* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download biochem 47 A [3-20
Evolution of metal ions in biological systems wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Adenosine triphosphate wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Mitochondrion wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Lactate dehydrogenase wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Citric acid cycle wikipedia , lookup
Biochemistry wikipedia , lookup
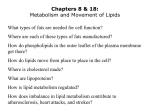
1. 2. 3. 4. 5. 6. 7. 8. Biochemistry 47 What type of mutation occurs in Duchenne muscular dystrophy? [Test Q] What is the result? [Test Q] Becker muscular dystrophy? a. Duchenne’s: X-linked, large deletion of the gene causes the absence of dystrophin=> loss of muscle function and breakdown of the sarcolemma b. Becker’s- point mutation that causes milder form of disease How does an action potential propogate to the sarcoplasmic reticulum? a. Over the sarcolemma (cell membrane), to T-tubules, then sarcoplasmic reticulum What are some characteristics of slow-twitch fibers? What color are intermediate-twitch fibers? What type are fast-twitch fibers? [3 test Qs] a. Small diameter, lots o’ mitochondria, low glycogen, found in higher concentration in tonic postural muscles b. type IIa fast-oxidative glycolitic fibers are Red like slow twitch due to high myoglobin content c. type IIb [for type I, think steak from a slow-moving cow; for type II, think cutlets from a bird flapping its 2 wings] What are some characteristics of cardiac muscle? a. Striated, involuntary, syncytial (cells connected in a network that contracts and relax synchronously), built for endurance and consistency, use aerobic metabolism with very little glycolysis capacity or glycogen How does acetylcholine cause skeletal muscle contraction at the NMJ? a. opens of Na+/K+ channels causing membrane depolarization. b. depolarization causes the dihydropyridine receptor (DHPR) in the T-tubules to bind and activate the ryanodine receptor of the sarcoplasmic recticulum c. This activates the ryanodine receptor/channel causing the release of calcium d. calcium causes a troponin-tropomyosin conformational change, ultimately exposing myosin binding sites on actin. e. myosin, using ATP, climbs along the actin to cause contraction How is cardiac muscle different? a. DHPR causes some calcium release, which activates calcium-gated ryanodine calcium channels How does nerve gas work? a. It irreversibly covalently modifies acetylcholinesterase so that muscles stay stimulated (blurred vision, bronchoconstriction, seizures, respiratory arrest, death) How is PFK-2 in skeletal muscle different from in the liver? What about cardiac PFK-2? a. Skeletal PFK-2 is not inactivated by cAMP mediated phosphorylation (lacks the regulatory site). Cardiac PFK-2 is phosphorylated to an active state by insulin. i. In liver PFK-2 is phosphorylated to an inactive state to block glycolysis and allow for gluconeogenisis 9. How are fatty acids allowed to enter muscle when energy levels drop? a. When energy drops AMP is elevated by adenylate kinase (myokinase); it activates AMP-activated protein kinase (AMP-PK) b. AMP-PK phosphorylates 2 enzymes: i. Inhibits acetyl CoA carboxylase-2 (ACC-2), slowing conversion of acetyl CoA to malonyl CoA ii. activates malonyl CoA decarboxylase (MCoADC), hastening conversion of malonyl CoA to Acetyl CoA c. High malonyl CoA normally inhibits carnitine palmitoyl transferase 1, meaning that FAs can’t enter mitochondria d. But by inhibiting ACC-2, and activating MCoADC, FAs are permitted to enter the mitochondria. e. In brief: malonyl CoA usually inhibits carnitine palmitoly transferase I (CPT-I), but when AMP levels are high, malonyl CoA is converted to acetyl CoA by malonyl CoA decarboxylase (MCoADC) and ACC-2 is also inhibited 10. What type of fuel does cardiac muscle prefer? How does glucose enter the heart m.? How do insulin and ischemia stimulate? a. Fatty acids (60-80% of metab) i. glucose and lactate (20-40%) b. GLUT 4 (90%) and GLUT 1 c. insulin and ischemia can increase # of GLUT 4s, which is additive to insulin’s translocation effect 11. How does ischemia impact the cardiac muscle? What happens when O2 is