* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Biochemistry
Magnesium transporter wikipedia , lookup
Catalytic triad wikipedia , lookup
Protein–protein interaction wikipedia , lookup
Nitrogen cycle wikipedia , lookup
Nucleic acid analogue wikipedia , lookup
Ribosomally synthesized and post-translationally modified peptides wikipedia , lookup
Two-hybrid screening wikipedia , lookup
Western blot wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Point mutation wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Metalloprotein wikipedia , lookup
Peptide synthesis wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Citric acid cycle wikipedia , lookup
Protein structure prediction wikipedia , lookup
Genetic code wikipedia , lookup
Proteolysis wikipedia , lookup
Biochemistry wikipedia , lookup
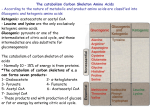
Biochemistry Protein Turnover and Amino Acid Catabolism Stryer Ch. 23 Protein Turnover • Proteins are constantly being degraded and resynthesized – Location of protein degradation • Proteins from diet are hydrolyzed in the digestive tract • Proteins within each cell are broken down within that cell in a proteasome • EXCESS AMINO ACIDS ARE NEITHER STORED NOR EXCRETED – Degradation of amino acids requires • Removal of amino group – deamination – Urea cycle • Conversion of carbon skeletons into glucose / glycogen via conversion to: – – – – • Acetyl CoA Acetoacetyl CoA Pyruvate Citric Cycle intermediate Amino Acids are classified as essential and nonessential – Essential – organism lacks the ability to synthesize these amino acids; must be acquire from diet – Nonessential – amino acids are synthesized in vivo from smaller non amino acid precursors Degradation of Dietary Proteins • Dietary Proteins are digested by general and specific proteases into free amino acids, dipeptides and tripeptides, which are absorbed into the intestine by specific transporters. – Stomach • Acidic pH = 2 • Pepsin – primary protease of stomach – Lumen of Intestine • MOST enzymes involved in digesting proteins are synthesized in the pancreas and secreted as zymogens. • Aminopeptidase – nonspecific protease that sequentially hydrolyze proteins from the amino terminal end. Degradation of Cellular Proteins • Proteins turn over within the cell. – Damaged / Mis-folded proteins are quickly destroyed • Identified by attachment of ubiquitin – Proteins that are no longer needed • Half life of protein varies from protein to protein. – Minutes, hours, days, years, decades. – Determined by N-terminal residue • R or L favors ubiquination (fast destruction) • M or P disfavors ubiquination (slow destruction; long half life) – Other signals exist. • Some diseases are due to abnormal aggregation / improper destruction of proteins. Ubiquitin (Ub) • 8.5 kd protein – 76 amino acids • Found in ALL eukaryotes • “Mark of death” – tags protein for proteolysis • Ub covalently attached to proteins – C-terminal gly of Ub – Lys of protein • ε amino group (R-group) • Ub forms polymers – polyubiquitination Ub attachment requires three enzymes • E1 or Ubiquitin-activating enzyme – Activates Ub by attachment to AMP – Links C-terminal carboxylate of Ub to sulfhydryl of E1 by thioester. • E2 or Ubiquitin-Conjugating enzyme – activated Ub transferred from sulfhydryl of E1 to sulfhydryl of E2 • E3 or ubiquitin-protein ligase – Catalyzes the transfer of Ub from E2 to target protein – Largest gene family in humans Disease linked to E3 • Parkinson disease (some forms) – Improper functioning E3 leads to abnormal accumulation of proteins. • Angelman syndrome – Severe neurological disorder (mental retardation, absence of speech, uncoordinated movement.) • Human papilloma virus (HPV) – Causes >90% of cervical carcinomas – Activates specific E3 of host leading to destruction of p53 (tumor suppressor) and other DNA repair genes. Structure