* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download MSIV personality disorders v 2012_Dr D Mercer
Gender dysphoria wikipedia , lookup
Mental status examination wikipedia , lookup
Bipolar II disorder wikipedia , lookup
History of psychiatric institutions wikipedia , lookup
Excoriation disorder wikipedia , lookup
Bipolar disorder wikipedia , lookup
Panic disorder wikipedia , lookup
Substance use disorder wikipedia , lookup
Moral treatment wikipedia , lookup
Separation anxiety disorder wikipedia , lookup
Autism spectrum wikipedia , lookup
Depersonalization disorder wikipedia , lookup
Schizoaffective disorder wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
Obsessive–compulsive personality disorder wikipedia , lookup
Conversion disorder wikipedia , lookup
Abnormal psychology wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
Mental disorder wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Causes of mental disorders wikipedia , lookup
Borderline personality disorder wikipedia , lookup
Conduct disorder wikipedia , lookup
Asperger syndrome wikipedia , lookup
History of psychiatry wikipedia , lookup
Spectrum disorder wikipedia , lookup
Child psychopathology wikipedia , lookup
Personality disorder wikipedia , lookup
History of mental disorders wikipedia , lookup
Classification of mental disorders wikipedia , lookup
Pyotr Gannushkin wikipedia , lookup
Schizoid personality disorder wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
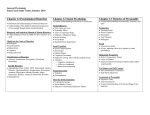
Dissociative identity disorder wikipedia , lookup
Personality Disorders Deanna Mercer MD FRCPC MSIV March 21 2012 [email protected] Objectives • Describe personality disorders: criteria, clusters and core symptoms • Axis I and Axis II comorbidity • Understanding self injurious behaviour • Borderline Personality Disorder: diagnosis and treatment • Antisocial Personality Disorder: diagnosis and basic treatment 5296 Describe the general diagnostic criteria for a PD. 5297 State the classification of PD in three clusters. 5298 Describe the main enduring pattern of each PD type. 5299 Explain the clinical relevance of comorbity of Axis I and Axis II disorders. 5300 Describe the mental disorders associated with self‐injurious behaviors (SIB) 5301 List the biological, demographic, economic, social and developmental factors associated with SIB. 5302 Describe the pertinent factors in the recognition of the potential of SIB. 5303 List criteria for borderline personality disorder (BPD). 5304 Describe common psychiatric comorbidities asociated with BPD. 5305 Describe a treatment approach to BPD including use of hospitalization, outpatient care, pharmacological treatment and psychotherapy Good References • Disordered Personalities • Field Guide to Disordered Personalities Dave Robinson MD Rapid Psychler Press Personality Disorders Introduction Criteria, clusters and core symptoms Personality What is it? How do you get one? Personality: Definition • An individual’s characteristic pattern of response to his/her environment. • Includes: how one thinks, feels, acts and relates to others. Personality: Etiology Temperament X Environment Time Disorder • Leads to clinically significant distress or impairment in functioning DSM IV general criteria for personality disorder • Enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture • cognition, affectivity, interpersonal functioning and impulse control • Pattern is inflexible and pervasive • Leads to clinically significant distress or impairment in functioning • Not better accounted for by other mental disorder PD’s are Ego Syntonic • Ego Syntonic: Individual experiences significant distress, but does not feel that their thoughts, emotions or behaviours are the source of their distress • external locus of control • Ego Dystonic: Individual sees their disorder as arising from their own thoughts, emotions or behaviours • internal locus of control Epidemiology DSM “informed speculation” –Any PD 9% –Most PD’s 1-2 % –No sex differences in any PD • In clinical populations 50 -80% • Torgersen 2001 Norway, • Lezenweger 2007 National Comorbidity Survey Replication Prognosis • All tend to improve over time (years) • Cluster B the most • Schizotypal, Borderline and Avoidant have the greatest functional impairment • Narcissistic, Histrionic, Obsessive Compulsive personality disorders have the least functional impairment Why make a diagnosis of Personality Disorder? Why make a PD diagnosis ? • Axis I with PD • More impaired, more chronicity • Overall poorer response to treatment requiring more intensive and prolonged care • Certain PD’s (BPD, ASPD, Schizotypal PD) have specific treatments or are contraindications for certain treatments Personality Disorders: Clusters • Cluster A: odd Schizoid, schizotypal, paranoid • Cluster B: dramatic Borderline, histrionic, narcissistic, antisocial • Cluster C: anxious Obsessive