* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Delerium
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Nicotinic agonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
NMDA receptor wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Effects of long-term benzodiazepine use wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
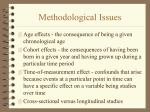
Delerium, Dementia and Insomnia 14th Feb 2006 Delerium Delirium - “to go out of the furrow” Acute Confusional State 30% of elderly medical inpatients High Mortality High Morbidity Longer hospital stays Predicts institutionalisation Often missed Poorly managed Diagnosis of Delirium Disturbance of consciousness with reduced ability to focus, sustain or shift attention Change in cognition or perceptual disturbance Short period of time (hours to days) and fluctuates Caused by the direct physiological consequences of a general medical condition, substance intoxication or substance withdrawal Differential Diagnosis Dementia - AMT / MMSE cannot distinguish - often delerium superimposed on dementia Psychotic illness Delirium vs Dementia Collateral history Acute onset, short duration Reduced consciousness Diurnal fluctuation Hallucinations common Physical precipitant Risk factors Age Dementia Severe illness Physical frailty Infection/dehydration Sensory impairment Polypharmacy Excess alcohol Psychosocial stresses Common Causes Infection Drugs Neurological Cardiac Respiratory Pain Electrolytes Endocrine/metabolic Nutritional Often multiple aetiologies Drug classes commonly implicated in Delirium Opiates Anticholinergics Sedative/hypnotics including withdrawal Dopamine agonists Antidepressants Alcohol withdrawal Corticosteroids Lithium Investigations - for all FBC Calcium Urea and electrolytes LFTs Glucose TFTs CXR ECG Blood cultures Urinalysis Investigations - when indicated ABG B12 & Folate Specific cultures Lumbar puncture CT head EEG CT Brain Scanning Not helpful if performed routinely Focal neurological signs Confusion following head injury Confusion following a fall Raised intracranial pressure EEG Limited use Delirium versus dementia Non-convulsive status epilepticus Focal intracranial lesions Management Identify and treat the underlying cause Evaluate response (monitor AMT) Optimum environment Multidisciplinary team Avoid physical restraints Avoid major tranquilizers where possible Control dangerous and disruptive behavior Psychotropic medication To prevent harm or allow evaluation and treatment Low-dose haloperidol (0.5 to 1.0 mg orally or intramuscularly) to control agitation or psychotic symptoms MOA: D2 dopamine receptor antagonist Low frequency of sedation and hypotension Onset of action is 30 to 60 minutes after parenteral administration or longer with the oral route s/e extrapyramidal; neuroleptic malignant syndrome Atypical antipsychotics - ↑ risk cerebrovascular disease Benzodiazepines Benzodiazepines (eg, lorazepam 0.5 to 1.0 mg po/IM) have a more rapid onset of action (five minutes after parenteral administration) Commonly worsen confusion and sedation Drugs of choice in cases of sedative drug and alcohol withdrawal May be useful adjuncts to neuroleptics to promote light sedation and reduce extrapyramidal side effects Alois Alzheimer 1864-1915 Dementia A general decrease in the level of cognition, especially memory Behavioral disturbance Interference with daily function and independence Dementia syndromes Alzheimer's disease (AD) 60-80% Vascular dementia (VaD) 10-20% Dementia with Lewy bodies (DLB) 10% Parkinson's disease with dementia (PDD) 5% Fronto-temporal dementia (FTD) Reversible dementias Others eg alcoholic Cholinergic Deficit Alzheimer's disease (AD) sufferers have reduced cerebral production of choline acetyl transferase & impaired cortical cholinergic function Cholinesterase inhibitors MOA: increase cholinergic transmission by inhibiting cholinesterase at the synaptic cleft Tacrine (abn LFTs), donepezil od, rivastigmine bd, and galantamine s/e: insomnia; nausea; diarrhoea; syncope; BP changes; arrhythmias Int: anticholinergics; antipsychotics Evidence of Efficacy 13 RCTs treatment for 6 months - 1 year mild, moderate or severe dementia due to Alzheimer's disease improvements in cognitive function -2.7 points (95%CI -3.0 to -2.3), in the midrange of the 70 point ADAS-Cog Scale ↑ clinical global measures Delay disease progression Conflicting data on cost effectiveness NMDA Receptor antagonists Excessive N-methyl-Daspartate (NMDA) receptor stimulation can be induced by ischemia and lead to excitotoxicity Memantine MOA: low affinity glutamate NMDA receptor antagonist Ind: Moderate to severe VaD, AD small beneficial effect at six months 1.85 ADAS-Cog points, 95% CI 0.88 to 2.83 Agents that block pathologic stimulation of NMDA receptors may protect against further damage in