* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Major Depressive Disorder Definition and Diagnostic Criteria Major
Drug rehabilitation wikipedia , lookup
Munchausen by Internet wikipedia , lookup
Panic disorder wikipedia , lookup
Cognitive behavioral therapy wikipedia , lookup
Depersonalization disorder wikipedia , lookup
Antisocial personality disorder wikipedia , lookup
Bipolar disorder wikipedia , lookup
Treatments for combat-related PTSD wikipedia , lookup
Schizoaffective disorder wikipedia , lookup
Spectrum disorder wikipedia , lookup
Conduct disorder wikipedia , lookup
Asperger syndrome wikipedia , lookup
Conversion disorder wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Bipolar II disorder wikipedia , lookup
Diagnosis of Asperger syndrome wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
Mental disorder wikipedia , lookup
Antidepressant wikipedia , lookup
Causes of mental disorders wikipedia , lookup
Postpartum depression wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Child psychopathology wikipedia , lookup
Epigenetics of depression wikipedia , lookup
Externalizing disorders wikipedia , lookup
Biology of depression wikipedia , lookup
Treatment of bipolar disorder wikipedia , lookup
Behavioral theories of depression wikipedia , lookup
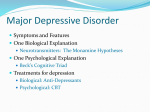
Major Depressive Disorder Definition and Diagnostic Criteria Major Depressive Disorder (MDD), also known as Unipolar Depression or Major Depression, is a disorder in which an individual’s daily functioning is impaired. The Diagnostic and Statistical Manual of Mental Disorders (2000) (DSM-IV-TR) defines MDD as having five or more of the following diagnostic features present nearly every day during a single 2 week period (DSM-TV-TR in Evans, Foa, Gur, Hendin, O’Brien, Seligman, and Walsh, 2005, p. 6): Depressed or irritable mood Diminished interest or pleasure in activities Significant weight change, or a change in appetite Change in sleep pattern Psychomotor agitation or retardation Fatigue, or loss of energy Feelings of inappropriate guilt, or hopelessness Diminished ability to concentrate Suicidal ideation and attempts If these features are met (full criteria) for Major Depressive Disorder, several specifiers are applied to the episode, as defined by the American Psychiatric Association (2000, ¶ 5) below: Mild, Moderate or Severe Without Psychotic Features, Severe with Psychotic Features, Chronic: having the full criteria for MDD met for the past 2 years Catatonic Features: immobility or over activity Melancholic Features: near complete absence of pleasure in daily activities Atypical Features: Able to be cheered up, may go through a period in which not sad, appetitite increase, hypersomnia, rejection sensitivity 1 Postpartum Onset (up to 4 weeks after childbirth): Constant concern with infant well-being, thoughts including thoughts concerned with increased risk of harm to infant Signs, Symptoms, and Risk Factors Several signs and symptoms are prevalent among those with MDD. These may vary with age group. Signs and symptoms of depression that may occur among adolescents include: decline in performance at school, withdrawal from friends, change in reactions to others comments, decrease in self-esteem, and problems with authority figures (Mental Health America, 2006). The Annenberg Foundation Trust at Sunnylands Adolescent Mental Health Initiative (Evans, Foa, Gur, Hendin, O’Brien, Seligman, and Walsh, 2005) reports that there are several risk factors associated with onset of depression in adolescent youth, including: being a female, a predisposition through having a family history of MDD, negative family interactions that may trigger depression. Prevalence Research on the prevalence of Major Depressive Disorder is slightly varied, but with similar findings. The National Alliance on Mental Illness (NAMI) cited that nearly 15 million American adults, or 5% to 8%, are affected (NAMI, 2006). Findings among children and adolescents reveal that the disorder is not limited to adulthood alone. Studies completed on the U.S. population found the incidence of MDD to be 0.9% in preschoolers, 1.9% in school-age children, and 4.7% of adolescents (Kashani and 2 Sherman, 1988 in Lewis, 2007). A study conducted in the southeastern United States on adolescents 11 to 16 year of age support previous research, finding the 1-year incidence of MDD being 3.3% (Garrison, Waller, Cuffe, et. al, 1997 in Lewis, 2007) Comorbidity of Major Depressive Disorder Major Depressive Disorder is linked to many other disorders as well. Co morbid disorders occurring along with MDD are the following: Substance-Related Disorders, Panic Disorder, Obsessive-Compulsive Disorder, Anorexia Nervosa, Bulimia Nervosa, and Borderline Personality Disorder (American Psychiatric Association, 2000, Associated Feature and Disorders, ¶ 1). Suicidal ideation is common among individuals with Major Depressive Disorder as well. The DSM-IV-TR (American Psychiatric Association, 2000) reports that up to 15% of those with MDD die from suicide. The National Institute of Mental Health believes that “30 to 70% of suicides completed are by individuals with major depression” (Poling, 1997, p. 17). Treatment A variety of treatments currently exists for Major Depressive Disorder, including (NAMI, 2008): Medications: o Selective Serotonin Reuptake Inhibitors (SSRIs) o Serotonin and norepinephrine reuptake inhibitors (SNRIs) o Tricyclic