reintroduced? a. Increases rate of anaerobic glycolysis leading to acidification via lactic acid b. When O2 reintroduced, FA’s are high in blood b/c heart hasn’t been using them and now it uses them too rapidly => NADH accumulation in the mitochondria and amounts of Acetyl CoA => inhibit pyruvate dehydrogenase => increased production of lactate (further acidifies) c. As pH goes down, it becomes harder to maintain ion gradients across the sarcolemma; the heart uses its ATP to help, but then there’s less to use for contraction 12. How do pFOX inhibitors help the heart after an ischemic attack? a. Partial fatty acid oxidation (pFOX) inhibitors like ranolazine reduce the extensive FA oxidation that takes place after the ischemic episode and reduce the damage from lactate buildup 13. What 2 amino acids are used to form creatine? Where does this occur (2 steps)? What happens in the liver? How is creatinine formed and how much is formed? a. Glycine and arginine combine to form guanadoacetate in the kidney. In the liver, S-adenosyl methionine methylates the compound, forming creatine [think of insulin glargine] b. Phosphocreatine is unstable and cyclizes to creatinine at a rate proportional to muscle mass. 14. How does poststreptococcal glomerulonephritis cause an increase in serum creatinine? a. Reduces GFR by reducing blood flow to the filtration surface 15. What substance activates ACC-2 to tell the heart cell to stop taking in FAs? a. Citrate, which diffuses out slightly from the mitochondria i. malonyl CoA increases, signaling CPT-1 to reduce FA oxidation 16. What are 3 situations in which anaerobic glycolysis is especially important to produce ATP in exercise? a. At onset of exercise because phosphocreatine and stored ATP can only provide energy for 10 sec, and blood flow for oxidative resp cant increase immediately b. in muscles w/ predominantly fast twitch (IIb) fibers c. during strenuous activity when ATP demand exceeds oxidative capacity; anaerobic glycolysis is used to reduce some pyruvate to lactate and restore NAD+ 17. What 3 factors are used to control phosphorylase b and glycogen breakdown in anaerobic glycolysis of skeletal muscle? a. AMP: AMP is produced as [ADP] increases, which activates both phosphorylase b (glycogenolysis) and phosphofructokinase-1 (anaerobic glycolysis, the pyruvate doesn’t enter mitochondria) b. Ca++: allosterically binds & activates calmodulin subunit of phosphorylase b c. Epinephrine: activates adenylyl cyclase; cAMP activates PKA and PKA fully activates phosphorylase b (slower than other 2) 18. What are the potential fates of lactate generated during exercise? a. It can be used in resting skeletal muscle or cardiac muscle to produce pyruvate i. NADH/NAD+ is lower in these cases than in exercising muscle b. It can also go to liver for use in the cori cycle 19. How long can the liver continue to put out glucose? a. After 40 to 240 min the amount of glucose production from glycogen decreases b. Fatty acids are always the preferred food for muscle, except just after eating! 20. What five factors lead to FA usage over glucose? a. Availability of free FA in blood (from hormone sensitive lipase) b. Inhibition of glycolysis by FA oxidation products c. Decreased glucose transport in long term exercise (less GLUT 4) d. Lower ketone body usage (production by liver increases in exercise) e. Inactivation of acetyl CoA carboxylase (ACC-2) 21. What are 2 functions of using branched-chain a. a. in muscle? When is usage at a max? a. Can be used to produce ATP and glutamine; used to transfer ammonia to kidney, hence highest rate of BCAA usage is during acidosis 22. What are the general effects of training on muscle? a. Increases glycogen stores and increases number and size of mitochondria b. Resistance training also causes m. hypertrophy allowing more force to be generated from those muscles 23. How does a mutation in phospholamban (PLN) cause cardiomyopathies? a. The mutated PLN binds protein kinase A (PKA) blocking PKA’s ability to inactivate PLN. With PLN constantly active, it constantly inhibits SERCA 2a, weakening contraction. The heart becomes dilated by teenage years as it tries to compensate, eventually causing pulmonary congestion and left heart failure