of Proteasome • 26 S Large protease complex – Two 19S caps • Contains AAA class ATPase activity – ATPase associated with various activities – One 20S catalytic core • Four rings of 7 subunits each – 28 subunits total » 14 alpha (outer rings) Seven isoforms of alpha are known » 14 beta (two inner rings) Seven isoforms of beta are known. • Active sites are on beta subunits. Action of Proteasome • Hydrolyzes Ubiquinated proteins. • Proteolytic active sites are located on the beta subunits – Threonine residue acts as nucleophile to attach carbonyl of peptide bond. • Digest proteins to 7 – 9 amino acid peptides – These peptides are released from proteasome and further degraded to amino acids by cellular proteases. Bortizomib (Velcade) • Inhibitor of proteasome • Therapy for multiple myeloma Nitrogen Removal from Amino Acids • Liver is primary site of amino acid degradation – Muscle is secondary site of amino acid degradation for branched chain amino acids (e.g. L,I,V) • Two step process Removal of Amino Groups • Aminotransferase (AKA transaminases) – α amino group transferred to αketoglutarate to form glutamate – Examples • Aspartate amino transferase • Alanine amino transferase – Reversible • Also used in synthesis of amino acids. – Contain pyridoxal phosphate (PLP) as prosthetic group • Derived from pyridoxine (vitamin B6) • Glutamate dehydrogenase – Converts nitrogen of glutamate to ketoacid and free ammonium ion – Localized to mt of Liver – May use EITHER NAD+ or NADP+ – Close to equilibrium in liver • Direction of reaction determined by [substrate] or [product] • Normally driven forward by removal of ammonium Pyridoxal Phosphate (PLP) • Prosthetic group • Group transfer to or from an amino acid. • Precursor = Pyridoxine (Vitamin B6) • Deficiency = depression, confusion, convulsions. Pyridoxal Phosphate (Cont’) • Mechanism see p 659 – 660. Serine and Threonine are directly deaminated • Serine dehydratase – dehydrates and deaminates serine to produce pyruvate and ammonium • Amino group is NOT transferred to αketoglutarate • Threonine dehydratase – dehydrates then deaminates threonine to yield α-ketobutyrate and ammonium • Amino group is NOT transferred to αketoglutarate Peripheral Tissues Transport Nitrogen to the Liver Glucose – Alanine Cycle • Muscle tissue uses branched amino acids as fuel. • The nitrogen from these amino acids is transferred to alanine (through glutamate). • Alanine is carried to liver via blood stream. • Alanine is converted to pyruvate which is used to produce glucose. Excretion of Nitrogen • Terrestrial vertebrates – Ureotelic – excrete excess nitrogen as urea • Aquatic vertebrates and invertibrates – Ammoniotelic – excrete excess nitrogen as ammonium • Birds and reptiles – Uricotelic – excrete excess nitrogen as uric acid Urea Cycle Hans Krebs and Kurt Henseleit (1932) • Cycle responsible for synthesis of urea – Urea = form of nitrogen excreted in vertebrates. – Humans excrete 10 kg urea / yr. • 10 kg = 22 lbs. • Source of atoms in Urea – 1 N from free NH4+ • ammonium – C from HCO3• bicarbonate derived from hydration of CO2 – 1 N from aspartate • Carbamoyl Phosphate – intermediate in urea cycle – Synthesized from NH3 and HCO3– Carbamoyl group has a high phosphate transfer potential due to anhydride bond. Carbamoyl Phosphate Synthetase • Catalyzes the three step synthesis of carbamoyl phosphate – Bicarbonate phosphoryled by phosphate from ATP forming carboxyphosphate. – Carboxyphosphate reacts with ammonia to form carbamic acid. – Carbamic acid is phosphorylated by ATP to yield carbamoyl phosphate. • Mt matrix • 2 ATP / carbamoyl phosphate synthesized • Isozyme catalyzes the synthesis of carbamoyl phosphate for use in pyrimidine biosynthesis Carbamoyl Phosphate Synthetase • Three reaction sites – Glutamine hydrolysis site – Bicarbonate phosphorylation site – Carbamic acid