antidepressants (TCAs) o Monoamine Oxidase Inhibitors (MAOIs) 3 Psychotherapy o Cognitive Behavioral Therapy (CBT) o Interpersonal Therapy (IPT Electroconvulsive Therapy (ECT) Within the use of medications, the initial effect of the antidepressants may not take place until two to four weeks into the start of treatment. In addition, it may take up to 12 weeks for the full effect to be felt (NAMI, 2008). Cognitive Behavioral Therapy (CBT) is a treatment in which negative thoughts are the source for the depression, and these are replaced with positive thoughts. Interpersonal Therapy takes the treatment and links it to other individuals, looking at improving the personal relationships that may contribute to the depression (NAMI, 2008). In the most severe cases, Electroconvulsive Therapy (ECT) is used when other options have proven non-effective. With the concern of ECT treatment among children and adolescents, this is a treatment under question due to the safety among children and adolescents receiving it (Lewis, 2007). Any of the previous treatments may be used for Major Depressive Disorder, whether it is singularly, or in combination with another and have proven effective according the National Alliance on Mental Illness(NAMI). However, NAMI reports that, “Research demonstrates that a combination of medication and psychotherapy is often the most effective treatment” (NAMI, 2008, p. 10). 4 Within the population of children and adolescents with depression, it is suggested that a biopsychosocial approach is used (Lewis, 2007). According to Lewis (2007, p. 774), this approach incorporates medication, therapy, and includes not only the individual but the family as well. In addition to previous therapies mentioned, play therapy, the life stress model, and parent training may be included. Play therapy is most often used among the younger population and provides a nonverbal interaction that may show life stressors (Lewis, 2007, p. 774). The life stress model is a therapy in which children and adolescents either rid themselves of, or learn how to cope with life stressors (Lewis, 2007, p. 775). Lastly, parent training is incorporated in order teach parents how to demonstrate appropriate behaviors, and how to react to their child’s behaviors (Lewis, 2007, p. 775). Educational Information In order to educate individuals about what Major Depressive Disorder and depression are, it is important to look at what they are not. In Living with Depression: A Survival Manual for Families (Third Edition), Kim Poling, L.S.W., reports many current myths people have about depression (Poling, 1997, p. 7-9). The following are myths she describes: Myth Depression will “go away on its own” “Everyone feels this way” Reality Depression that goes untreated can last many years. Sadness is a temporary reaction, depression is persistent 5 Even though someone may talk about suicidal thoughts, they would never attempt suicide. If depression is mild, suicide is uncommon. Children and adolescents cannot suffer from depression. Suicidal threats should not be ignored. Suicidal ideation may occur at any level of diagnosis Depression does occur in children and adolescents and may impair them in daily functioning. Conclusion Major Depressive Disorder may occur at any age, to anyone. A myriad of treatment is widely available, depending on the level of the disorder and the symptoms, as well as age. Education is the key, learning the truth about the disorder and dispelling myths. It is imperative to know the signs and symptoms of MDD, as well as what actions to take if someone is demonstrating them. 6 References American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders, fourth edition (text revision). Washington, DC: Author. Evans, D. L., Foa, E. B., Gur, R. E., Hendin, H., O’Brien, C. P., Seligman, M. E. P., & Walsh, B. T. (2005). Treating and preventing adolescent mental health disorders. New York City: Oxford University Press. Retrieved September 5, 2008, from http://amhi-treatingpreventing.oup.com/anbrg/public/content/ mentalhealth/9780195173642/toc.html Garrison, C. Z., Waller, J. L., Cuffe, S. P., et. al. (1997). Incidence of major depressive disorder and dysthymia in young adults. Journal of Child and Adolescent Psychopharmacology, 36, 458-465. Kashani, J. H. & Sherman, D. D. (1998). Childhood depression: Epidemiology, etiological models, and treatment implication. Integrated Psychiatry, 6, 1-8. Lewis, M. (2007). Child and adolescent psychiatry: A comprehensive textbook (4th ed.). Philadelphia: Lippincott Williams & Wilkins. Retrieved September 4, 2008, from http://hsls.pitt.edu Mental Health America (2006). Factsheet: Depression in Teens. Retrieved September 9, 2008, from http://www.mentalhealthamerica.net/go/information/getinfo/depression/depression-in-teens 7 National Alliance on Mental Illness (2006). Major Depression. Retrieved September 9, 2008, from http://www.nami.org/Template.cfm?Section=By_Illness&template=/ ContentManagement/ContentDisplay.cfm&ContentID=7725 National Alliance on Mental Illness (2008). Understanding Major Depression and recovery: What you need to know about this medical illness. Retrieved September 5, 2008, from http://www.nami.org/Template.cfm?Section=By_Illness&template=/ContentMan agement/ContentDisplay.cfm&ContentID=61084 Poling, K. (1997). Living with Depression: A survival manual for families (3rd ed.). Pittsburgh: University of Pittsburgh, Services for Teens at Risk (STAR-Center). 8