compulsive, dependent, avoidant Cluster A Personality Disorders Schizoid PD Schizotypal PD Paranoid PD Pictures of famous People with Schizoid Personality Disorder Schizoid Personality Disorder • “A pervasive pattern of detachment from social relationships and a restricted range of expression of emotions in interpersonal settings beginning by early adulthood and present in a variety of settings..” • “DR” • Detached from relationships • Restricted range of emotional expression Schizotypal Personality Disorder Schizotypal PD A pervasive pattern of social and interpersonal deficits marked by acute discomfort with, and reduced capacity for, close relationships as well as by cognitive or perceptual distortions and eccentricities of behavior, beginning by early adulthood and present in a variety of settings “ACE” • Acute discomfort in close relationships: • Cognitive and perceptual distortions: • paranoia rather than fear of judgment odd beliefs, unusual perceptions, suspiciousness,paranoia, odd speech Eccentric Behaviours Paranoid Personality Disorder Paranoid PD • “A pervasive distrust and suspiciousness of others such that their motives are interpreted as malevolent, beginning by early adulthood and present in a variety of settings…” • • • • “DSMM” Distrusts others, Suspiciousness others Motives are interpreted as Malevolent How to Remember Cluster A • Schizoid: looks like negative symptoms of scz • Schizotypal: looks like positive symptoms of scz (but not full blown psychosis) • Paranoid PD: looks like delusional disorder, paranoid type ( but no full blown delusions and more pervasive suspiciousness) All cluster A have: • Increased risk of brief psychotic episodes • Genetic link to schizophrenia: – Schizotypal>schizoid>ppd • Few relationships – Schizoid: if any close relationship it is with 1˚ family – Schizotypal: lacks close friends except 1˚ family – Paranoid: few friends with similar beliefs • Risk of developing scz – Schizotypal: 10-20% Cluster B Histrionic PD Antisocial PD Narcissistic PD Borderline PD Histrionic Personality Disorder Histrionic PD • “A pervasive pattern of excessive emotionality and attention seeking, beginning by early adulthood and present in a variety of contexts…” • “theatrical” • Intense but shallow emotions • Craves being the centre of attention Antisocial Personality Disorder Antisocial PD • “Pervasive pattern of disregard for and violation of the rights of others occurring since age 15 years / must be at least age 18 years” • • • • • • • Repeated lawbreaking Deceitfulness Impulsivity Irritability and aggressiveness Reckless disregard for safety of self or others Consistent irresponsibility Lack of remorse ASPD epidemiology • DSMIV tr 1% females 3% males • New community based studies 1% M=F ASPD prognosis • Highest risk of ASPD: early onset conduct (before age 10) and ADHD • 75% of conduct disorder resolves by adulthood • Prognosis better if has some connection to a group • ASPD > Sociopathy ( Tony Soprano) > Psychopath (Ken Lay) • Decrease impulsivity and criminal behavior, but continue to be difficult people (poor spouses, parents, employees) Treatment Rarely seek help for distress caused by their actions Most common reasons for psychiatric contact: detox, seeking meds with a street value, notes for missing work, assessments to avoid criminal responsibility, military service, work that they see as undesirable Psychotherapy usually contraindicated, particularly psychopathy Stay respectful, but avoid emotional investment in patient ◦ Confront denial and minimization ◦ Restrict focus to possible outcomes of antisocial behaviour ◦ Help to find healthier alternatives to acting out Psychopathy http://www.youtube.com/watch?v=s5h EiANG4Uk Narcissistic Personality Disorder Narcissistic PD “ A pervasive pattern of grandiosity (in fantasy or behaviour) need for admiration, and lack of empathy, beginning by early adulthood and present in a variety of contexts” • “AGE” – need for Admiration, – Grandiosity (fantasy or behaviour) – lack of Empathy for others Borderline Personality Disorder Borderline PD “ A pervasive pattern of instability of interpersonal relationships, self-image and affects, and marked impulsivity beginning by early adulthood and present in a variety of contexts…” Cluster C” anxious” Obsessive Compulsive Avoidant Dependent Obsessive Compulsive Personality Disorder OCPD http://www.youtube.com/watch?v= T-GKovedEy4&feature=related OCPD • “A pervasive pattern of preoccupation with orderliness, perfectionism, and mental and interpersonal control, at the expense of flexibility, openness, and efficiency, beginning by early adulthood and present in a variety of contexts..” • “OCP” • Orderliness • Perfectionism • Control : mental and interpersonal • *Most do not have OCD (only 30%) • Adolescents with strong OCPD traits can grow out of the diagnosis Avoidant Personality Disorder Avoidant PD “A pervasive pattern of social