phosphorylation site • Substrate channeling – Substrates pass from one active site to another active site through a channel. Is not released by enzyme. – Benefits • Increases the rate of reaction because the substrate is not “released” from the enzyme. • Protects libile substrates from degradation by hydrolysis – Carbonic acid decomposes in 1 s at ph =7. Ornithine transcarbamoylase • Catalyzes the synthesis of citrulline from ornithine and carbamoyl phosphate • Citrulline and ornithine – Amino acids NOT used in synthesis of proteins. • Mt matrix • Following synthesis, citrulline is transported to cytoplasm Argininosuccinate Synthetase • Catalyzes the condensation of citrulline with aspartate to form argininosuccinate • Cytoplasm • 1 ATP / argininosuccinate synthesized – Hydrolized to AMP and PPi Argininosuccinase • Cleaves argininosuccinate into arginine and fumarate. – Conserves carbon skeleton of aspartate in fumarate. • Cytoplasm Arginase • Hydrolyzes arginine into ornithine and urea. • Ornithine transported into mt • Urea excreted. Urea Cycle is Linked to Gluconeogenesis • Aspartate and Fumarate link Urea Cycle to Gluconeogenesis. Inherited Diseases of the Urea Cycle • Hyperammonemia – Elevated levels of ammonium (NH4+) in blood – Causes include: • lack / reduced synthesis of carbamoyl phosphate • Lack / reduced activity of the four enzymes of urea synthesis • Why is excess ammonium toxic? – Maybe the synthesis / accumulation of glutamine causes an osmotic imbalance??? Treatments of Hyperammonemias • Argininosuccinase deficiency treatment – Provide excess arginine in diet – Restrict total protein in diet • reduces amount of nitrogen to be excreted • Arginine is converted into Ornithine which reacts with Carbamyol phosphate to form citrulline. Citrulline reacts with aspartate to form arginiosuccinate which is excreted. Treatments of Hyperammonemias (cont’) • Carbamoyl phosphate synthetase or ornithine transcarbamoylase deficiency treatment – Excess nitrogen accumulates in glycine and glutamine. – Restrict protein in diet – Supplement diet with benzoate and phenylacetate • Converted into Benzoyl CoA and phenylacetate CoA – Excess nitrogen excreted as hippurate or phenylacetylglutamine Fates of Carbon Skeletons • Carbon skeletons from deaminated amino acids are converted into seven intermediates – – – – – – – Pyruvate Acetyl CoA - K Acetoacetyl CoA - K α-Ketoglutarate Succinyl CoA Fumarate Oxaloacetate • Ketogenic Amino Acids – Carbon skeletons are converted into intermediates (acetyl CoA or Acetoacetyl CoA) that can form ketone bodies or fatty acids • Glucogenic Amino Acids – Carbon skeletons are converted into intermediates that can be used to synthesize glucose. • Both – Some amino acids have carbons that end up in ketogenic and glucogenic intermediates. Fates of Carbon Skeletons Amino Acids • GLUCOGENIC BOTH NONESSENTIAL – Alanine (A, Ala) – Arginine (R, Arg)* – Asparagine (N,Asn ) – Aspartate (D, Asp) – Cysteine (C, Cys) – Glutamate (E, Glu) – Glutamine (Q, Gln) – Glycine (G, Gly) – Proline (P, Pro) – Serine (S, Ser) NONESSENTIAL – Tyrosine (Y, Tyr) ESSENTIAL ESSENTIAL (Val and His Three Methods) (Iley Trpped BOTH Phesants) – – – – – Isoleucine (I, ile) – Phenylalanine (F, Phe) – Tryptophane (W, Trp) Histidine (H, His)* Methionine (M, Met) Threonin (T, Thr) Valine (V, Val) Essential: TV FILM HW(R)K KETOGENIC NONESSENTAIL ESSENTAIL KETONES in Leu of Lysine --Leucine (L, Leu) -- Lysine (K, Lys) Updated 2014 Amino Acids • GLUCOGENIC BOTH NONESSENTIAL – A – R* – N – D – C – E – Q – G – P – S NONESSENTIAL – Y ESSENTIAL ESSENTIAL (Val and His Three Methods) (Iley Trpped BOTH Phesants) – – – – – I, Ile – F, Phe – W, Trp H, His* M, Met T, Thr V, Val Essential: TV FILM HW(R)K KETOGENIC NONESSENTAIL ESSENTAIL KETONES in Leu of Lysine --L, Leu --K, Lys Updated 2014 Definitions • Glucogenic Amino Acids – Carbon