamate-mediated excitotoxicity Glutamate theory Memantine was approved for the treatment of moderate and severe AD case as early as in February 2002. The basis for this approval was the result of two randomized placebo-controlled clinical studies that have showed a positive effect in a later stage of this disease (Reisberg et al. 2003). It only affects pathophysiological conditions (NMDA receptor over activation) and leaves physiological neurotransmission unchanged. The amyloid cascade hypothesis Amyloid precursor protein (APP) is a protein containing 770 amino acids Cleaved into peptides by three enzymes: alpha, beta and gamma secretase. APP is mainly formed by a two step process: If alpha secretase initially cleaves APP, alpha-soluble APP (αsAPP) is formed and eventually becomes a benign peptide. When beta secretase initially cleaves APP, it becomes beta soluble APP (β-sAPP). β -sAPP can subsequently be cleaved by gamma secretase at two different sites producing harmful peptides such as Ab 40 and Ab 42. The amyloid cascade hypothesis There are two types of beta secretase betasite APP cleaving enzyme 1,2 (BACE 1, BACE 2) Two forms of gamma secretase (presenilin 1, presenilin 2). Alzheimer and genetics Less than 10% of the AD cases are autosomal dominantly inherited and are linked to one of three different chromosomes. To date, mutations in the following genes have been described to be causative for AD presenilin-1 gene on chromosome 14, presenilin-2 gene on chromosome 1 amyloid precursor protein gene on chromosome 21. Alzheimer and genetics People that carry mutations in any one of these genes usually experience a very early onset of AD, well below 60 years of age Potential target in the future β-secretase inhibitors γ-Secretase inhibitors Metal Ions and Amyloid β proteins Aβ itself can act as a metalloprotein displaying high affinity for copper (Cu2+) and zinc (Zn2+). Interaction between amyloid and metal ions might mediate amyloid aggregation and amyloid nerve cell toxicity Ion chelators clioquinol is a hydrophobic compound that acts as a copper and zinc chelator It can readily cross the blood brain barrier Clioquinol was used decades ago as an oral antiamoebic compound, but it has been withdrawn from the market because of possible neuropathic side-effects. Phase II clinical trial Disease-related changes of the tau tau is a protein involves binding and stabilization of microtubule structure and function. The microtubule network in the cell is required for the transport of proteins. Tau, calpains and apoptosis cyclin-dependent kinase 5 (cdk5), which promote phosphorylation of tau p35 is a neuron-specific activator of cdk5 conversion of p35 into p25 by calpain-dependent proteolysis causes prolonged activation and mislocalization of cdk5. Consequently, the p25 ⁄ cdk5 kinase hyperphosphorylates tau, disrupts the cytoskeleton, and promotes apoptosis of primary neurons. Tau, calpains and apoptosis preaggregated Aβ induced the generation of a neurotoxic 17-kDa tau fragment prevented by a calpain inhibitor Prevented by anti-tau. Apolipoprotein E4 (ApoE4) Approximately 15% of the human population inherit an allele, apolipoprotein E4 (ApoE4) which can increase the risk for AD by approximately 3-fold . The APO E gene comes in three flavors, the epsilon 2, epsilon 3 and epsilon 4 alleles. Apolipoprotein E4 (ApoE4) In healthy people, the frequency of the epsilon 4 allele is 10%; in AD patients, this frequency is increased to over 40%. The existence of one or two copies of the epsilon 4 allele increases of the AD onset in a dose-dependant manner Apolipoprotein E4 (ApoE4) This allele increases cholesterol concentrations and may be responsible for augmenting the amount of Aβ or decreasing its clearance (4, 5). the formation of myelin is dependent on cholesterol, it has been suggested that cholesterol may be partially responsible for the progression of AD Statins for Alzheimer Medications which inhibit 3-hydroxy-3methylglutaryl- coenzyme A (HMG-CoA) reductase have been proven to reduce serum cholesterol, and low density lipoproteins (LDL) lovastatin, simvastatin and cerivastatin cross BBB reduce the amount of Aβ peptides by reducing cholesterol from the blood and/or the cerebrospinal fluid (CSF) Anti-inflammatory Inflammation is also occurring during the development of AD (Rogers et al. 1992; Akiyama et al. 2000). senile plaques attracting activated microglia, reactive astrocytes, cytokines and complement components (Akiyama et al. 2000) Reduction in the risk of AD associated with a chronic use of non-steroidal anti-inflammatory drugs (NSAID) ibuprofen, indomethacin and sulindac – but no other NSAID decrease the release of Aβ Treatment of behavioural signs Behavioural signs, such as aggression, psychomotor agitation, and psychosis (hallucinations and delusions) Atypical antipsychotic drugs Dementia and Alzheimer's disease Alzheimer's disease (AD) is a common age-related dementia, distinct from vascular dementia associated with brain infarction. The main pathological features of AD comprise amyloid plaques, neurofibrillary tangles and a loss of neurons (particularly cholinergic neurons of the basal forebrain). Amyloid plaques consist of the Aβ fragment of amyloid precursor protein (APP), a normal neuronal membrane protein, produced by the action of β- and γ-secretases. AD is associated with excessive Aβ formation, resulting in neurotoxicity. Familial AD (rare) results from mutations in the genes for APP, or the unrelated presenilin, both of which cause increased Aβ formation. Neurofibrillary tangles comprise aggregates of a highly phosphorylated form of a normal neuronal protein (Tau). The relationship of these structures to neurodegeneration is not known. Loss of cholinergic neurons is believed to account for much of the learning and memory deficit in AD. Anticholinesterases (tacrine, donepezil, rivastigmine) give proven, though limited, benefit in AD. Many other drugs, including putative vasodilators (dihydroergotamine), muscarinic agonists (arecoline, pilocarpine ) and cognition enhancers (piracetam, aniracetam), give no demonstrable benefit and are not officially approved. Certain anti-inflammatory drugs, and also clioquinol (a metal chelating agent), may retard neurodegeneration and are undergoing clinical evaluation.