patients with vascular dementia s/e Dizziness, agitation, delusions Antioxidants Vitamin E Selegiline (MAO-B inhibitor) Delayed nursing home placement No evidence of benefit on cognition Selegiline and Vitamin E: Delay in Clinical Progression of Alzheimer's Disease Ginkgo Biloba Chinese herbal medicine Contains flavoglycosides potent free radical scavengers inhibit platelet-activating factor (PAF) May improve regional circulation May improve cholinergic neurotransmission Ginkgo Biloba Ginkgo Biloba (Meta-analysis of RCTs) Four studies with 212 subjects in each placebo and drug groups using EGb 761 120–240 mg/day Results: small but significant effect of 3–6 month treatment 120–240 mg of Gingko biloba extract on objective measures of cognitive function Side effects: four reports of hemorrhage Caution: in patients taking anticoagulants, antiplatelets or with bleeding diathesis lack of regulation, including variability in the dosing and contents of herbal extracts Agents with no clear benefit or evidence of harm Oestrogen/testosterone replacement NSAIDS immunization with amyloid beta peptide (6% meningoencephalitis) Behavioral symptoms Agitation Aggression Delusions Hallucinations wandering Behavioral symptoms depression and sleep disturbances depressive pseudodementia concomitant medical illness medication toxicity behavioral methods Treatment of behavioral symptoms Non-pharmacological - look for medical cause eg: constipation, urinary retention, infection, drug toxicity, pain, delirium - look for an environmental cause eg: fear of unrecognized caregivers, trigger of the behavior, sensory deprivation Treatment of behavioral symptoms Antipsychotic agents Atypical 1.6- to 1.7 fold increase in mortality compared with placebo Typical agents have problems with extrapyramidal s/e Antidepressants SSRIs preferable Benzodiazepines worsening gait, potential paradoxical agitation, and possible physical dependence Insomnia Insomnia inadequate quantity or quality of sleep difficulty initiating or maintaining sleep Non-restorative sleep/impaired daytime functioning Persistent insomnia is usually a consequence of medical, neurologic or psychiatric disease Assessment Alcohol and drug history - central nervous system stimulants - withdrawal of CNS depressant drugs Treatment of co-morbid insomnia is unlikely to be successful unless the primary cause of the disturbance is diagnosed and properly remedied Nonpharmacologic measures in conjunction with the judicious use of hypnotics Who should be prescribed hypnotics? Judicious use of hypnotics may be helpful when treating transient or short-term idiopathic or psychophysiologic insomnia Short courses to alleviate acute insomnia after causal factors have been established Some patients with insomnia benefit from long term hypnotics without evidence of tolerance or abuse Who should not? Contraindicated in pregnancy Avoid or use judiciously in patients with alcoholism or renal, hepatic, or pulmonary disease Avoid in patients with sleep apnea syndrome Avoid concomitant alcohol ingestion Avoid where high risk of abuse/dependence Avoid where altered performance may be detrimental eg driving, on-call, carers Historical agents Laudanum Bromide 19th C Chloral hydrate Clomethiazole Barbiturates Chlordiazepoxide 1960s Hypnotic agents Benzodiazepines Nonbenzodiazepine drugs Sedating antidepressants eg, amitriptyline, trazodone Antihistamines diphenhydramine Valerian – no clear evidence of effectiveness Melatonin - large doses sold over-the-counter may be associated with side effects, such as hypothermia, gynecomastia, seizures Melatonin receptor agonists - unpublished trials Benzodiazepines Low capacity to produce fatal CNS depression MOA: enhance effects of the inhibitory neurotransmitter, GABA on the GABA A receptor Sedative, hypnotic, muscle relaxant, anxiolytic, anticonvulsant, anterograde amnesia Increase total sleep time but shortened time in REM sleep Most have active metabolites with long t1/2 Adverse effects of BZDs Can get rebound insomnia on withdrawal esp with short-acting agents Residual somnolence esp with long-acting agents Tolerance Dependence and abuse ↑ falls risk in elderly Delirium in elderly Withdrawal – confusion, convulsions, DTs Up to 3 weeks after long-acting agent Paradoxical effects Anterograde amnesia Nonbenzodiazepine hypnotics nonbenzodiazepine drugs eg zolpidem, zaleplon, zopiclone also activate the benzodiazepine receptor, although they do not have a benzodiazepine structure Nonbenzodiazepine hypnotics at hypnotic doses less muscle relaxation or memory-disrupting effects ↓ tolerance and dependence Less effects on REM sleep Short half-life of ±2 hours and elimination by liver metabolism - minimal sedation the next day after administration Azapirones MOA: 5HT1A agonists Eg Buspirone Mild to moderate anxiety No tolerance or withdrawal