skeletons are converted into intermediates that can be used to synthesize glucose. • Ketogenic Amino Acids – Carbon skeletons are converted into intermediates (acetyl CoA or Acetoacetyl CoA) that can form ketone bodies or fatty acids – NOT substrates for glyconeogenesis • Nonessential Amino Acids – enzymes present for de novo synthesis of these amino acids • Essential Amino Acids – lacks enzymes to synthesize the amino acids. – Must be obtained from diet. Pyruvate • Amino Acids with 3 C backbone – Ala, Trp – Ser, Gly – Cys • Sulfur is converted to H2S, SCN- or SO32- – Thr • 2-amino-3-ketobutyrate intermediate Acetyl CoA Acetoacetyl CoA • Branched chain (Leu, Ile, Lys,) and aromatic amino acids (Phe, Trp, Tyr) Oxygenases are Required for Degradation of Aromatic Amino acids • Phenylalanine hydroxylase – Hydroxylates Phe to Tyr – Monooxygenase • Each atom of oxygen incorporated into different products – Tyr and water – Tetrahydrobiopterin • Electron carrier Tetrahydrobiopterin (BH4) • Electron carrier – Derived from Biopterin • Synthesized in vivo from phenylalanine – NOT a vitamin because it is synthesized by the body. • Phenylalanine hydroxylase – Synthesizes dihydrobiopterin by hydroxylating phenylalanine • Dihydrofolate reductase – Reduces dihydrobiopterin to tetrahydrobiopterin using NADPH • Dihydropteridine reductase – Reduces quinonoid dihydrobiopterin itto Tetrahydrobiopterin using NADPH Phe / Tyr • 1.Transamination • 2. p-hydroxyphenylpyruvate hydroxylase – Dioxygenase • both atom of oxygen are incorporated into the product • 3. Homogentisate oxidase – Dioxygenase • 4.Isomerization • 5. Hydrolyzed 2 1 5 4 3 Trp Converted into alanine and acetoacetate via the action of several oxidases. 2 1 4 3 α-Ketoglutarate • Amino acids with C5 skeletons – Glu • Deaminated into αKetoglutarate – Gln • Hydrolyzed to glutamate by Glutaminase – Pro • Converted to glutamate γsemialdehyde – Arg • Converted to glutamate γsemialdehyde – His • Multistep process with 4imidazolone 5-propionate intermediate Succinyl CoA • Major intermediates are common to oxidation of odd numbered fatty acids. – Propionyl CoA – Methylmalonyl CoA – Succinyl CoA • Met – Nine steps involving S-adenosylmethionine (SAM) as methyl donor. – See next slide • Val • Iso Met degradation Fumarate • Asp • Tyr – Some carbons • Phe – Some carbons Oxaloacetate • Asp – Direct deamination into Oxa • Asn – NH4+ removed by Asparaginase to form Asp which is deaminated Alcaptonuria • Archibald Garrod (1902) – First description of an inborn error of metabolism • Defective degradation of phe and tyr. • Recessive inheritance • Homogentisate accumulates and is excreted in the urine. • Harmless condition Maple Syrup Urine Disease (branched-chain ketoaciduria) • Defective / missing branchedchain dehydrogenase • Defective degradation of val, ile, leu. – Causes elevation of the level of these amino acids and the α ketoacid derivatives in vivo and in urine. • Causes Mental and Physical retardation • Patients urine smells like maple syrup. • Detection – Reaction of α ketoacid in urine with 2,4-dinitrophenylhydrazine – Mass Spec. Phenylketonuria (PKU) • Defective / missing phenylalanine hydroxylase (or the tetrahydrobiopterin cofactor) – Phenylalanine cannot be converted into tyrosine therefore phe accumulates • Autosomal recessive • Due to high [phe], reactions of Phe not found in normal individuals are prevalent in PKU patients – e.g. formation of phenylpyruvate • Phenylpyruvate in urine with FeCl3 to turn urine olive green. (this reaction lead to the initial description of PKU) • Untreated PKU leads to retardation and reduced like expectancy (death in 20 – 30s). • Treatment – Low phenylalanine diet. • Just enough phe for growth and replacement. • Prevents accumulation of phe • Must be started soon after birth. Other Diseases involving Enzymes of Amino Acid Degradation