* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Sympathetic Drugs
Nicotinic agonist wikipedia , lookup
Orphan drug wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Pharmacogenomics wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Neuropharmacology wikipedia , lookup
Drug interaction wikipedia , lookup
Norepinephrine wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
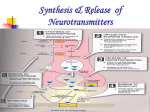
Sympathetic Drugs Stress and The Adrenal Glands Adrenal Medulla: A Modified Sympathetic Ganglion Mechanism: Norepinephrine Release and Recycling Review of Efferent Pathways: Motor and Autonomic Catechalomines: Activity • • • • • Stimulates the “fight or fight” reaction Increased plasma glucose levels Increased cardiovascular function Increased metabolic function Decreased gastrointestinal and genitourinary function Activity of Epinephrine Sympathomimetics • Drugs that partially or completely mimic the actions or norepinephrine (NE) and epinephrine (Epi). • Act either - directly on α- and/or βadrenoceptors or indirectly on presynaptic terminals, usually by causing the release of NE. • See Below • β2-Adrenoceptor Agonists – cause bronchial dilation - used for the treating asthma, prevent pre-term labor (relaxing uterine muscle). • β1-Adrenoceptor Agonists – (e.g., dobutamine) sometimes used to increase the force of heart contraction in severe lowoutput heart failure. • α1-Agonists – (e.g., phenylephrine) – used as mydriatics, decongestants. • α2-Agonists – (e.g., clonidine, methyldopa) – centrally acting hypotensive drugs. • Sympathomimetics act mainly by causing release of NE (e.g., amphetamine) have the α1/α2 selectivity of NE. • β-Adrenoceptor antagonists (β-blockers) – used to treat hypertension, angina, cardiac arrhythmias, CHF, and glaucoma. • α-Adrenoceptor antagonists (α-blockers) – limited clinical application – prazosin (selective α1antagonist – used to treat hypertension. • Adrenergic neuron blocking drugs – either deplete the nerve terminals of NE or prevent its release – used as hypotensive agents. Metabolism of Norepinephrine • • • • Reuptake Monoamine Oxidase Catechol-O-methytransferase (COMT) α1-Adrenoceptors – in several tissues (e.g., smooth muscle, salivary glands) incr IP3 and [Ca2+]in vasoconstriction or glandular secretion • α2-Adrenoceptors – on noradrenergic nerve terminals. Activation by NE inhibit AC, decr cAMP, Ca2+ channels close decr further nt release. • β-Adrenoceptor – stim AC incr [cAMP] 2nd messenger intracellular signaling physiol response. Indirectly-Acting Sympathomimetics • Transported into nerve terminals where they displace vesicular NE into the cytoplasm. Some is metabolized by MAO, but the remainder is released by carriermediated transport to activate adrenoceptors. • Amphetamines – resistant to MAO. - Peripheral actions - tachycardia, hypertension mainly caused by catecholamine release. - Dexamfetamine and methylphenidate used for hyperactive children. • Cocaine – NE reuptake inhibitor (also dopamine) – Intense central stimulant popular drug of abuse. Acute and chronic effects of Indirectly acting sympathomimetics G = Guanethidine Mechanism of action of cocaine and reserpine Directly-Acting Sympathomimetics • Effects in humans depends on their receptor specificity (α and/or β) and on the compensatory reflexes they evoke. • Epi incr bp by stim the rate and force of the heart beat (β1 effects). • Stimulation of vascular α-receptors causes vasoconstriction (viscera, skin), whereas…, • Stimulation of vascular β2-receptors vasodilation (skeletal muscle) … • And the total peripheral resistance may actually decrease. • NE has little-to-no effect on the vascular β2-receptors; thus, the α-mediated vasoconstriction is unopposed. • The resulting rise in bp reflexively slows the heart, usually overcoming the direct β1-stimulant action on the heart rate. β-Receptor-Selective Drugs • Isoprenaline – stimulates all β-receptors incr rate and force of heart beat and vasodilation full diastole and MAP, with little change in systolic pressure. • β2-Adrenoceptor Agonists – relatively selective class of drugs that produce bronchodilation – used for asthma (resistant to MAO, not uptaken into neurons). Adrenoceptor Antagonists α-Blockers • Decr artiolar and venous tone decr peripheral resistance hypotension. • Reverse the pressor effects of Epi, because its β2mediated vasodilator effects are unopposed by αmediated vasoconstriction peripheral resistance falls (Epi reversal). • Cause reflex tachycardia – this is greater with non-selective drugs that also block α2-presynaptic receptors on the heart, because the augmented release of NE further stimulates the cardiac βreceptors (e.g., prazosin). Adrenoceptor Antagonists β-Blockers • Vary in lipid solubility and cardioselectivity • All block β1-receptors and decr bp and prevent angina. • Higher Kow-drugs more rapid absorption from GIT, 1st-pass hepatic elimination more rapidly eliminated. • Also more likely to enter CNS and cause central effects (e.g., nightmares). • Cardioselectivity diminishes with higher doses. Adrenoceptor Antagonists β-Blockers (Cont’d) • Nevertheless, selective β1-blockade less peripheral vasoconstriction (cold hands and feet) and does not reduce the response to exerciseinduced hypoglycemia (stim of gluconeogenesis in liver is mediated by β2-receptors). • Cardioselective drugs may have sufficient β2activity to ppt severe bronchospasms in patients with asthma – these patients should avoid βblockers . • Some possess intrinsic sympathomimetic activity (partial agonists), but this is debatable. Catecholamine synthesis, storage, release, and reuptake pathways