inhibition, feelings of inadequacy, and hypersensitivity to negative evaluation, beginning by early adulthood and present in a variety of contexts” • similar to social phobia, but more pervasive Dependent PD • A pervasive and excessive need to be taken care of that leads to submissive and clinging behaviour and fears of separation, beginning by early adulthood and present in a variety of contexts..” • • • • “Dependent on relationships” Difficulty making everyday decisions without a lot of advice, reassurance from others unable to disagree with others because fears loss of support, will do things that are unpleasant, degrading to maintain support If person’s fear of retribution realistic (abusive spouse) do not make diagnosis Borderline Personality Disorder BPD DSMIV • A pervasive pattern of instability of interpersonal relationships, self-image and affects, and marked impulsivity • Affective: emotional lability, problems with anger • Relationships: chaotic, idealizing/devaluing, fears of abandonment “I hate you, don’t leave me” • Behaviours: suicide and self harm, impulsive (sex, A&D, binge eating, driving fast, promiscuity) • Cognitive: emptiness, unstable sense of self, mild psychotic symptoms under stress, dissociation Self Harm / SIB • Behaviours that inflict harm to one’s body without the obvious intention of committing suicide • 1-4 % general population • chronic/severe SH 1% • Teens 5- 13 %, college age 17- 35% • Age of onset: 14 - 24 • majority (75%) <10 times • Increasing in teens • Increased risk of suicide behaviours • F=M • abrading/scratching> cutting, banging> biting, burning Risk Factors • Social: Low SES, adverse events during childhood (abuse and trauma) • Biological: ↓ serotonin, impulsivity • Psychiatric Disorders (90%) : Personality disorders (BPD -75%), depression, pervasive developmental delay, dissociative identity disorder, eating disorders, • Alcohol and substance abuse are common SIB • Situational Risk factors: recent negative life events • Reasons: – relief from intense painful emotions – self punishment – to get significant others to respond Assessing for SIB • Suspect in teens and young adults who are presenting with psychological distress • Important to recognize that SIB is usually an attempt to reduce emotional distress • Best way to solve the problem is to look for a solution to the event that caused the emotional distress SIB: intervention • Start by validating that the prompting problem and the distress are real and that it makes sense to want to reduce emotional pain • Highlight that while SH does reduce emotional pain in the short term, it is not a great way to solve the problem that got the distress going in the long run • Invite the person to look at other methods of problem solving Objective # 5305 Describe a treatment approach to BPD including use of hospitalization, outpatient care, pharmacological treatment and psychotherapy Bio-Social Theory EMOTION DYSREGULATION Emotionally Vulnerable individual Invalidating Environment Linehan 1993 BPD: prognosis • With primarily OPD treatment 75% of patients with BPD no longer meet criteria after 6 years • 75% have history of suicide and self harm attempts. 5 - 10% die by suicide • Worst prognostic factor: concurrent substance dependence • Best prognostic factor: GAF at time of diagnosis BPD: Comorbidity • Mood disorders : depression 50%, dysthymia 70%. At time of admission 90% MDE • Bipolar I,II: 18% • Eating Disorders(An, BN, obesity) : 50% • Anxiety Disorders: 90% • Substance Use Disorders: 60% • Narcissistic PD, antisocial PD: 50% Treatment of BPD • Mainstay of treatment is outpatient care and psychotherapy – BPD patients are exquisitely sensitive to what happens in their environment – treatment has to help them find ways to : 1.Solve problems causing painful emotions 2.Feel better 3.Tolerate both the situation and how they feel about it without making the situation worse BPD treatment: Psychotherapy • All empirically based psychotherapies (DBT, MBT, TFP, Schema focused) – Focus of treatment is to establish connection between actions and feelings – Therapists manage, pay careful attention to countertransference. – Therapist has ongoing discussion with colleagues or easy access to consultation – Here and now focus BPD: Hospitalization • Admission indicated: – After a serious suicide attempt – Psychosis/severe disorganization • May be indicated – loss of significant social support – Worsening depression, substance abuse • Caution when – Hospital has not been helpful or has made person worse Links 2010 BPD: Meds • Adjunct to psychotherapy, limit expectations (yours and your patient’s!) • Concurrent MDE: SSRI’s, Effexor • Affective lability: mood stabilizers – Lamotrigine, Aripiprazole • Insomnia, agitation, brief psychotic symptoms – low dose quetiapine, olanzapine • Avoid: benzodiazepines, meds that are dangerous in overdose (lithium, tricyclics)